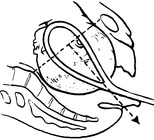
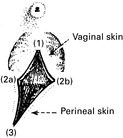
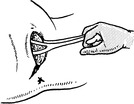
Making an incision in the perineal body at the time of delivery.
Indications
Types of Incision
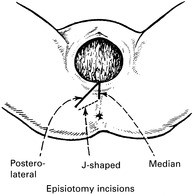
Technique

Repair
FORCEPS DELIVERY
Indications for the use of forceps
Conditions for forceps delivery
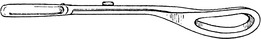
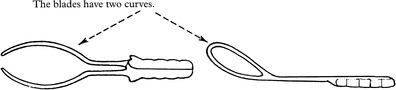
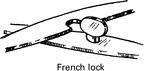
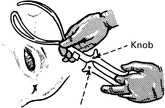
OBSTETRIC FORCEPS


Low Forceps
Mid Forceps
Wrigley’s Forceps

Anderson’s (Simpson’s) Forceps

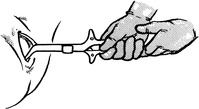
Kielland’s Forceps




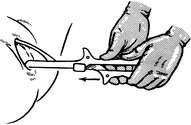
FORCEPS DELIVERY
Preparations
Anaesthesia

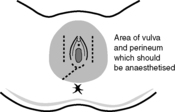
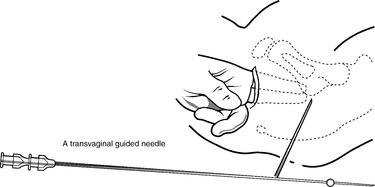
Pudendal Nerve Block
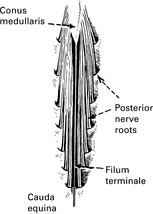
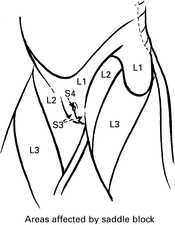
Physiology of Spinal Anaesthesia
Circulatory Effects
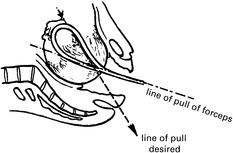
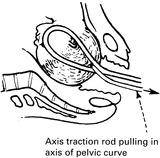
LOW FORCEPS DELIVERY





MID FORCEPS DELIVERY




DELIVERY WITH KIELLAND’S FORCEPS








![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree