• Review of current meds & allergies: Discuss holding NSAIDs, antiplatelet agents, anticoagulant supplements (eg, fish oil); consider bridging long-acting anticoagulants to shorter acting meds (eg, warfarin to heparin)
• Review relevant prior operative reports.
• Most healthy women w/ no identifiable RFs require no further testing or consultation.
• Consider ECG in women >50 y. Depending on invasiveness & urgency of procedure, periop eval by PCP ± anesthesia or other specialist is recommended. Additional testing based on identified risk.
• Informed consent, w/ balanced discussion of:
Risks, benefits, alternatives (including nontreatment & poss additional procedures), & complications.
Healthcare team & their roles including trainee & supportive teams
Permission to take photos or videos for documentation or teaching
Possibility of bld or bld product use
• Identify existing advance directive & healthcare proxy/power of attorney. Consider creating an advance directive if one does not already exist.
• Discuss expected postop course (hospital stay, recovery, change in fxn, etc.)
• Identify special needs for OR (eg, interpreter services)
Perioperative Optimization
• New or uncontrolled medical conditions → consultation/optimization w/ appropriate specialist + primary care input.
• Pulm dz:
RFs = older age, current smoking, obesity, obstructive sleep apnea, low serum albumin (<3 g/dL) & BUN >30 mg/dL, higher ASA scores are a/w higher risk for postop pulm complications (Ann Surg 2000;232:242; Ann Intern Med 2006;144(8):581).
Well-controlled asthma not a/w pulm postop complications
Advise smoking cessation >8 w before elective Surg (if <8 w, no dec in pulm complications)
Preop PFTs/CXR if unexplained dyspnea or respiratory sx; consider if COPD of unclear severity.
Postoperatively: Deep breathing exercise, incentive spirometry, early ambulation, upright position, & adequate pain control after Surg are effective in preventing postop pulm complications.
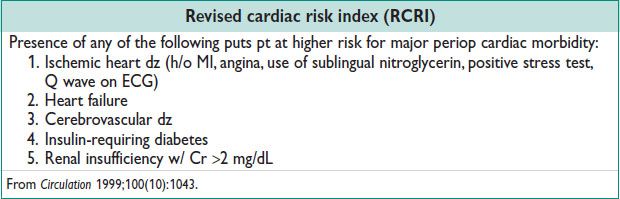
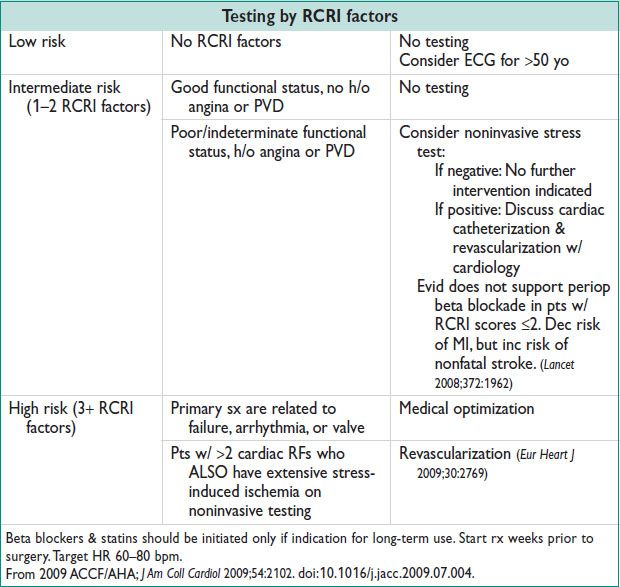
• Cardiovascular dz:
Most abdominal/pelvic Surg is considered as an intermediate risk regarding cardiac morbidity
Selected procedures may be of low risk (eg, D&C) or high risk (major debulking Surg)
Nonemergent Surg should be delayed or cancelled if pt has (1) unstable coronary syns, (2) decompensated heart failure, (3) signif arrhythmia, or (4) sev valvular dz.
• Hematology:
Anemia: Investigate if unexplained; correct anemia w/ iron suppl if there is time before Surg or transfuse if Hgb <7 g/dL, symptomatic, or for high anticipated bld loss. Consider menstrual suppression if menorrhagia is a contributing factor. Consider erythropoiesis-stimulating agents if xfusion is refused.
