Chapter 68 Orthopedics
A Practical Approach
NEWBORN INFANT
ETIOLOGY
EVALUATION
How Do I Detect Developmental Dysplasia of the Hip?
Careful examination of the hips is mandatory for all newborns. The Ortolani maneuver identifies the dislocated hip, and the Barlow maneuver identifies the dislocatable hip. Careful attention to proper technique is critical (See Chapter 5 and Figure 5-4). You must be able to distinguish DDH from a capsular or ligamentous click, which is a benign finding similar to the “popping” that might occur in your own joints. This click is very different from the gross “clunk” felt when a hip is reduced or dislocated by the Ortolani or Barlow maneuver, respectively. The examination for DDH is done on each physical examination until the age of 1 year, but after age 2 to 3 months, the dislocated hip cannot be reduced by the Ortolani maneuver, and limited abduction is the abnormal finding in DDH. Ultrasonography is the preferred imaging modality when DDH is suspected.
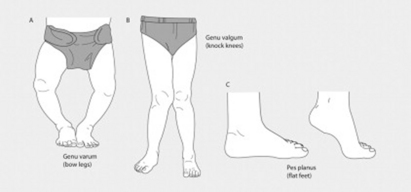
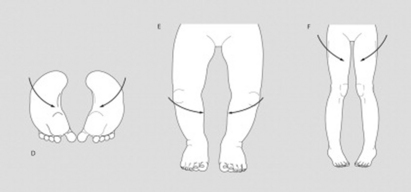
How Do I Distinguish the Various Foot Deformities?
All foot deformities are identified by visual inspection and by manipulation to determine whether the deformity is flexible or rigid. The lateral border of the sole of the foot should be a straight line. Metatarsus varus (Figure 68-1D) is present if the foot curves inward (like the letter C). If the curve can be easily straightened, it represents a flexible deformity. A fixed deformity cannot be easily straightened. Talipes equinovarus or clubfoot requires three features for diagnosis: hindfoot equinus (plantarflexion of the foot at the ankle), hindfoot varus (inversion deformity of the heel), and forefoot varus. This deformity cannot be straightened by simple manipulation.
OLDER INFANTS AND TODDLERS
ETIOLOGY
What Orthopedic Problems Affect This Age Group?
Older infants and toddlers commonly have deformities of the extremities, mainly of the legs, that provoke parental concern. Most do not cause long-lasting problems and do not require any treatment, but you must be able to identify them so that you can reassure worried parents. The deformities reflect physiologic variations of “normal” and include either angulation at a joint or rotation along a long bone (Figure 68-1). Angular deformities affect the knees (genu valgus and genu varus) and the feet (metatarsus varus—also called metatarsus adductus). Although metatarsus varus should be identified and managed in the newborn, it may be undetected until the child begins to walk and parents experience problems finding shoes that fit. Rotational deformities affect the femur (femoral anteversion or retroversion) and the tibia (tibial torsion). Femoral anteversion describes internal rotation of the femur, and femoral retroversion describes external rotation. Both cause the feet to turn away from the expected straight position and may be associated with tripping or gait patterns that concern parents. Internal tibial torsion (ITT) refers to rotation along the long axis of the bone, not bowing. The rotation of ITT is toward the midline, resulting in the feet also “turning in” toward the midline.
EVALUATION
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree