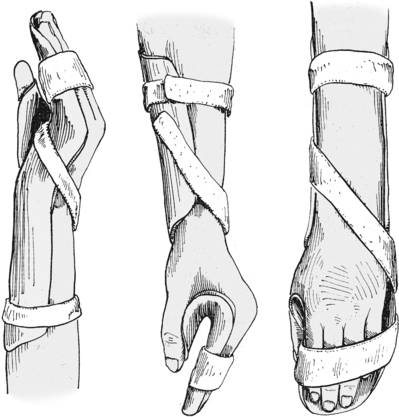
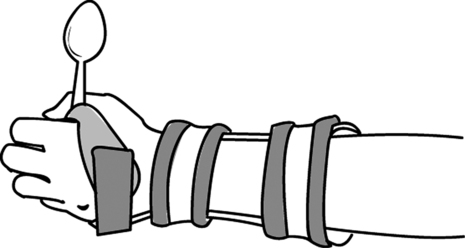
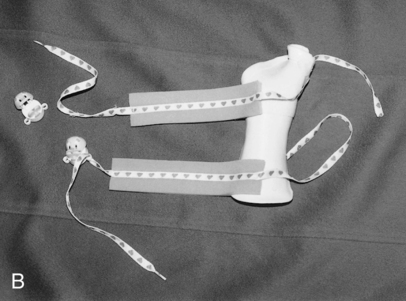
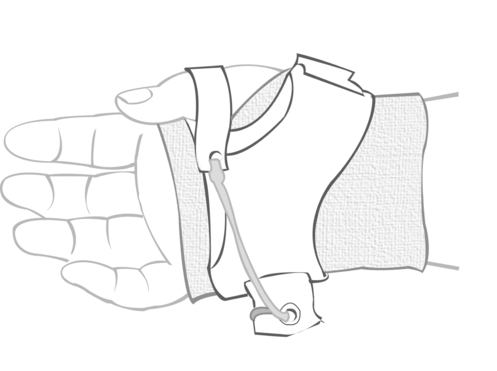
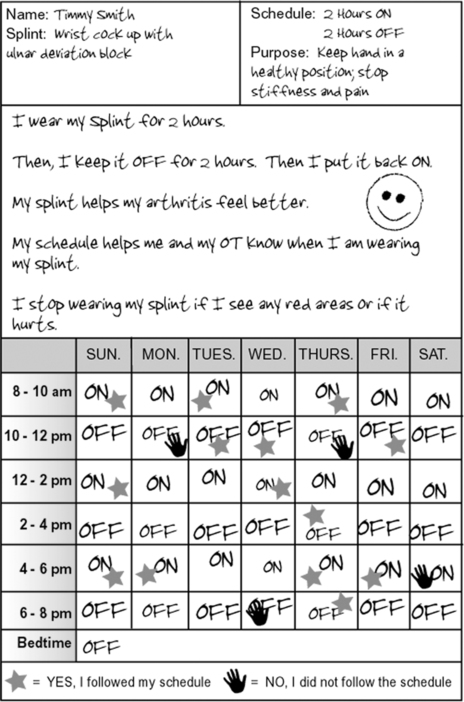
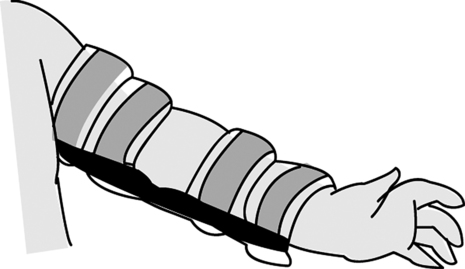
27 ALLYSON BARRY and MELISSA M. STEVENS* After studying this chapter, the reader will be able to accomplish the following: • Explain how orthoses and taping impact the occupational performance of children and adolescents • Describe general considerations when fabricating and providing an orthosis • Understand the goals of orthoses and taping for children and adolescents • Define common orthosis options specific to upper and lower extremity problems • Understand how orthoses and taping are used as intervention in pediatric practice • Describe the role of a certified occupational therapy assistant (COTA) in fabricating and using orthoses and taping • Explain strategies to increase the compliance of children and adolescents in using orthoses • Describe terms, concepts, and trends in the use of Kinesio Tex taping method • Discuss the best practice strategies for application, reassessment, and use of Kinesio Tex taping • Provide concise information regarding the use, technique of application, and contraindications of Kinesio Tex tape OT practitioners traditionally used the term splint to describe temporary devices fabricated to support a part of the body, whereas the term orthotic was used to refer to a more permanent device. To eliminate confusion in the use of terminology among orthotists, OT practitioners, and insurance companies, OT practitioners are now encouraged to use the term orthosis to refer to temporary and permanent devices that immobilize, restrain, or support a part of the body.2 Therefore, this chapter will use the terms splints and orthoses interchangeably. The purpose of an orthosis/splint is to protect, correct, or assist a joint, limb, or muscle to increase functional performance.5 For example, an orthosis might protect an injured wrist from increased pain when a child or adolescent is playing or prevent deformity occurring during sleep. An orthosis might help support a child’s wrist to make writing more efficient. Orthoses may be classified as static or dynamic. Static orthoses prevent movement, promote functional position, and prevent deformity. Dynamic orthoses allow children to move the joints and assist with movement. Table 27-1 provides additional definitions of the types of orthoses in accordance with the Centers for Medicare and Medicaid (CMS). TABLE 27-1 Sample Types of Orthoses According to Centers for Medicare and Medicaid (CMS) From CMS HCPCS Public Meeting Summary (by Chris Blake of the American Society of Hand Therapists), June 8, 2005. Orthoses may stabilize, support, or protect body parts enabling children to use their hands (or legs in the case of lower extremity orthoses) during activities of daily living (ADLs), education, play, and social participation. OT practitioners consider many factors before designing and fabricating an orthosis to help a child engage in daily occupations. The OT practitioner considers the child’s age, diagnosis, motivations, interests, habits, and routines, along with the context in which the orthosis will be worn. Context refers to the setting in which the child belongs, such as school, home, and his or her cultural, physical, temporal (i.e., time in child’s life), and social environments.1 The OT practitioner also considers the child’s physical abilities (including range of motion [ROM], muscle tone, strength, endurance, and structural appearance). The OT practitioner uses clinical reasoning to determine the best solution for the child. For example, the OT practitioner