FIGURE 29-1 Decline in operative vaginal delivery rates, 1990–2010. (From Martin, 2012.)
INDICATIONS
If it is technically feasible and can be safely accomplished, termination of second-stage labor by operative vaginal delivery is indicated in any condition threatening the mother or fetus that is likely to be relieved by delivery. Some fetal indications for operative vaginal delivery include nonreassuring fetal heart rate pattern and premature placental separation. In the past, forceps delivery was believed to be somewhat protective of the fragile preterm infant head. Subsequent studies, however, reported no significant differences in outcomes for neonates who weighed 500 to 1500 g between those delivered spontaneously and those delivered by outlet forceps (Fairweather, 1981; Schwartz, 1983).
Some maternal indications include heart disease, pulmonary injury or compromise, intrapartum infection, and certain neurological conditions. The most common are exhaustion and prolonged second-stage labor. For nulliparas, the latter is defined as > 3 hours with or > 2 hours without regional analgesia (American College of Obstetricians and Gynecologists, 2012). In parous women, it is defined as > 2 hours with and > 1 hour without regional analgesia.
Operative vaginal delivery should generally be performed from either a low or outlet station. Additionally, forceps or vacuum delivery generally should not be used electively until the criteria for an outlet delivery have been met. In these circumstances, operative vaginal delivery is a simple and safe operation, although with some risk of maternal lower reproductive tract injury (Yancey, 1991). Moreover, there is no evidence that use of prophylactic operative delivery is beneficial in the otherwise normal delivery.
CLASSIFICATION AND PREREQUISITES
The American College of Obstetricians and Gynecologists (2012) classifies operative vaginal deliveries as summarized in Table 29-1. It emphasizes that the two most important discriminators of risk for both mother and infant are station and rotation. Station is measured in centimeters, –5 to 0 to +5. Zero station reflects a line drawn between the ischial spines. Deliveries are categorized as outlet, low, and midpelvic procedures. High forceps, in which instruments are applied above 0 station, have no place in contemporary obstetrics.
TABLE 29-1. Operative Vaginal Delivery Prerequisites and Classification According to Station and Rotationa
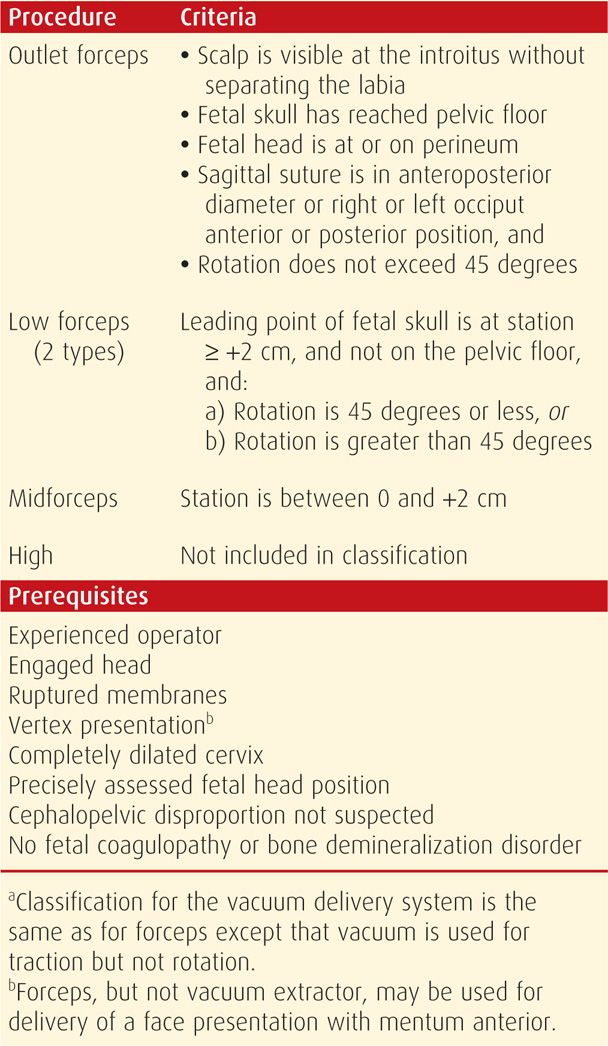
Once station and rotation are assessed, there are several prerequisites for operative vaginal delivery (see Table 29-1). In addition and specific to vacuum extraction, fetuses should be at least 34 weeks gestational age, and although infrequently used in the United States, fetal scalp blood sampling should not have been recently performed.
Regional analgesia or general anesthesia is preferable for low forceps or midpelvic procedures, although pudendal blockade may prove adequate for outlet forceps. Before operative vaginal delivery, the bladder should also be emptied to provide additional pelvic space and minimize bladder trauma.
MORBIDITY
In general, a higher station and/or greater degrees of rotation increase the chance of maternal or fetal injury. In the discussion of operative vaginal delivery, morbidity is most properly compared with morbidity from cesarean delivery, and not with that from spontaneous vaginal delivery. This is because the alternative to indicated operative vaginal delivery is cesarean delivery. As examples, postpartum uterine infection and pelvic cellulitis are more frequent, and often more severe, in women following cesarean delivery compared with that following operative vaginal delivery (Robertson, 1990). Moreover, in a study of more than 1 million births, Spiliopoulos and associates (2011) reported cesarean delivery, but not operative vaginal delivery, as a risk for peripartum hysterectomy.
 Maternal Morbidity
Maternal Morbidity
Lacerations
The very conditions that lead to indications for operative vaginal delivery also increase the need for episiotomy and the likelihood of lacerations (de Leeuw, 2008). That said, operative vaginal delivery is associated with higher rates of third- and fourth-degree lacerations as well as vaginal wall and cervical lacerations (Hamilton, 2011; Hirayama, 2012; Landy, 2011). These appear to occur more frequently with forceps compared with vacuum extraction, and especially if there is a midline episiotomy (Kudish, 2006; O’Mahony, 2010). Hagadorn-Freathy and coworkers (1991) reported a 13-percent rate of third- and fourth-degree episiotomy extensions and vaginal lacerations for outlet forceps, 22 percent for low forceps with less than 45-degree rotation, 44 percent for low forceps with more than 45-degree rotation, and 37 percent for midforceps deliveries.
In an effort to lower rates of third- and fourth-degree lacerations, and coincident with overall efforts to reduce routine episiotomy use, many advocate only indicated episiotomy with operative vaginal delivery. For example, Ecker and colleagues (1997) reported a significant decrease in the episiotomy rate with both forceps—96 to 30 percent—as well as vacuum—89 to 39 percent—deliveries from 1984 to 1994. During this time, there was a decrease in fourth-degree but no change in third-degree lacerations. If episiotomy is required, several studies have reported a protective effect from mediolateral episiotomy against these more extensive perineal lacerations (de Leeuw, 2008; de Vogel, 2012; Hirsch, 2008). But as discussed in Chapter 27 (p. 551), this is balanced against the additional potential morbidity compared with a midline episiotomy. Early disarticulation of forceps and cessation of maternal pushing during disarticulation can also be protective. Last, these injuries are more common with operative vaginal delivery from an occiput posterior position (Damron, 2004). Thus, manual or forceps rotation from occiput posterior to occiput anterior position and then subsequent operative vaginal delivery may decrease lower-reproductive-tract injury.
Pelvic Floor Disorders
This term encompasses urinary incontinence, anal incontinence, and pelvic organ prolapse. Operative vaginal delivery has been suggested as a possible risk for each of these. Proposed mechanisms include structural compromise and/or pelvic floor denervation secondary to forces exerted during delivery.
Urinary retention and bladder dysfunction are often short-term effects of forceps and vacuum deliveries (Mulder, 2012). Importantly, episiotomy and epidural analgesia, both common associates of operative vaginal delivery, are also identified risks for urinary retention. Symptoms are brief and typically resolve with 24 to 48 hours of passive catheter bladder drainage.