Thrombocytopenia: Goal is Plts >50000
Pt on anticoagulation:
Determine risk of stopping anticoagulation perioperatively. Stop warfarin 5 d prior to procedure, goal INR <1.5. Consider heparin bridge if at high risk of thrombosis.
Avoid elective Surg w/i 1 mo of acute venous or arterial thrombosis
Consider IVC filter if recent thrombosis & high risk of bleeding w/ anticoag
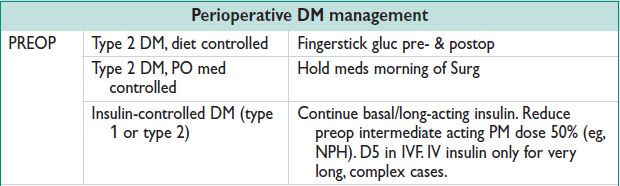
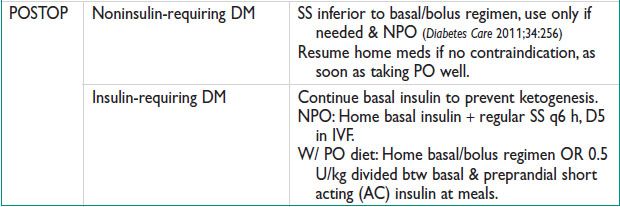
• Endocrine:
DM:
Periop gluc problems: (1) surgical stress, (2) preop NPO, (3) decreased PO postop, (4) type of anesthesia (general > neuraxial). Critical considerations: (1) type 1, type 2, or gestational diabetes; (2) timing, length, & invasiveness of procedure; (3) current med regimen.
Poor periop gluc control a/w (1) increased risk of infxn, (2) poor wound healing, (3) neuro/cardiac sequelae of hypoglycemia. Postop goals: Maintain euglycemia (<150–180 mg/dL) & prevent ketoacidosis & nonketotic hyperosmolar state.
Metformin contraindicated w/ renal insufficiency or poor tissue perfusion; thiazolidinediones may exacerb edema or precipitate CHF.
• Thyroid dz:
Hyperthyroid: If new dx or uncontrolled, postpone Surg, consult endocrinology, continue chronic meds.
Hypothyroid: Consider endocrinology consult if new dx. Otherwise, continue meds. No need for IV/IM thyroid replacement if NPO for <7 d.
For hypo- & hyperparathyroidism: Follow for calcium imbalance
• Adrenal insufficiency:
Higher risk for periop adrenal crisis (HoTN, HoNa)
Minimal suppression of the HPA axis in pts w/ <5 mg prednisone (or equiv) daily; <10 mg prednisone every other day; or ANY dose of glucocorticoid for <3 w. These pts do not require supplemental steroids (N Engl J Med 2003;348:727).
Replacement based on type of Surg (JAMA 2002;287:236):
Minor Surg (outpt Surg or minimally invasive): → consider 25 mg hydrocortisone on day of procedure → pt returns to regular dose.
Obstetric cases & all gynecologic Surg: → 50 mg hydrocortisone just before procedure → followed by 25 mg IV every 8 h for 24 h → back to maint dose
For sev surgical stress (consider in extensive debulking surgeries): 100–150 mg hydrocortisone on day of procedure → rapid taper to usual dose over 1–2 d
Critically ill pts (septic shock): → 50–100 mg hydrocortisone IV q6–8 h or 0.18 mg/kg/h as a continuous infusion & 50 μg/d fludrocortisone until shock is resolved → taper slowly (monit sodium).
• Elderly pts:
Polypharmacy: Carefully review meds & potential interactions
Avoid bowel prep due to higher risk of dehyd/electrolyte derangement
Higher risk for the following postoperatively (Am J Obstet Gynecol 2003;189:1584)
Delirium & mental status changes; ensure sleep hygiene, orientation to environment & careful dosing of psychoactive meds. W/u medical causes of delirium.
Pulm edema w/ heart failure due to fluid overload; monit fluid balance
MI & stroke
Slow return of bowel fxn
Longer hospital stay
• Obese pts:
Higher risk for the following postoperatively (Am J Obstet Gynecol 2010;202:306):
SSI; plan incision & dose Abx appropriately
Pulm complications; encourage early ambulation & pulm toilet
Thromboembolic complication; consider weight-based anticoagulant dosing per pharmacy guidelines
Preoperative Measures
• Preg test: For ALL women of reproductive age
• Bld type & Ab screen: Consider cross-match for high-risk surgeries
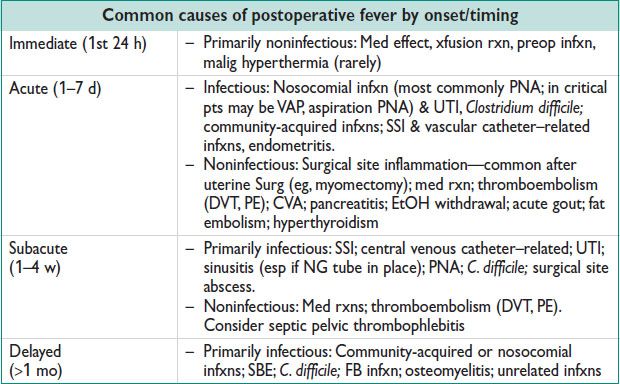
• Antibiotic ppx for prevention of SSI: See below
• Antibiotic ppx for prevention of SBE:
Not routinely recommended for GU procedures. Used in women w/ highest potential risk (prosthetic valve, prev infective endocarditis, pt w/ unrepaired cyanotic heart dz, repaired heart dz w/i 6 mo of procedure, or repaired dz w/ residual defects near prosthetic material, cardiac xplant w/ signif valvular dysfxn) (Circulation 2008;118(8):887).
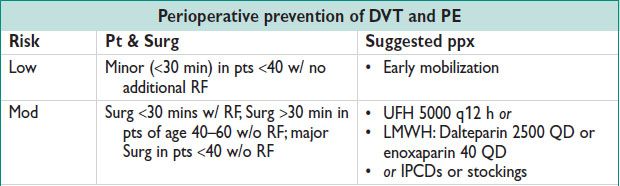
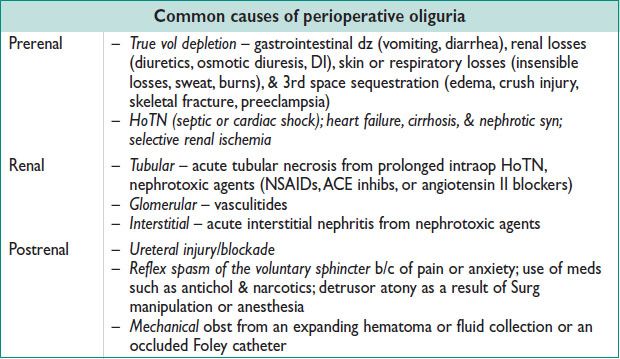
• Venous thromboembolism ppx: See below
• Bowel prep: Mechanical bowel preparation (eg, magnesium citrate, polyethylene glycol) not recommended for most gynecologic or colorectal Surg (Am J Obstet Gynecol 2011;205:309).
• Fasting: Preop NPO reduces aspiration risk. Milk or fried/fatty food: 8 h; light meal not including milk: 6 h; clear fluids: 2 h (Anesthesiology 2011;114:495).
• Skin prep: SSI, see below
• Positioning & incision selection: Neurologically neutral positioning & padding of all jnts. Avoid prolonged lithotomy (>4 h) or steep Trendelenburg. Select incision for appropriate exposure & to avoid excessive retraction.