may decide that a simple design is best to ensure proper wear and compliance or that a prefabricated orthosis will meet a particular child’s temporary needs, whereas another child may need a custom-made orthosis for long-term wear. Examples of the use of orthoses include the following: • Orthoses sometimes provide children with external support necessary to improve ROM or to help the child compensate for lack of ROM. For example, a universal cuff allows a child who has a hand deformity to hold a spoon. • Children who experience joint pain, such as children who have juvenile rheumatoid arthritis (JRA), may benefit from orthoses that will help them rest their joints. In this case, the purpose of the orthosis is to help children maintain ROM but rest the joint adequately during inflammatory periods of this disease (Figure 27-1). • Children with muscle tone abnormalities may benefit from external support of the joints, which will provide them with stability that they typically lack. For example, an elbow orthosis may stabilize the elbow joint allowing the child or adolescent to focus on using his or her hands for holding objects more easily. A thumb splint may provide enough tactile input, sustained over time to open a fisted hand enough so that the child is able to pick up objects in the palm. OT practitioners consider typical child and adolescent development (e.g., gross and fine motor skill development, age, and occupational roles) when fabricating an orthosis. (See Table 27-2 for a description of upper extremity development.) For example, 8-month-old infants crawl on their hands and knees. Therefore, the OT practitioner making an orthosis for this infant wants to be sure that the splint allows the child to crawl. TABLE 27-2 Adapted from Jacobs ML, Austin N: Splinting the hand and upper extremity: Principles and process, Baltimore, MD, 2003, Lippincott Williams and Wilkins. Orthoses are customized to fit the individual and meet his or her occupational needs.2,3,9 By positioning a limb in a functional position, the child or adolescent may engage in meaningful occupations such as play and ADLs. OT practitioners use their knowledge of anatomy, kinesiology, the child’s medical condition(s) along with information about the child’s age, developmental level, contexts, and, most importantly, the purpose of the orthosis. The OT practitioner uses all of these factors for clinical reasoning in order to design and fabricate the device. Generally, orthoses are recommended to improve function, promote proper position, and ensure hygiene. OT practitioners fabricate orthoses based on principles of anatomy and kinesiology. Box 27-1 provides an overview of these principles. A functional orthosis can substitute for weak or absent muscles, which may be caused by peripheral nerve dysfunction, neuromuscular disorders (e.g., CP), or spinal cord injuries.2,4 Other examples of functional orthoses include those designed to help the child hold a pencil, toy, or eating utensil. Several types of orthoses are used to improve hand function. • Serial static orthoses immobilize joints in a stationary position.6 The serial static orthosis applies continued force to maximize the length of the tissue and is worn for long periods allowing the tissue to adapt. Once the tissue has accommodated to the stretch, a new orthosis may be made, or the old orthosis is remolded, to hold the tissue at a new maximum length.6 • Dynamic orthoses apply force to one or more joints. These orthoses include a rubber band, pulley, spring, screw, hook, elastic, or other outriggers to provide the continuous force.4 These types of orthoses are not worn as long as the serial orthoses. The force is continuous while the orthosis