Several factors have contributed to improved obstetrical anesthesia safety (Hawkins, 2011). The most significant is the increased use of regional analgesia. Increased availability of in-house anesthesia coverage almost certainly is another important reason. Despite these encouraging results suggesting the safety of general anesthesia, there are now reports of increasing complications with regional analgesia techniques.
GENERAL PRINCIPLES
 Obstetrical Anesthesia Services
Obstetrical Anesthesia Services
The American College of Obstetricians and Gynecologists (2008) reaffirmed its joint position with the American Society of Anesthesiologists that a woman’s request for labor pain relief is sufficient medical indication for its provision. Identification of any of the risk factors shown in Table 25-2 should prompt consultation with anesthesia personnel to permit a joint management plan. This plan should include strategies to minimize the need for emergency anesthesia in women for whom such anesthesia would be especially hazardous.
TABLE 25-2. Maternal Factors That May Prompt Anesthetic Consultation
Morbid obesity
Severe edema or anatomical abnormalities of the face, neck, or spine, including trauma or surgery
Abnormal dentition, small mandible, or difficulty opening the mouth
Extremely short stature, short neck, or neck arthritis
Goiter
Serious maternal medical problems, such as cardiac, pulmonary, or neurological disease
Bleeding disorders
Severe preeclampsia
Prior anesthetic complications
Obstetrical complications likely to lead to operative delivery—examples include placenta previa, preterm breech presentation, or higher-order multifetal gestation
Goals for optimizing obstetrical anesthesia services have been jointly established by the American College of Obstetricians and Gynecologists and the American Society of Anesthesiologists (2009) and include:
1. Availability of a licensed practitioner who is credentialed to administer an appropriate anesthetic whenever necessary and to maintain support of vital functions in an obstetrical emergency
2. Availability of anesthesia personnel to permit the start of a cesarean delivery within 30 minutes of the decision to perform the procedure
3. Anesthesia personnel immediately available to perform an emergency cesarean delivery during the active labor of a woman attempting vaginal birth after cesarean (Chap. 31, p. 615)
4. Appointment of a qualified anesthesiologist to be responsible for all anesthetics administered
5. Availability of a qualified physician with obstetrical privileges to perform operative vaginal or cesarean delivery during administration of anesthesia
6. Availability of equipment, facilities, and support personnel equal to that provided in the surgical suite
7. Immediate availability of personnel, other than the surgical team, to assume responsibility for resuscitation of a depressed newborn (Chap. 32, p. 625).
To meet these goals, 24-hour in-house anesthesia coverage is usually necessary. Providing such service in smaller facilities is more challenging—a problem underscored by the fact that approximately a third of all hospitals providing obstetrical care have fewer than 500 deliveries per year (American College of Obstetricians and Gynecologists, 2009).
Bell and coworkers (2000) calculated the financial burden that may be incurred to provide 24/7 obstetrical anesthesia coverage. Given the average indemnity and Medicaid reimbursement for labor epidural analgesia, they concluded that such coverage could not operate profitably at their tertiary referral institution. Compounding this burden, some third-party payers have denied reimbursement for epidural analgesia in the absence of a specific medical indication—an approach repudiated by the American College of Obstetricians and Gynecologists and the American Society of Anesthesiologists (2008).
 Role of an Obstetrician
Role of an Obstetrician
Every obstetrician should be proficient in local and pudendal analgesia that may be administered in appropriately selected circumstances. In general, however, it is preferable for an anesthesiologist or anesthetist to provide pain relief so that the obstetrician can focus attention on the laboring woman and her fetus.
 Principles of Pain Relief
Principles of Pain Relief
In a scholarly review, Hawkins (2010) emphasized that labor pain is a highly individual response to variable stimuli that are uniquely received and interpreted (Fig. 25-1). These stimuli are modified by emotional, motivational, cognitive, social, and cultural circumstances. Labor pain caused by uterine contractions and cervical dilation is transmitted through visceral afferent sympathetic nerves entering the spinal cord from T10 through L1. Later in labor, perineal stretching transmits painful stimuli through the pudendal nerve and sacral nerves S2 through S4. Cortical responses to pain and anxiety during labor are complex and may be influenced by maternal expectations for childbirth, her age and preparation through education, the presence of emotional support, and other factors. Pain perception is heightened by fear and the need to move into various positions. A woman may be motivated to have a certain type of birthing experience, and these opinions will influence her judgment regarding pain management and other choices during labor and delivery.
