ORTHOPEDICS
What is the most likely diagnosis?
a. Diabetic neuropathy
b. Multiple sclerosis
c. Carpal tunnel syndrome
d. Syphilis
e. Syringomyelia
Answer c. Carpal tunnel syndrome
Carpal tunnel syndrome is a collection of symptoms caused by the compression of the median nerve within the carpal tunnel. Symptoms include paresthesias, motor weakness, and wasting of the muscles innervated by the median nerve. Multiple sclerosis is a demyelinating disorder of the central nervous system with multiple neurologic deficits, commonly visual disturbance. Diabetic neuropathy would present with pain and tingling in a “stocking and glove” distribution, but this patient does not have diabetes. Syphilis can cause tabes dorsalis, but this would affect vibratory sense, 2-point discrimination, and proprioception. Syringomyelia is a lack of pain and temperature in a capelike distribution.
In carpal tunnel syndrome, sensory fibers often are affected first followed by motor fibers.
The median nerve is damaged within the rigid confines of the carpal tunnel, initially undergoing demyelination followed by axonal degeneration.
Wasting and weakness of the median-innervated hand muscles include:
• L: First and second lumbricals
• O: Opponens pollicis
• A: Abductor pollicis brevis
• F: Flexor pollicis brevis
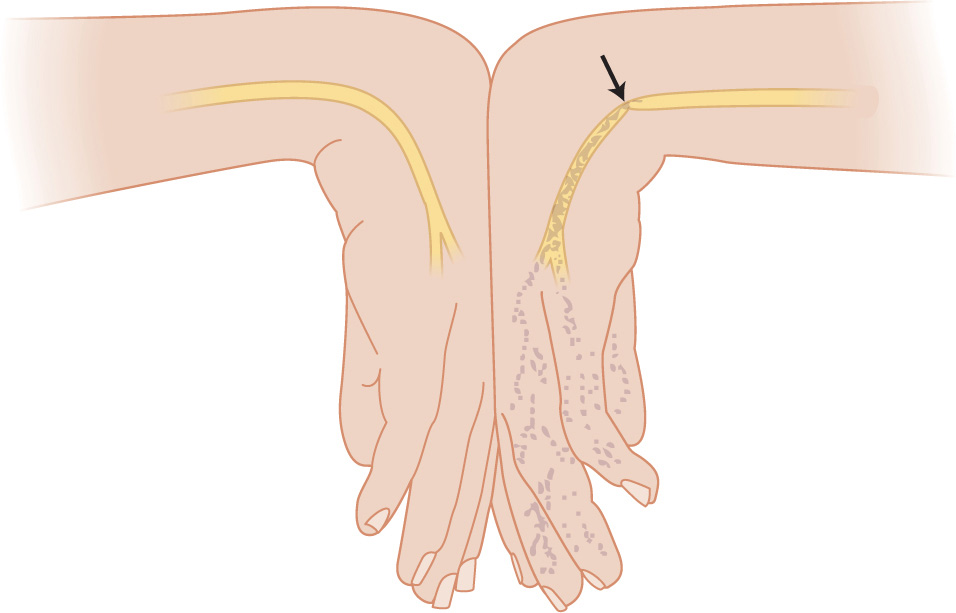
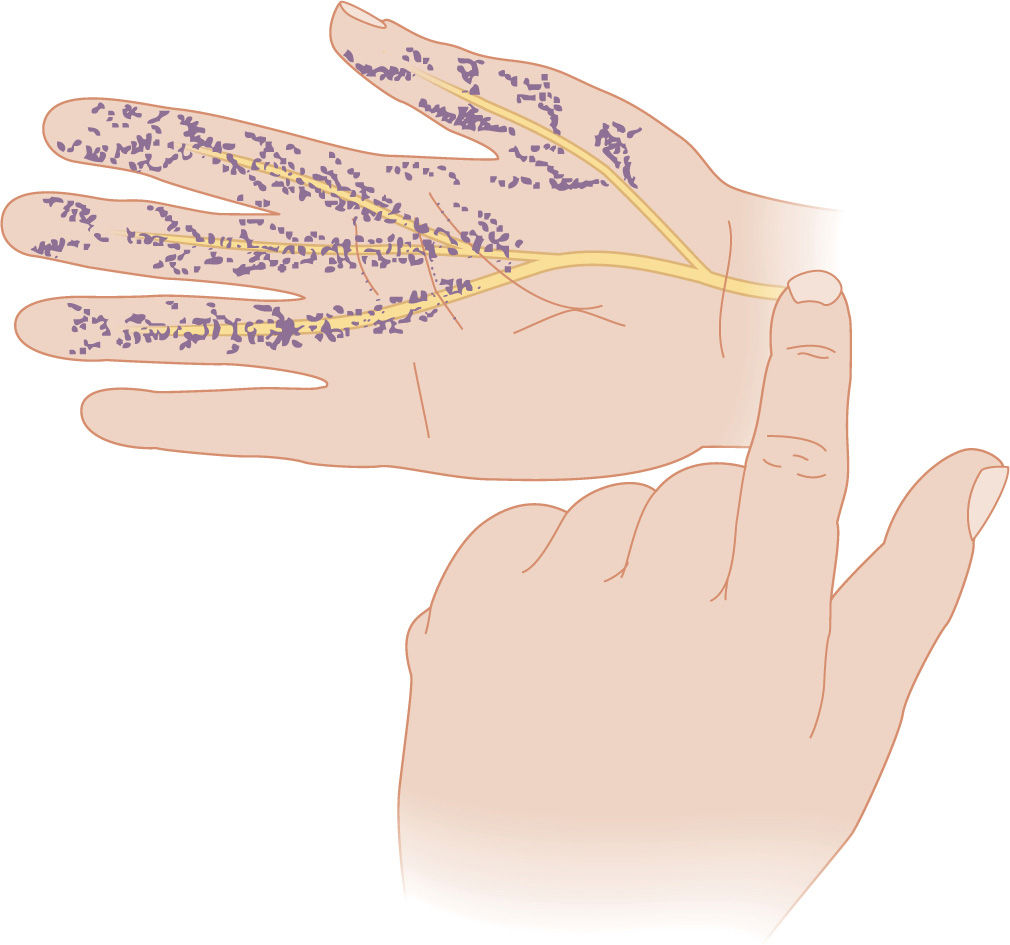
Figure 13-2. Phalen maneuver. The Phalen maneuver is performed by compressing the opposing dorsal surfaces of the hand with the wrists flexed together as shown. (Reproduced, with permission, from Simon RR, Sherman SC. Emergency Orthopedics. 6th ed. New York: McGraw-Hill; 2011.)