Regarding more sustained urinary dysfunction, parity and specifically vaginal delivery are known risk factors for urinary incontinence (Gyhagen, 2013; Rortveit, 2003). And, a few studies show a greater attributable risk with operative vaginal delivery (Baydock, 2009; Handa, 2011). But, many studies do not support an increased risk compared with vaginal delivery alone (Handa, 2012; Leijonhufvud, 2011; MacArthur, 2006; Thom, 2011).
Evidence linking anal incontinence with operative vaginal delivery is conflicting. Some studies show that anal sphincter disruption caused by higher-order episiotomy, but not delivery mode, is the main etiological factor strongly associated with anal incontinence (Baud, 2011; Bols, 2010; Evers, 2012; Nygaard, 1997). In contrast, others directly link operative vaginal delivery with this complication (MacArthur, 2005; Pretlove, 2008). But, these studies may not be incongruous as operative vaginal delivery, as previously discussed, is associated with increased rates of higher-order episiotomy. Importantly, several studies and reviews have not found cesarean delivery to be protective for anal incontinence (Nelson, 2010).
Last, evidence linking pelvic organ prolapse with operative vaginal delivery also shows mixed results (Gyhagen, 2013; Handa, 2011). Interestingly, Glazener and associates (2013) evaluated women 12 years after delivery by means of a symptom questionnaire and physical examination. Complaints of prolapse symptoms were linked to operative vaginal delivery, but true objective measurement of prolapse showed a protective effect from this delivery mode compared with vaginal delivery alone.
 Perinatal Morbidity
Perinatal Morbidity
Acute Perinatal Injuries
These are more frequent with operative vaginal deliveries than with cesarean delivery or spontaneous vaginal delivery alone. Although these may be seen with either method, they are more commonly seen with vacuum extraction. Some injuries include cephalohematoma, subgaleal hemorrhage, retinal hemorrhage, neonatal jaundice secondary to these hemorrhages, shoulder dystocia, clavicular fracture, and scalp lacerations. Cephalohematoma and subgaleal hemorrhage are both extracranial lesions described in Chapter 33 (p. 646).
In 1998, the Food and Drug Administration issued a Public Health Advisory regarding the possible association of vacuum-assisted delivery with serious fetal complications, including death. In response, the American College of Obstetricians and Gynecologists (1998) issued a Committee Opinion recommending the continued use of vacuum-assisted delivery devices when appropriate. At that time, they estimated that there was approximately one adverse event per 45,455 vacuum extractions per year.
In contrast, forceps-assisted vaginal delivery has higher rates of facial nerve injury, brachial plexus injury, depressed skull fracture, and corneal abrasion (Demissie, 2004; Dupuis, 2005; American College of Obstetricians and Gynecologists, 2012). And while some studies have associated vacuum extraction with higher rates of intracranial hemorrhage, others show similar rates with either of the two methods (Towner, 1999; Wen, 2001; Werner, 2011).
As a group, if operative vaginal delivery is compared with cesarean delivery, rates of extracranial hematoma, skull fracture, facial nerve or brachial plexus injury, retinal hemorrhage, and facial or scalp laceration are lower with cesarean delivery, and shoulder dystocia is eliminated. Importantly, however, fetal acidemia rates are not increased with operative vaginal delivery (Contag, 2010; Walsh, 2013). Intracranial hemorrhage rates are similar among infants delivered by vacuum extraction, forceps, or cesarean delivery during labor (Towner, 1999). But, these rates are higher than among those delivered spontaneously or by cesarean delivery before labor. These authors suggest that the common risk factor for intracranial hemorrhage is abnormal labor. Werner and associates (2011), in their evaluation of more than 150,000 singleton deliveries, reported that forceps-assisted delivery was associated with fewer total neurological complications compared with vacuum-assisted or cesarean delivery. However, as a subset, subdural hemorrhage was significantly more frequent in both operative vaginal delivery cohorts compared with infants in the cesarean delivery group.