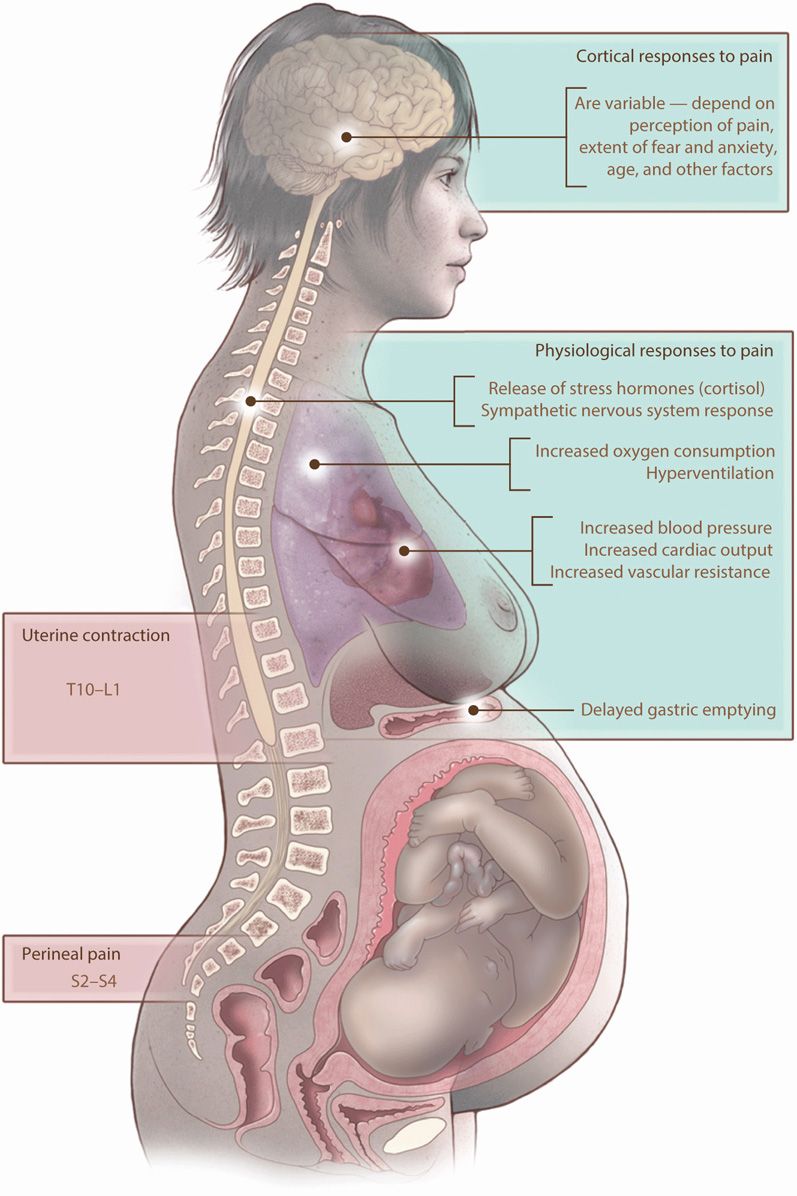
FIGURE 25-1 Sources of pain during labor and maternal physiological responses. (From Hawkins, 2010, with permission.)
Maternal physiological responses to labor pain may influence maternal and fetal well-being and labor progress. For example, hyperventilation may induce hypocarbia. An increased metabolic rate increases oxygen consumption. Increases in cardiac output and vascular resistance may increase maternal blood pressure. Pain, stress, and anxiety cause release of stress hormones such as cortisol and β-endorphins. The sympathetic nervous system response to pain leads to a marked increase in circulating catecholamines that can adversely affect uterine activity and uteroplacental blood flow. Effective analgesia attenuates or eliminates these responses.
ANALGESIA AND SEDATION DURING LABOR
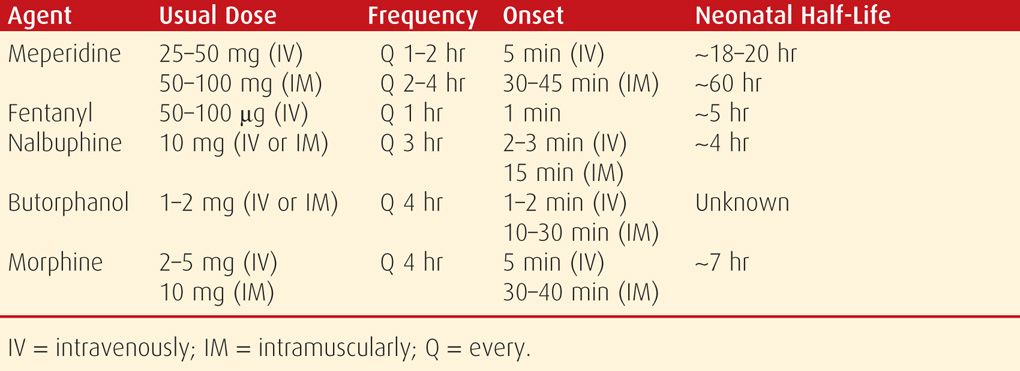
If uterine contractions and cervical dilatation cause discomfort, pain relief with a narcotic such as meperidine (Demerol), plus one of the tranquilizer drugs such as promethazine (Phenergan), is usually appropriate. With a successful program of analgesia and sedation, the mother should rest quietly between contractions. In this circumstance, discomfort usually is felt at the acme of an effective uterine contraction. Appropriate drug selection and administration of the medications shown in Table 25-3 should safely accomplish these objectives.
TABLE 25-3. Some Parenteral Analgesic Agents for Labor Pain
 Parenteral Agents
Parenteral Agents
Meperidine and Promethazine
Meperidine, 50 to 100 mg, with promethazine, 25 mg, may be administered intramuscularly at intervals of 2 to 4 hours. A more rapid effect is achieved by giving meperidine intravenously in doses of 25 to 50 mg every 1 to 2 hours. Whereas analgesia is maximal 30 to 45 minutes after an intramuscular injection, it develops almost immediately following intravenous administration. Meperidine readily crosses the placenta, and its half-life in the newborn is approximately 13 hours or longer (American College of Obstetricians and Gynecologists, 2013b). Its depressant effect in the fetus follows closely behind the peak maternal analgesic effect.