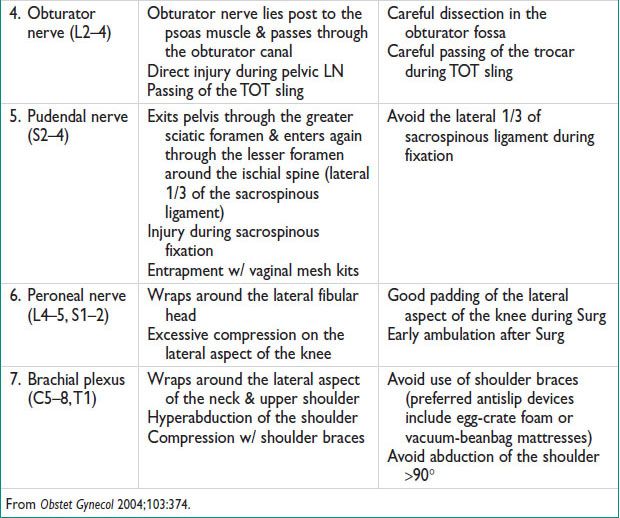
POSTOPERATIVE FEVER
Definitions
• Nml temperature ranges from 36.5–37.5°C
• Fever defined as temperature >38.0°C or >100.4°F.
Workup
• Hx: Review records for preop infxn, intraop complications, xfusion, med list, allergies, urinary catheter, vascular access sites. Ask about diarrhea, productive cough, skin rash, new onset pain, sputum, preop illness.
• Physical exam: Temperature (& trends), pulse, bld pres, & respiratory rate. Examine skin (rash), lungs (decreased breath sounds, rales, rhonchi), heart (new murmurs), abd (tenderness or peritoneal signs), operative site (including vaginal cuff, poss), catheter/drain/IV sites, & lower extremities (DVT).
• Lab: Based on Hx, exam, & diff. May include urinalysis & culture, CBC w/ diff, bld culture ×2 before Abx (1 set from indwelling central line if present), sputum culture (generally low yield), wound culture (low yield), CXR, lower limb US for DVT, & PE protocol CT scan. W/u for other medical conditions as appropriate.
• Mgmt: Based on etiology, if Abx indicated, target to suspected sources; tailor to culture results when available
SURGICAL SITE INFECTIONS (SSI)
Definition, Microbiology, and Epidemiology
• SSI introduced at time of Surg by endogenous flora
• Common organisms: Staphylococcus aureus, enterococcus, Escherichia coli, coagulase-negative staphylococci. Gyn SSI more likely caused by gram-negative bacilli, enterococci, group B streptococcus, anaerobes
• Infxn rate by category of procedure: Clean 2.6%, clean-contaminated 3.6%, contaminated/dirty 10.5% (Arch Surg 1999;134:1041)
• RFs: Obesity, existing infxn, diabetes, smoking, corticosteroids, immunosuppression, poor nutrition, long duration of Surg, active bact vaginosis or cervicitis
Prophylaxis (Infect Control Hosp Epidemiol 2008 29:S51)
• Skin prep: Chlorhexidine-alcohol superior to povidone-iodine (NEJM 2010;362:18)
• Sterile technique, avoid razor hair removal (trim/clip instead), avoid hyperglycemia
• Antimicrobial ppx: (Am J Obstet Gynecol 2008;199:301.e1, Obstet Gynecol 2009;113:1180.)
Administer <30 min before Surg (Ann Surg 2009;250:10), or at time of anesthesia
Additional dose may be req for obese pts, Surg >4 h or EBL >1500 mL
Clinical Manifestations (Infect Control Hosp Epidemiol 1992; 13:606; Infect Dis Obstet Gynecol 2003;11:65)
• Incision cellulitis: Warmth, swelling, erythema, pain w/o fluid collection
• Superficial incisional SSI (skin, subcutaneous tissue): Positive cx, purulent drainage
• Deep incisional SSI (fascia, muscle): Spont dehiscence, abscess
• Vaginal cuff cellulitis: Edema, induration, & erythema of the vaginal cuff
• Organ space: Pelvic abscess, vaginal cuff abscess
• Nec fasciitis: Erythema, swelling/edema, pain disproportionate to exam (followed by analgesia), crepitus, gray-colored discharge
Workup
• CBC (leukocytosis ± bandemia), gram stain + cx of incision or abscess fluid, bld culture
• US: Inexpensive, sens 56–93%, spec 86–98% for pelvic abscess (J Emerg Med 2011;40:170)
• CT: Abscess characterized by multilocular (89%), thick enhancing wall (95%) (J Reprod Med 2005;50(3):203)
Treatment
• Incisional cellulitis: Antimicrobial rx w/ gram-positive coverage, consider MRSA coverage
• For more complicated SSI: Parenteral antibiotic therapy ± abscess drainage
• Nec fasciitis: Emergent wide local debridement + beta-lactam/beta-lactamase inhib + clindamycin (antitoxin effect) + MRSA coverage
PERIOPERATIVE DVT/PE
Definition and Epidemiology
• VTE: DVT & PE are common periop complications. See Chapter 16 for full details on diagnosis and management.