Reports of neonatal morbidity rates compared between midforceps and cesarean delivery are conflicting. In the study by Towner and colleagues (1999), similar risks were reported for intracranial hemorrhage. Bashore and associates (1990) observed comparable Apgar scores, cord blood acid-base values, neonatal intensive care unit admission, and birth trauma between these two. In another study, however, Robertson and coworkers (1990) reported significantly higher rates of these adverse outcomes in the midforceps group. And Hagadorn-Freathy and colleagues (1991) reported an increased risk for facial nerve palsy—9 percent—with midforceps delivery.
Mechanisms of Acute Injury
In general, with operative vaginal delivery, the types of fetal injury can usually be explained by the forces exerted. In cases of cephalohematoma or subgaleal hemorrhage, suction and perhaps rotation during vacuum extraction may lead to a primary vessel laceration (Fig. 33-1, p. 647). Intracranial hemorrhage may result from skull fracture and vessel laceration or from vessel laceration alone due to exerted forces. With facial nerve palsy, one of the forceps blades may compress the nerve against the facial bones (Duval, 2009; Falco, 1990). The higher rates of shoulder dystocia seen with vacuum extraction may result from the angle of traction. With the vacuum, this angle creates vector forces that actually pull the anterior shoulder into the symphysis pubis (Caughey, 2005). To explain brachial plexus injury, Towner and Ciotti (2007) proposed that as the fetal head descends down the birth canal, the shoulders may stay above the pelvic inlet. Thus, similar to shoulder dystocia at the symphysis, this “shoulder dystocia at the pelvic inlet” is overcome by traction forces but with concomitant stretch on the brachial plexus.
Long-Term Infant Morbidity
Evidence regarding long–term neurodevelopmental outcomes in children delivered by operative vaginal delivery is reassuring. Seidman and colleagues (1991) evaluated more than 52,000 Israeli Defense Forces draftees at age 17 years and found that regardless of delivery mode, there were similar rates of physical or cognitive impairments. Wesley and associates (1992) noted similar intelligence scores among 5-year-olds following spontaneous, forceps, or vacuum deliveries. Murphy and coworkers (2004) found no association between forceps delivery and epilepsy in a cohort of 21,441 adults. In their epidemiological review, O’Callaghan and colleagues (2011) found no association between cerebral palsy and operative vaginal delivery. A prospective study by Bahl and associates (2007) included children of 264 women who underwent operative delivery. Their incidence of neurodevelopmental morbidity was similar in those undergoing successful forceps delivery, failed forceps with cesarean delivery, or cesarean delivery without forceps.
Data regarding midforceps deliveries are for the most part reassuring. Broman and coworkers (1975) reported that infants delivered by midforceps had slightly higher intelligence scores at age 4 years compared with those of children delivered spontaneously. Using the same database, however, Friedman and associates (1977, 1984) analyzed intelligence assessments at or after age 7 years. They concluded that children delivered by midforceps had lower mean intelligence quotients compared with children delivered by outlet forceps. In yet another report from this same database, Dierker and colleagues (1986) compared long-term outcomes of children delivered by midforceps with those of children delivered by cesarean after dystocia. The strength of this study is the appropriateness of the control group. These investigators reported that delivery by midforceps was not associated with neurodevelopmental disability. Last, Nilsen (1984) evaluated 18-year-old men and found that those delivered by Kielland forceps had higher intelligence scores than those delivered spontaneously, by vacuum extraction, or by cesarean. As discussed on page 582, Burke and coworkers (2012) reported 144 cases of attempted Kielland forceps rotation and described minimal morbidity.
TRIAL OF OPERATIVE VAGINAL DELIVERY
If an attempt to perform an operative vaginal delivery is expected to be difficult, then it should be considered a trial. Delivery is conducted preferably in an operating room equipped and staffed for immediate cesarean delivery. If forceps cannot be satisfactorily applied, then the procedure is stopped and either vacuum extraction or cesarean delivery is performed. With the former, if there is no descent with traction, the trial should be abandoned and cesarean delivery performed.