According to Bricker and Lavender (2002), meperidine is the most common opioid used worldwide for pain relief from labor. Tsui and associates (2004) found meperidine to be superior to placebo for pain relief in the first stage of labor. In a randomized investigation of epidural analgesia conducted at Parkland Hospital, patient-controlled intravenous analgesia with meperidine was found to be an inexpensive and reasonably effective method for labor analgesia (Sharma, 1997). Women randomized to self-administered analgesia were given 50-mg meperidine with 25-mg promethazine intravenously as an initial bolus. Thereafter, an infusion pump was set to deliver 15 mg of meperidine every 10 minutes as needed until delivery. Neonatal sedation, as measured by need for naloxone treatment in the delivery room, was identified in 3 percent of newborns.
Butorphanol (Stadol)
This synthetic narcotic, given in 1- to 2-mg doses, compares favorably with 40 to 60 mg of meperidine (Quilligan, 1980). Its major side effects are somnolence, dizziness, and dysphoria. Neonatal respiratory depression is reported to be less than with meperidine. Importantly, the two drugs are not given contiguously because butorphanol antagonizes the narcotic effects of meperidine. Hatjis and Meis (1986) described a transient sinusoidal fetal heart rate pattern following butorphanol administration but with no short-term maternal or neonatal adverse sequelae (Chap. 24, p. 482).
Fentanyl
This short-acting and potent synthetic opioid may be given in doses of 50 to 100 μg intravenously every hour. Its main disadvantage is a short duration of action, which requires frequent dosing or use of a patient-controlled intravenous pump. Moreover, Atkinson and coworkers (1994) reported that butorphanol provided better initial analgesia than fentanyl and was associated with fewer requests for additional medication or for epidural analgesia.
Efficacy and Safety of Parenteral Agents
Parenteral sedation is not without risks. Hawkins and colleagues (1997) reported that 4 of 129 maternal anesthetic-related deaths were from such sedation—one from aspiration, two from inadequate ventilation, and one from overdosage.
Narcotics used during labor may cause newborn respiratory depression. Naloxone is a narcotic antagonist capable of reversing respiratory depression induced by opioid narcotics. It acts by displacing the narcotic from specific receptors in the central nervous system. Withdrawal symptoms may be precipitated in recipients who are physically dependent on narcotics. For this reason, naloxone is contraindicated in a newborn of a narcotic-addicted mother (American Academy of Pediatrics and American College of Obstetricians and Gynecologists, 2012). After adequate ventilation has been established, naloxone may be given to reverse respiratory depression in a newborn infant whose mother received narcotics (Chap. 32, p. 626).
 Nitrous Oxide
Nitrous Oxide
A self-administered mixture of 50-percent nitrous oxide (N2O) and oxygen may provide satisfactory analgesia during labor (Rosen, 2002a). Some preparations are premixed in a single cylinder (Entonox), and in others, a blender mixes the two gases from separate tanks (Nitronox). The gases are connected to a breathing circuit through a valve that opens only when the patient inspires. The use of intermittent nitrous oxide for labor pain has been reviewed by Rosen (2002a).
NERVE BLOCKS
Various nerve blocks have been developed over the years to provide pain relief during labor and/or delivery. These include pudendal, paracervical, and neuraxial blocks such as spinal, epidural, and combined spinal-epidural techniques.
 Anesthetic Agents
Anesthetic Agents
Some of the more commonly used nerve block anesthetics, along with their usual concentrations, doses, and durations of action, are summarized in Table 25-4. The dose of each agent varies widely and is dependent on the particular nerve block and physical status of the woman. The onset, duration, and quality of analgesia can be enhanced by increasing the dose. This can be done safely only by incrementally administering small-volume boluses of the agent and by carefully monitoring early warning signs of toxicity. Administration of these agents must be followed by appropriate monitoring for adverse reactions. Equipment and personnel to manage these reactions must be immediately available.
TABLE 25-4. Local Anesthetic Agents Commonly Used in Obstetrics
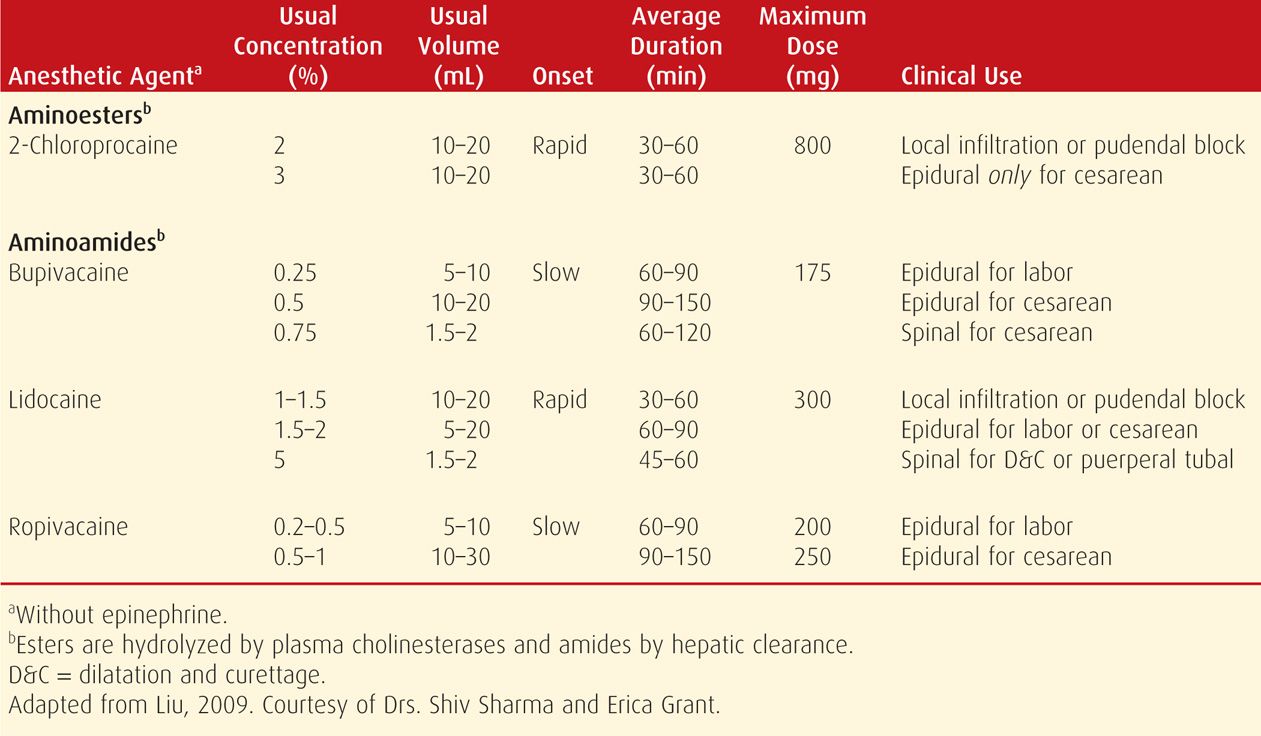
Most often, serious toxicity follows inadvertent intravenous injection. Systemic toxicity from local anesthetics typically manifests in the central nervous and cardiovascular systems. For this reason, when epidural analgesia is initiated, dilute epinephrine is sometimes added and given as a test dose. A sudden significant rise in the maternal heart rate or blood pressure immediately after administration suggests intravenous catheter placement. Local analgesic agents are manufactured in more than one concentration and ampule size, which increases the potential for dosing errors.
Central Nervous System Toxicity
Early symptoms are those of stimulation but, as serum levels increase, depression follows. Symptoms may include light-headedness, dizziness, tinnitus, metallic taste, and numbness of the tongue and mouth. Patients may show bizarre behavior, slurred speech, muscle fasciculation and excitation, and ultimately, generalized convulsions, followed by loss of consciousness.
For management, the convulsions should be controlled, an airway established, and oxygen delivered. Succinylcholine abolishes the peripheral manifestations of the convulsions and allows tracheal intubation. Diazepam (Valium) can be used to inhibit convulsions. Magnesium sulfate, administered according to the regimen for eclampsia, also controls convulsions (Chap. 40, p. 758). Abnormal fetal heart rate patterns such as late decelerations or persistent bradycardia may develop from maternal hypoxia and lactic acidosis induced by convulsions. With arrest of convulsions, administration of oxygen, and application of other supportive measures, the fetus usually recovers more quickly in utero than following immediate cesarean delivery. Moreover, the mother is better served if delivery is forestalled until the intensity of hypoxia and metabolic acidosis has diminished.
Cardiovascular Toxicity
These manifestations generally develop later than those from cerebral toxicity, and they may not develop at all because they are induced by higher serum drug levels. The notable exception is bupivacaine, which is associated with the development of neurotoxicity and cardiotoxicity at virtually identical levels (Mulroy, 2002). Because of this risk of systemic toxicity, use of 0.75-percent solution of bupivacaine for epidural injection has been proscribed by the Food and Drug Administration. Similar to neurotoxicity, cardiovascular toxicity is characterized first by stimulation and then by depression. Accordingly, there is hypertension and tachycardia, which soon is followed by hypotension, cardiac arrhythmias, and impaired uteroplacental perfusion.
Hypotension is managed initially by turning the woman onto either side to avoid aortocaval compression. A crystalloid solution is infused rapidly along with intravenously administered ephedrine. Emergency cesarean delivery is considered if maternal vital signs have not been restored within 5 minutes of cardiac arrest (Chap. 47, p. 956). As with convulsions, however, the fetus is likely to recover more quickly in utero once maternal cardiac output is reestablished.
 Pudendal Block
Pudendal Block
Pain with vaginal delivery arises from stimuli from the lower genital tract. These are transmitted primarily through the pudendal nerve, the peripheral branches of which provide sensory innervation to the perineum, anus, vulva, and clitoris. The pudendal nerve passes beneath the posterior surface of the sacrospinous ligament just as the ligament attaches to the ischial spine. Sensory nerve fibers of the pudendal nerve are derived from ventral branches of the S2 through S4 nerves.