• Rates of postsurgical VTE w/o rx: 29% for benign Gyn & 38% for Gyn oncology (Br Med J 1978;1:272; Aust N Z J Obstet Gynecol 1983;23:216)
SEPSIS
Definitions (Crit Care Med 2003;31(4):1250)
• SIRS: 2+ of the following: (1) temp >38 OR <36°C, (2) HR >90 bpm, (3) RR >24/min or arterial CO2 <32 mm Hg or mechanical vent, (4) WBC >12 K/mm3 or <4 K/mm3 or >10% immature forms
• Sepsis: SIRS + documented infxn
• Sev sepsis: Sepsis + sign(s) of organ hypoperfusion/dysfxn including oliguria, metabolic acidosis, abrupt AMS, thrombocytopenia or DIC, cardiac dysfxn, acute lung injury
• Septic shock: Sev sepsis w/ HoTN despite adequate fluid resusc or need for vasopressors to maintain BP.
Epidemiology (NEJM 2003 348:16)
• Incid: 240 cases per 100000, 9% annual ↑ from 1979–2000
• Rate of sev postop sepsis 0.9%, mortality 34% (Anesthesiology 2010;112:917)
• Sepsis: Amplified, uncontrolled, self-sustaining intravascular inflamm response
Bact wall components (endotoxin, LPS) & products (exotoxins) activate host defense
Initial excessive resp of inflamm mediators (TNFα & IL-1). Activation of coagulation cascade & enhanced formation of microvascular thrombi. Impaired tissue oxygenation & tissue damage. Late shift to anti-inflammatory immunosuppressive state → inability to clear infxn.
Clinical Manifestations
• HoTN, initial ↑ cardiac output, but eventual systolic & diastolic failure
• AMS (encephalopathy): Agitation, confusion, obtundation
• Acute renal failure due to hypoperfusion/hypoxia: Oliguria, electrolyte abnormalities
• Pulm edema → V/Q mismatch → hypoxemia → ARDS
Workup
• Obtain appropriate cx (eg, bld, urine, wound, catheter tip)
• CXR to assess acute lung injury & ARDS (diffuse bilateral infiltrates)
• Imaging studies (eg, CT) to confirm infxn site & sample poss source
Management (Crit Care Med 2008;36:296; see also www.survivingsepsis.org)
• Identify infectious source
• Early respiratory stabilization: Pulse oximetry, mechanical ventilation as needed
• Adequate access: CVC if sev sepsis or shock
• Aggressive fluid resusc: Crystalloid or colloid, necessary to prevent organ dysfxn
Goals: CVP ≥8 mm Hg (12 mm Hg if ventilated), MAP ≥65% mm Hg, UOP ≥5 mL/kg/h
• IV Abx: Begin as soon as poss after cx are collected. Broad spectrum: Directed at most likely pathogens of presumed source.
• Vasopressors: If BP not responsive to IV fluid administration, use to maintain MAP >65 mm Hg (norepinephrine generally 1st line. Alternatives include phenylephrine, epinephrine, vasopressin, dopamine)
• Corticosteroids: Consider hydrocortisone IV (for adrenal insufficiency) if BPs unresponsive to fluid resusc.