What is the best next step in the management of this patient?
a. Surgery
b. Wrist splinting
c. Nonsteroidal antiinflammatory drugs (NSAIDs)
d. Oral steroids
e. Steroid injection
f. Physical therapy or yoga
g. Ultrasound therapy
Answer b. Wrist splinting
After the diagnosis of carpal tunnel syndrome is made, the best next step is conservative therapy with placement of the affected hands into a wrist splint in the “neutral position.” Wrist splints, oral steroids, ultrasound therapy, and yoga are only effective in the short term, but wrist splinting is the most effective (Figure 13-3). Steroid injection is considered second-line therapy and a bridge to surgery. Surgery is considered the most definitive therapy and should only be used if splinting and conservative measures have failed.

Figure 13-3. Typical wrist splint with the wrist in neutral position for treatment of carpal tunnel syndrome. (Used, with permission, from Barbara Steckler and Judy Tintinalli.)
Bones of the carpal tunnel are:
• Scaphoid
• Lunate
• Triquetrum
• Pisiform
• Trapezium
• Trapezoid
• Capitate
• Hamate
What is the best next step in the management of this patient?
a. Surgery
b. Steroid injection
c. NSAIDs
d. Physical therapy
Answer b. Steroid injection
Second-line therapy for a patient with carpal tunnel syndrome is steroid injection directly into the carpal tunnel, which is only used after conservative measures have failed. If the patient returns with symptoms and conservative measures such as splinting and steroid injections have failed, the patient should be referred for surgery.
The carpal bones form the dorsal surface of the tunnel, and the volar surface is formed by the flexor retinaculum.
Surgery in carpal tunnel syndrome involves cutting the transverse ligament.
What is the most likely diagnosis?
a. Pulmonary embolism (PE)
b. Fat embolism
c. Amniotic fluid embolism
d. Thrombotic thrombocytopenic purpura (TTP)
e. Henoch-Schönlein purpura (HSP)
Answer b. Fat embolism
Fat embolism is a type of embolism that is secondary to physical trauma, such as long bone traumas. It can also occur from parenteral lipid infusion or burns. The triad of findings in a patient with fat embolism is neurologic dysfunction, petechial rash, and respiratory distress. This patient presents with all findings: the neurologic dysfunction manifested as a seizure, while the respiratory distress is seen as the patient overbreathing the vent and dropping pulse oximetry. A PE presents with respiratory distress but would not have a petechial rash, and an amniotic fluid embolism requires the patient to be pregnant. TTP is a combination of neurologic dysfunction and purpura but would not include a patient in respiratory distress. Last, HSP is small vessel vasculitis with deposition of IgA, classically seen after a recent bacteria or viral illness such as streptococci or hepatitis B.
Fat embolism are caused by large fat droplets being released into the venous system and obstructing capillary beds.
What is the best next step in the management of this patient?
a. Heparin
b. Low-molecular-weight heparin (LMWH)
c. Surgical fixation of the long bones
d. Inferior vena cava filter placement
e. Observation
Answer c. Surgical fixation of the long bones
The best next step in the management of this patient is stabilization of long bone fractures. Fixation within 24 hours has been shown to reduce the incidence of respiratory distress from embolic phenomenon. LMWH and anticoagulation are the most common wrong answers and are indicated if there is a blood clot that has embolized, but not for fat. Placement of inferior vena cava filters is not indicated, and observation will result in detrimental outcomes. The mainstay of therapy after surgical fixation is supportive care.
What is the most likely diagnosis?
a. Cellulitis
b. Upper extremity deep venous thrombosis (DVT)
c. Rhabdomyolysis
d. Acute compartment syndrome
e. Arterial embolism
Answer d. Acute compartment syndrome
The 6 Ps of compartment syndrome are pain out of proportion to what is expected based on the physical examination findings, paresthesia, pallor, paralysis, pulselessness, and poikilothermia. The underlying etiology of compartment syndrome is rising pressures in the muscle compartment. This is because the fascia layer does not stretch, and thus any swelling, bleeding, or accumulation of fluid can cause significant impairment. Cellulitis would present with pain and fever, but there is never neurologic compromise or lack of pulses. An upper extremity DVT would present with painful swelling, and arterial embolism presents as painful swelling in the setting of a patient with atrial fibrillation. Rhabdomyolysis presents with muscle pain and elevated creatinine kinase levels.