The pudendal nerve block is a relatively safe and simple method of providing analgesia for spontaneous delivery. As shown in Figure 25-2, a tubular introducer is used to sheath and guide a 15-cm 22-gauge needle into position over the pudendal nerve. The end of the introducer is placed against the vaginal mucosa just beneath the tip of the ischial spine. The introducer allows 1.0 to 1.5 cm of needle to protrude beyond its tip, and the needle is pushed beyond the introducer tip into the mucosa. A mucosal wheal is made with 1 mL of 1-percent lidocaine solution or an equivalent dose of another local anesthetic (see Table 25-3). To guard against intravascular infusion, aspiration is attempted before this and all subsequent injections. The needle is then advanced until it touches the sacrospinous ligament, which is infiltrated with 3 mL of lidocaine. The needle is advanced farther through the ligament. As it pierces the loose areolar tissue behind the ligament, the resistance of the plunger decreases. Another 3 mL of solution is injected into this region. Next, the needle is withdrawn into the introducer, which is moved to just above the ischial spine. The needle is inserted through the mucosa and 3 more mL is deposited. The procedure is then repeated on the other side.
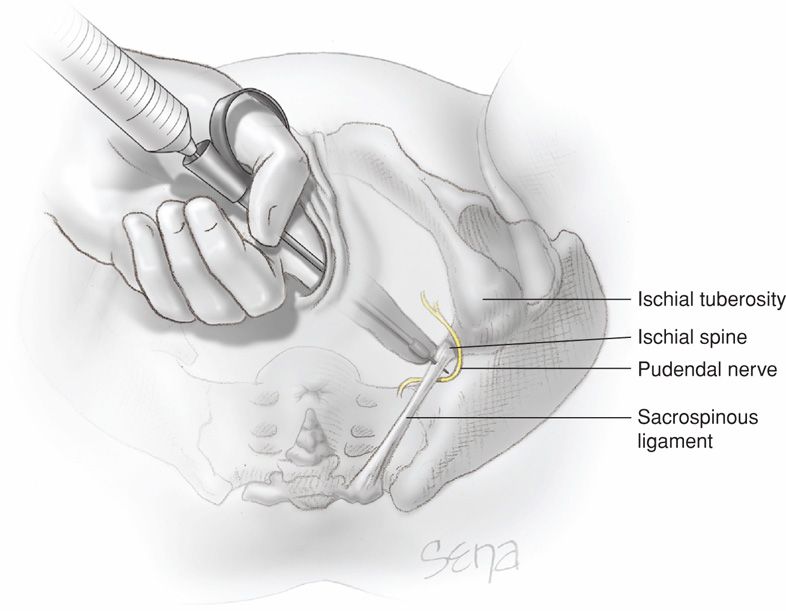
FIGURE 25-2 Local infiltration of the pudendal nerve. Transvaginal technique showing the needle extended beyond the needle guard and passing through the sacrospinous ligament to reach the pudendal nerve.
Within 3 to 4 minutes of injection, the successful pudendal block will allow pinching of the lower vagina and posterior vulva bilaterally without pain. If delivery occurs before the pudendal block becomes effective and an episiotomy is indicated, then the fourchette, perineum, and adjacent vagina can be infiltrated with 5 to 10 mL of 1-percent lidocaine solution directly at the planned episiotomy site. By the time of repair, the pudendal block usually has become effective.
Pudendal block usually does not provide adequate analgesia when delivery requires extensive obstetrical manipulation. Moreover, such analgesia is usually inadequate for women in whom complete visualization of the cervix and upper vagina or manual exploration of the uterine cavity is indicated.
Infrequently, complications may follow this block. As previously described, intravascular injection of a local anesthetic agent may cause serious systemic toxicity. Hematoma formation from perforation of a blood vessel is most likely when there is a coagulopathy (Lee, 2004). Rarely, severe infection may originate at the injection site. The infection may spread posteriorly to the hip joint, into the gluteal musculature, or into the retropsoas space (Svancarek, 1977).
 Paracervical Block
Paracervical Block
This block usually provides satisfactory pain relief during first-stage labor. However, because the pudendal nerves are not blocked, additional analgesia is required for delivery. For paracervical blockade, usually lidocaine or chloroprocaine, 5 to 10 mL of a 1-percent solution, is injected into the cervix laterally at 3 and 9 o’clock. Because these anesthetics are relatively short acting, paracervical block may have to be repeated during labor. We do not use it at Parkland Hospital.
Fetal bradycardia is a worrisome complication that occurs in approximately 15 percent of paracervical blocks (Rosen, 2002b). Bradycardia usually develops within 10 minutes and may last up to 30 minutes. Doppler studies have shown an increase in the pulsatility index of the uterine arteries following paracervical blockade (Chap. 10, p. 219). These observations support the hypothesis of drug-induced arterial vasospasm as a cause of fetal bradycardia (Manninen, 2000). For these reasons, paracervical block should not be used in situations of potential fetal compromise.
 Neuraxial Regional Blocks
Neuraxial Regional Blocks
Epidural, spinal, or combined spinal-epidural techniques were the more common methods used for relief of pain during labor and/or delivery in the United States in 2008 (Osterman, 2011b). Nearly two out of three mothers receive neuraxial anesthesia for relief of pain either during labor or during vaginal or cesarean delivery. Neuraxial techniques were more common in vaginal deliveries assisted by forceps—84 percent or vacuum extraction—77 percent than spontaneous vaginal deliveries—60 percent (Osterman, 2011a). Among first births, 68 percent of women delivered vaginally received neuraxial pain relief compared with 57 percent of women delivering their second or higher number child.