• Sepsis bundles:
Initial resusc bundle: All w/i 6 h of identification of sev sepsis
Measure serum lactate
Obtain bld cx prior to Abx (2 sets of bld cxs, other indicated site)
Broad-spectrum Abx w/i 1 h
If HoTN &/or lactate >4 mmol/L → fluids + vasopressors to goal MAP >65 mm Hg
If persistent HoTN despite fluid resusc (septic shock) → maintain CVP ≥8 mm Hg & ScvO2 ≥70% or SvO2 ≥65%
Subseq mgmt bundle: W/i 24 h includes ventilator mgmt of ARDS, bld products, steroids, vasopressors, sedation, maintaining euglycemia, renal replacement therapy, & mgmt of multiorgan dysfxn
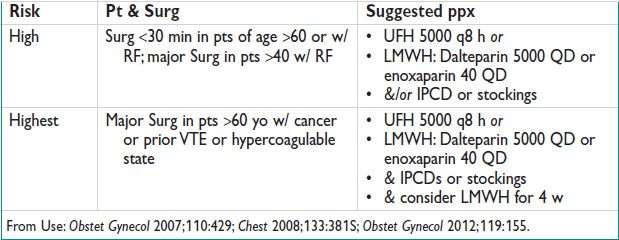
PERIOPERATIVE OLIGURIA
Definitions
• Generally, urine output of <30 mL/h for 2–3 h or <500 mL/d
• According to RIFLE criteria for AKI (Crit Care 2007:11R31)
Risk: UOP <0.5 mL/kg/h for 6–12 h; or Cr ↑ 1.5×
Injury: UOP <0.5 mL/kg/h for >12 h; or Cr ↑ 2×
Failure: UOP <0.3 mL/kg/h for >24 h or anuria for 12 h; or Cr ↑ 3×, or Cr >4 w/ acute rise >0.5 mg/dL
Loss: Persistent AKI w/ loss of kidney fxn >4 w
End stage: >3 mo of loss of kidney fxn
Workup
• History & physical exam
• Check the Foley catheter & irrigate as a 1st step.
• Check meds & hold/replace NSAIDs & other nephrotoxic meds. Consider renally dosing other meds as needed.
• Review operative report & anesthesia record: Intraop I/Os & BP
• Labs
Urinalysis w/ review of sediment for muddy brown, granular casts (ATN) & eos (interstitial nephritis)
CBC, Cr, serum electrolytes & urinary electrolytes/Cr
Serum BUN/Cr: Ratio >20 generally sugg prerenal dz
FENa: <1% in prerenal dz & >2% in intrinsic renal dz. Consider FEurea if recent use of diuretics.
• Renal US: Postrenal obst, chronic renal dz
Management
• Prerenal: Fluid challenge of 500–1000 cc of crystalloid. Cr resolves in 1–3 d.
• Renal: Identification & rx of underlying cause
• Postrenal:
Acute retention: Transurethral or suprapubic catheter
Ureteric/bladder injuries: Consider percutaneous nephrostomy tube, trial of stenting (antegrade or retrograde) followed by delayed repair. Drain if urinoma.
POSTOPERATIVE ILEUS
Definition
• Obstipation w/ intolerance to oral intake due to postop intestinal dysmotility.
• Physiologic ileus can last 1–3 d postop depending on procedure. Longer duration may be abnl.
Etiology
• Inhibition of nml motility by postop inflammation, inhibition of spinal reflexes, opioids, vasoactive intestinal polypeptide, substance P, nitric oxide
Clinical Manifestations
• Inability to tolerate PO diet, abdominal pain, distention, tympany on exam, decreased bowel sounds, delayed/decreased flatus
Diagnosis
• Generally clinical, though should rule out small bowel obst (see below).
• Intestinal dilatation w/o evid of transition point on CT, XR imaging of abd.
Treatment
• Bowel rest, NG tube if necessary. Vol resusc, repletion of electrolytes PRN.
• Reduce/eliminate aggravating med (eg, opioids)
• Serial abdominal exams until abdominal decomp/flatus.
Prevention
• Epidural + local anesthesia instead of systemic or epidural opioids (Cochrane Database Syst Rev 2000;(4):CD001893)
• Alvimopan (selective opioid receptor antag) postop. FDA has limited access to med as may inc risk MI in some pts.