remains on, but the orthosis is removed periodically.4 • Static progressive orthoses are used to apply adjustable static force. The orthosis is applied as the joint is positioned at its maximum. The force is then adjusted when the tissue response allows repositioning to a new length.4 Three stages of healing follow tissue injury: (1) inflammatory (where the wound prepares to heal), (2) fibroplastic (the tissue structure is rebuilt), and (3) remodeling (configuration develops).7 Edema can occur during any of these stages due to lack of functional use, which leads to stiffness and adherence and therefore continued inactivity.4 Edema, or excess fluid build up, may develop due to increased capillary permeability, which results in leakage of fluid and protein into the tissue spaces.13 Elevation, active motion, gentle external massage, and compression may all help minimize edema. orthoses provide a form of compression and may decrease edema, reduce pain, and encourage tissue repair.13 Applying orthoses during the early phase of healing allows the necessary rest and compression, as well as positioning, which protects the healing structures while maintaining a balanced, functional position.13 Some health disorders cause edema and inflammation as well. Orthoses are an effective way to mobilize the stiff hand, but orthoses are most effective when combined with an exercise program.4 Static orthoses serve the following purposes: • They decrease or prevent contractures by maximizing range of motion (ROM), thus preventing muscle and tendon shortening. • They provide stability to an unstable joint by giving external support to the joint. • They improve joint alignment and prevent the progression of deformity. An orthosis may place the child’s or adolescent’s hand in the proper anatomical position. • They provide rest to assist the healing process. (An orthosis will, for example, hold the hand in proper anatomic alignment, allowing the soft tissues to heal and edema and inflammation to diminish.4) The occupational therapist evaluated Timmy’s hand function. The occupational therapist and OTA together designed a wrist extension orthosis with ulnar deviation block for Timmy (Figure 27-3). The wrist extension orthosis held Timmy’s hand in slight wrist extension while providing a passive stretch to the wrist flexors. He wore his wrist extension orthosis with 2-hour increments to eliminate joint stiffness. See Figure 27-4 for Timmy’s schedule for wearing the orthosis. Using orthotic devices to prevent a child or adolescent from self-abuse and interfering behaviors or after a surgical procedure may be an adjunctive intervention provided by the OT practitioner.2–4 For example, an orthosis can protect a postoperative area before complete healing has occurred. An orthosis can be designed to help prevent or improve hygiene problems.5–7 For example, a spastic hand that remains fisted is at high risk for skin breakdown. The inability to extend the fingers makes nail clipping difficult, and long or sharp fingernails can cut the skin, which may lead to infection. Orthoses are frequently fabricated to protect the palm and decrease the risk of skin breakdown (Figure 27-6). For example, an elbow extension orthosis may prevent a child from scratching his face. Prior to designing and fabricating an orthosis for a child or adolescent, the OT practitioner considers the occupations in which he or she engages and the purpose of the orthosis for that child. Understanding the desires of the client helps the OT practitioner design an orthosis that is appealing and meaningful to the client, thereby increasing the chances that the orthosis will be worn. Compliance in wearing the orthosis is clearly related to how