Epidural analgesia via a catheter as shown in Figure 25-3 is typically used for relief of labor pain, although it can also be used for anesthesia during operative vaginal and cesarean delivery. Spinal analgesia is typically given as a single intrathecal injection of a local anesthetic at the time of operative vaginal delivery or cesarean. Continuous spinal analgesia during labor via an indwelling spinal catheter is also under investigation. Combined spinal-epidural analgesia/anesthesia also illustrated in Figure 25-3 consists of a single intrathecal injection followed by a catheter placed into the epidural space for either patient- or provider-controlled infusion of a local anesthetic and/or an opioid such as fentanyl. The combined spinal-epidural technique has the advantages of immediate pain relief from the spinal injection coupled with a portal for continuous analgesia via the epidural catheter. Unlike the spinal injection, the relief provided by the epidural catheter takes approximately 30 minutes to become effective. Perhaps as many as a third of epidural catheter tips will migrate during labor, resulting in ineffective pain control should cesarean be necessary.
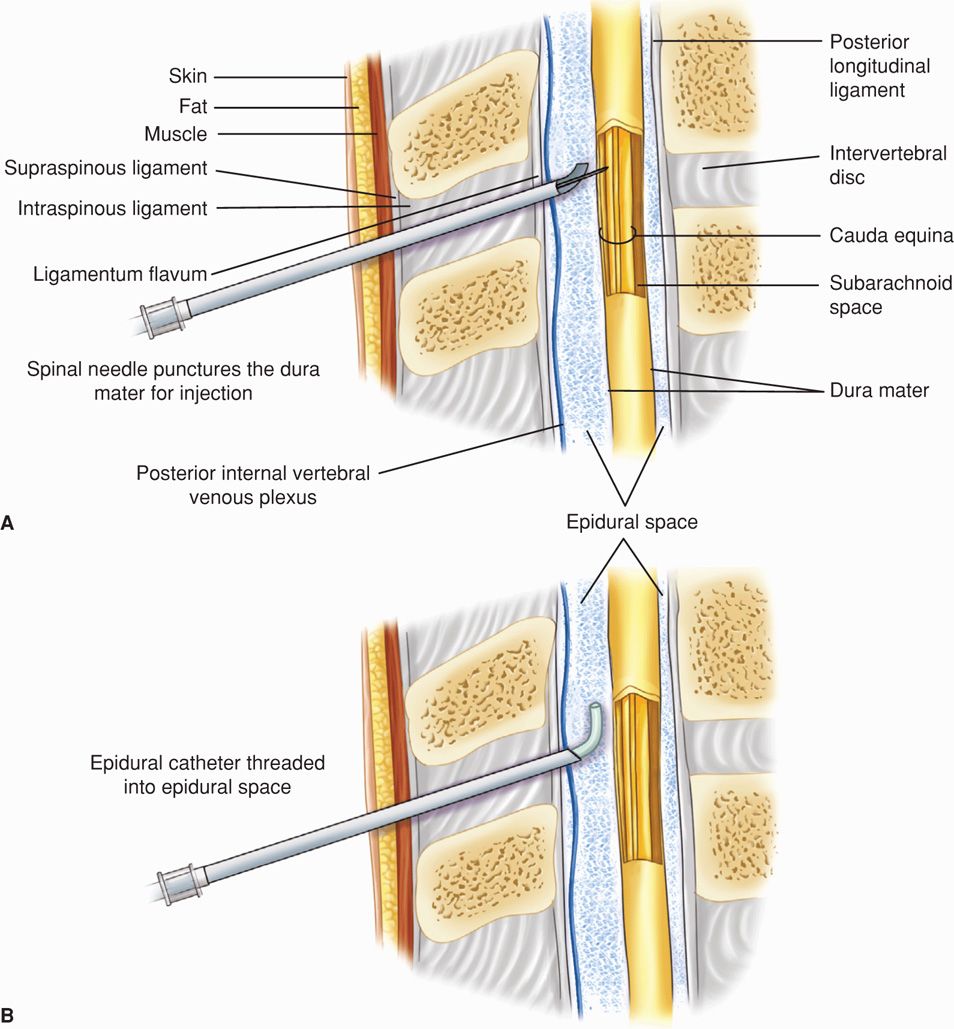
FIGURE 25-3 Neuraxial analgesia. A. Combined spinal-epidural analgesia. B. Epidural analgesia.
 Spinal (Subarachnoid) Block
Spinal (Subarachnoid) Block
Introduction of a local anesthetic into the subarachnoid space to effect analgesia has long been used for delivery. Advantages include a short procedure time, rapid blockade onset, and high success rate. Because of the smaller subarachnoid space during pregnancy, likely the consequence of internal vertebral venous plexus engorgement, the same amount of anesthetic agent in the same volume of solution produces a much higher blockade in parturients than in nonpregnant women.
Vaginal Delivery
Low spinal block can be used for operative vaginal delivery. The level of analgesia should extend to the T10 dermatome, which corresponds to the level of the umbilicus. Blockade to this level provides excellent relief from the pain of uterine contractions (Fig. 25-4).