With such caveats, cesarean delivery after an attempt at operative vaginal delivery was not associated with adverse neonatal outcomes if there was a reassuring fetal heart rate tracing (Alexander, 2009). A similar study evaluated 122 women who had a trial of midcavity forceps or vacuum extraction in a setting with full preparations for cesarean delivery (Lowe, 1987). Investigators found no significant difference in immediate neonatal or maternal morbidity compared with that of 42 women delivered for similar indications by cesarean but without such a trial. Conversely, in 61 women who had “unexpected” vacuum or forceps failure in which there was no prior preparation for immediate cesarean delivery, neonatal morbidity was higher.
Factors associated with operative delivery failure are persistent occiput posterior position, absence of regional or general anesthesia, and birthweight > 4000 g (Ben-Haroush, 2007). In general, to avert morbidity with failed forceps or vacuum delivery, the American College of Obstetricians and Gynecologists (2012) cautions that these trials should be attempted only if the clinical assessment is highly suggestive of a successful outcome. We also emphasize proper training.
Sequential instrumentation most frequently involves an attempt at vacuum extraction followed by one with forceps. This most likely stems from the higher completion rate with forceps compared with vacuum extraction noted earlier (p. 574). There is no evidence to justify this practice, as it significantly increases risks for fetal trauma (Dupuis, 2005; Murphy, 2001; Gardella, 2001). Because of these adverse outcomes, the American College of Obstetricians and Gynecologists (2012) recommends against the sequential use of instruments unless there is a “compelling and justifiable reason.”
TRAINING
As the rate of operative vaginal delivery has declined, so have opportunities for training. Fifteen years ago, Hankins and colleagues (1999) reported that fewer than half of residency directors expected proficiency with midforceps delivery. From the data shown in Figure 29-1, we, and others, would expect that number to be much lower today (Miller, 2014). In many programs, training in even low and outlet forceps procedures has reached critically low levels. For residents completing training in 2012, the Accreditation Council for Graduate Medical Education (2012) lists a median of only six forceps deliveries, and that for vacuum deliveries was 16.
Because traditional hands-on training has evolved, residency programs should have readily available skilled operators to teach these procedures by simulation as well as through actual cases (Spong, 2012). And, the effectiveness of simulation training has been reported (Bahl, 2009; Dupuis, 2006, 2009; Leslie, 2005). In one program, there were lowered rates of maternal and neonatal morbidity associated with operative vaginal delivery after the implementation of a formal education program that included a manikin and pelvic model (Cheong, 2004). In another, assignment of a labor and delivery attending with the specific goal to increase forceps delivery education led to a 59-percent increase in forceps-assisted vaginal delivery rates.
FORCEPS DELIVERY
 Forceps Design
Forceps Design
These instruments consist basically of two crossing branches. Each branch has four components: blade, shank, lock, and handle. Each blade has two curves: the outward cephalic curve conforms to the round fetal head, and the upward pelvic curve corresponds more or less to the axis of the birth canal. Some varieties have an opening within or a depression along the blade surface and are termed fenestrated or pseudofenestrated, respectively (Fig. 29-2). These blade modifications permit a firmer grasp of the fetal head, but at the expense of increased blade thickness, which may increase vaginal trauma. In general, Simpson or Elliot forceps, with their fenestrated blades, are used to deliver a fetus with a molded head, as is common in nulliparous women. The Tucker-McLane forceps have thin smooth blades and are often used for a fetus with a rounded head, which is more characteristic in multiparas (Fig. 29-3). In most situations, however, any of these are appropriate.

FIGURE 29-2 Elliot forceps. A. Note the ample pelvic curve in the blades. B. The cephalic curve, which accommodates the fetal head, is evident in the articulated blades. The fenestrated blade and the overlapping shank in front of the English-style lock characterize these forceps.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