well the OT practitioner matches the interests and goals of the client. Consequently, the OT practitioner also considers the developmental and functional level as well as the ability to don and doff the orthosis. During consideration of the physical status, the OT practitioner examines skin integrity, edema, ROM, muscle tone, and current functional status. The OT practitioner must clearly evaluate how the client moves and functions to design an orthosis that does not interfere with the client’s own techniques for moving. Since wearing an orthosis is key to the success of the intervention, OT practitioners use a variety of questions to guide decisions on orthoses, such as the following:7 1. What is the desired outcome of using the orthosis? 2. How will the orthosis have an impact on the client’s ability to engage in occupations?
Orthoses, orthosis fabrication, and taping
Definition
NAME
DESCRIPTION*
PURPOSE
Elbow orthosis
Rigid circumferential, dorsal, or volar framed orthosis with soft straps and closures for the arm, elbow, and forearm
Stabilizes and may limit motion of the elbow
Shoulder orthosis
Static, rigid circumferential, dorsal, or volar framed orthosis with soft straps and closures for the shoulder
Statically stabilizes or limits motion of the shoulder
Shoulder, elbow, wrist, hand, finger orthosis SEWHFO
Static, rigid anterior or posterior framed orthosis with soft straps and closures initiating proximal to the glenohumeral joint and axillary region, extending through the upper arm, crossing the elbow, wrists, and hand joints including fingers
Protects medical conditions of the shoulder, elbow, wrist, hand, and fingers during healing process and/or reduces contractures
Finger orthosis
Dynamic, rigid volar or dorsal orthosis with soft straps and closures. The orthosis may initiate at the proximal or middle digital crease and will extend to the tip of the finger/thumb
Protects medical conditions of the finger/thumb during healing process and/or reduces contractures and stiffness
Hand, finger orthosis
Dynamic, rigid volar, dorsal, radially or ulnar contoured orthosis with soft straps and closures; may initiate at the base of the hand and extend to the middle or distal digital crease or to the tip of the fingers
Protects medical conditions of the hand/finger/thumb during healing process and/or reduces contractures and stiffness
General considerations
AGE SKILL APPEARS (MONTHS)
UPPER EXTREMITY SKILLS
0–2
Physiologic flexion
2
Grasp reflex
3
Hands together on chest in supine position
4
Grasp reflex diminishing; objects held in both hands at midline; in supine position bears weight on forearm, with more weight on the ulnar than the radial side; pats sides of bottle with hands
5
Two-handed approach to objects, but grasp is unilateral; bilateral transfer; extended-arm weight bearing in prone position; places two hands on bottle, with some forearm supination
6
Weight shifts on extended arms in prone position; sits with a straight back; elbows fully extend when reaching
7
First purposeful release; pulls self to stand
8
Crawls on hands and knees
9
Active forearm supination when reaching
10
Pokes with index finger
12
Uses hands in coordinated manner in which one hand stabilizes and the other manipulates; begins to scribble
15
Releases a pellet with wrist extension and precision
Goals of orthosis fabrication
Use of orthoses to improve function
Use of orthoses to promote proper position
Use of orthoses to improve hygiene and prevent skin breakdown
Considerations for providing orthoses to children and adolescents
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Orthoses, orthosis fabrication, and taping
Only gold members can continue reading. Log In or Register to continue