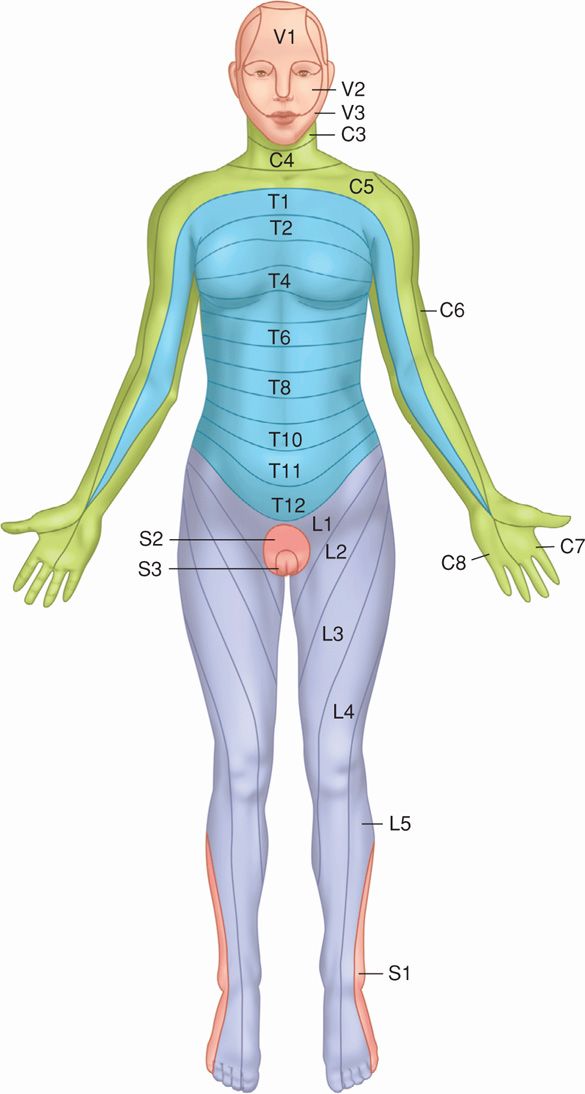
FIGURE 25-4 Dermatome distribution.
Several local anesthetic agents have been used for spinal analgesia (see Table 25-4). Addition of glucose to any of these agents creates a hyperbaric solution, which is heavier and denser than cerebrospinal fluid. A sitting position causes a hyperbaric solution to settle caudally, whereas a lateral position will have a greater effect on the dependent side. Lidocaine given in a hyperbaric solution produces excellent analgesia and has the advantage of a rapid onset and relatively short duration. Bupivacaine in an 8.25-percent dextrose solution provides satisfactory anesthesia to the lower vagina and the perineum for more than 1 hour. Neither is administered until the cervix is fully dilated, and all other criteria for safe forceps delivery have been fulfilled (Chap. 29, p. 575). Preanalgesic intravenous hydration with 1 L of crystalloid solution will prevent or minimize hypotension in many cases.
Cesarean Delivery
A level of sensory blockade extending to the T4 dermatome is desired for cesarean delivery (see Fig. 25-4). Depending on maternal size, 10 to 12 mg of bupivacaine in a hyperbaric solution or 50 to 75 mg of lidocaine hyperbaric solution are administered. The addition of 20 to 25 μg of fentanyl increases the rapidity of blockade onset and reduces shivering. The addition of 0.2 mg of morphine improves pain control during delivery and postoperatively.
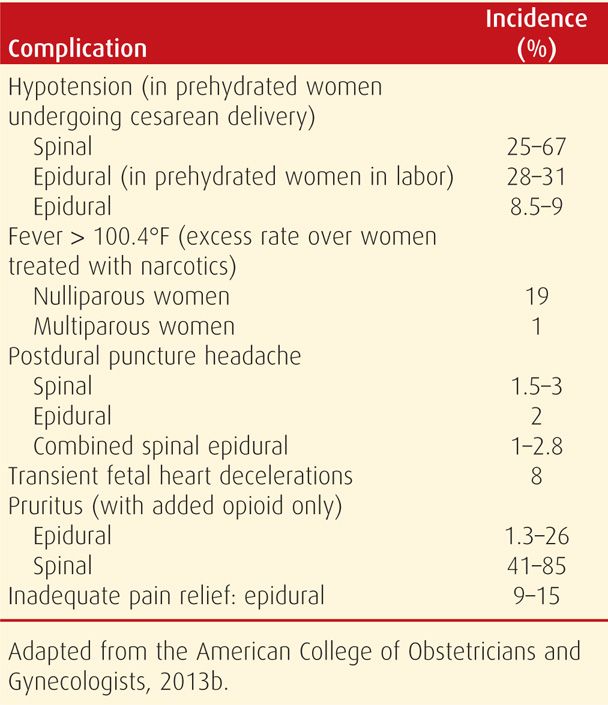
Complications
Shown in Table 25-5 are some of the more common complications associated with neuraxial analgesia. Importantly, obese women have significantly impaired ventilation and thus close clinical monitoring is imperative (Vricella, 2011).
TABLE 25-5. Complications of Regional Analgesia
Hypotension. This common complication may develop soon after injection of the local anesthetic agent. It is the consequence of vasodilatation from sympathetic blockade and is compounded by obstructed venous return due to uterine compression of the great vessels. In the supine position, even in the absence of maternal hypotension measured in the brachial artery, placental blood flow may still be significantly reduced. Treatment includes uterine displacement by left lateral patient positioning, intravenous crystalloid hydration, and intravenous bolus injections of ephedrine or phenylephrine.
Ephedrine is a sympathomimetic drug that binds to alpha- and beta-receptors but also indirectly enhances norepinephrine release. It raises blood pressure by increasing heart rate and cardiac output and by variably elevating peripheral vascular resistance. In animal studies, ephedrine preserves uteroplacental blood flow during pregnancy compared with alpha1-receptor agonists. Accordingly, it is a preferred vasopressor for obstetrical use. Phenylephrine is a pure alpha agonist and raises blood pressure solely through vasoconstriction. A metaanalysis of seven randomized trials by Lee (2002a) suggests that the safety profiles of ephedrine and phenylephrine are comparable. Following their systematic review of 14 reports, Lee (2002b) questioned whether routine prophylactic ephedrine is needed for elective cesarean delivery. But although fetal acidemia has been reported with prophylactic ephedrine use, this was not observed with prophylactic phenylephrine use (Ngan Kee, 2004).
Hypotension is the more common blood pressure perturbation. However, paradoxically, hypertension from ergonovine or methylergonovine injections following delivery is more common in women who have received a spinal or epidural block.
High Spinal Blockade. Most often, complete spinal blockade follows administration of an excessive dose of local anesthetic. This is certainly not always the case, because accidental total spinal block has even occurred following an epidural test dose. With complete spinal blockade, hypotension and apnea promptly develop and must be immediately treated to prevent cardiac arrest. In the undelivered woman: (1) the uterus is immediately displaced laterally to minimize aortocaval compression, (2) effective ventilation is established, preferably with tracheal intubation, and (3) intravenous fluids and ephedrine are given to correct hypotension.
Postdural Puncture Headache. Leakage of cerebrospinal fluid (CSF) from the meningeal puncture site can lead to postdural puncture or “spinal headache.” Presumably, when the woman sits or stands, the diminished CSF volume creates traction on pain-sensitive central nervous system structures.
Rates of this complication can be reduced by using a small-gauge spinal needle and avoiding multiple punctures. In a prospective, randomized study of five different spinal needles, Vallejo and associates (2000) concluded that Sprotte and Whitacre needles had the lowest risks of postdural puncture headaches. Sprigge and Harper (2008) reported that the incidence of postdural puncture headache was 1 percent in more than 5000 women undergoing spinal analgesia. Postdural puncture headaches are much less frequent with epidural blockade because the dura is not intentionally punctured. The incidence of inadvertent dural puncture with epidural analgesia approximates 0.2 percent (Introna, 2012; Katircioglu, 2008). There is no good evidence that placing a woman absolutely flat on her back for several hours is effective in preventing headache. Vigorous hydration may be of value, but compelling evidence to support its use is also lacking.
If a headache develops, the administration of caffeine, a cerebral vasoconstrictor, has been shown in randomized studies to afford temporary relief (Camann, 1990). With severe headache, an epidural blood patch is most effective. Ten to 20 mL of autologous blood are obtained aseptically by venipuncture into a tube without anticoagulant. This blood is then injected into the epidural space at the site of dural puncture. Further CSF leakage is halted by either mass effect or coagulation. Relief is immediate, and complications are uncommon. In a randomized trial of 64 women, Scavone and coworkers (2004) found that prophylactic blood patch did not decrease either the incidence of postdural puncture headache or the need for a subsequent therapeutic blood patch.
If a headache does not have the pathognomonic postural characteristics or persists despite treatment with a blood patch, other diagnoses should be considered. For example, Chisholm and Campbell (2001) described a case of superior sagittal sinus thrombosis that manifested as a postural headache. Chan and Paech (2004) have described persistent CSF leak in three women. Smarkusky and colleagues (2006) described pneumocephalus, which caused immediate cephalgia. Finally, intracranial and intraspinal subarachnoid hematomas have developed after spinal analgesia (Dawley, 2009; Liu, 2008).
Convulsions. In rare instances, postdural puncture cephalgia is associated with temporary blindness and convulsions. Shearer and associates (1995) described eight such cases associated with 19,000 regional analgesic procedures done at Parkland Hospital. It is presumed that these too are caused by CSF hypotension. Immediate treatment of seizures and blood patch was usually effective in these cases.
Bladder Dysfunction. With spinal analgesia, bladder sensation is likely to be obtunded and bladder emptying impaired for several hours after delivery. As a consequence, bladder distention is a frequent postpartum complication, especially if appreciable volumes of intravenous fluid are given. Millet (2012) randomized 146 women with neuraxial analgesia to either intermittent or continuous bladder catheterizations and found that the intermittent method was associated with significantly higher rates of bacteriuria.
Arachnoiditis and Meningitis. Local anesthetics are no longer preserved in alcohol, formalin, or other toxic solutes, and disposable equipment is used by most. These practices, coupled with aseptic technique, have made meningitis and arachnoiditis rare but have not eliminated them (Centers for Disease Control and Prevention, 2010).
Contraindications to Spinal Analgesia
Shown in Table 25-6 are the absolute contraindications to regional analgesia according to the American College of Obstetricians and Gynecologists (2013b). Obstetrical complications that are associated with maternal hypovolemia and hypotension—for example, severe hemorrhage—are contraindications to spinal blockade. The additive cardiovascular effects of spinal blockade in the presence of acute blood loss in nonpregnant patients were documented by Kennedy and coworkers (1968).
TABLE 25-6. Absolute Contraindications to Neuraxial Analgesia
Refractory maternal hypotension
Maternal coagulopathy
Thrombocytopenia (variously defined)
Low-molecular-weight heparin within 12 hours
Untreated maternal bacteremia
Skin infection over site of needle placement
Increased intracranial pressure caused by a mass lesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