• Gum chewing immediately postop (World J Surg 2009;33(12):2557)
• Scheduled postop laxative use after hysterectomy (Am J Obstet Gynecol 2007;196(4):311.e1)
• Minimal manipulation of bowel intraop
• Routine NG tube placement is NOT indicated (Cochrane Database Syst Rev 2007 18;(3):CD004929)
BOWEL OBSTRUCTION
Definition
• Failure of intestinal contents to progress normally through the small bowel.
Etiology
• Adhesive dz, malig, hernia most likely. Up to 42% of women w/ ovarian cancer (Ann Oncol 1993;4(1):15)
• Stricture (eg, postradiation or from Crohn’s dz), intussusception, volvulus, gallstone ileus less likely
Clinical Manifestations
• Nausea, vomiting (± feculent), crampy abdominal pain, inability to tolerate PO
• Extent of abdominal distention may depend on site of obst
• Generally unable to pass flatus as sx progress
• May be clinically hypovolemic
• Peritoneal signs may indicate ischemic bowel or perforation
Diagnosis
• Radiographic evid (XR, CT) of “transition point” w/ prox dilatation & distal decomp of bowel.
• CT more sensitive for signs of bowel ischemia/strangulation, perforation, closed loop (prox + distal) obst, hernia, additional intra-abdominal pathology.
• Consider lactate for biochemical evid of ischemia a/w SBO.
Treatment
• Conservative measures include bowel rest, NG tube to low suction for decomp, vol resusc & electrolyte repletion PRN. TPN if indicated.
• Consider therapeutic use of Gastrografin (water-soluble contrast) (World J Surg 2008;32(10):2293)
• Consider medical rx w/ octreotide for pts w/ advanced ovarian cancer (Cochrane Database Syst Rev 2010;(7):CD007792)
• Exploratory laparotomy if concern for strangulation/ischemia, perforation, early SBO after laparoscopic Surg w/ concern for port site hernia, failure of conservative mgmt.
• NG tube may be removed if (1) passage of flatus or stool, (2) residual vol of gastric contents <100 cc after 4 h clamped.
Large-bowel Obstruction
• In gynecologic Surg, most often related to malig
• Unlikely to respond to conservative mgmt
• Rx options include colostomy creation or endoscopic stent, depending on location & clinical situation.
COMPLICATIONS OF LAPAROSCOPY
Incidence (Clin Obstet Gynecol 2002;45(2):469)
• Occur in 0.2–10.3% of all laparoscopic cases
• Over 50% during entry into the abdominal cavity
Complications of Laparoscopy (J Minimally Invasive Gynecol 2006;13:352)
• Extraperitoneal insufflation: Misplacement of Veress needle → peritoneal tenting
Signs: Immediate insufflation pres >15 mm Hg, abdominal wall fullness/crepitus, hypercarbia, respiratory compromise
Prevention: Monit of insufflation pres, reposition Veress needle as appropriate.
Mgmt: Alert anesthesiologist, should resolve w/ expectant mgmt.
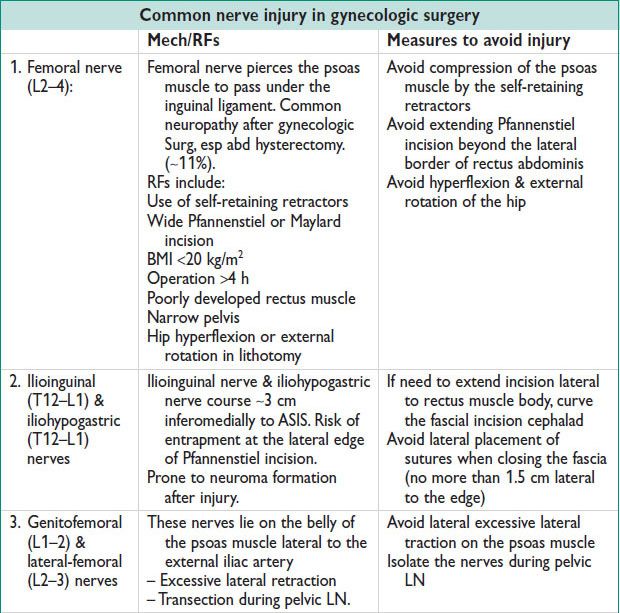
• Nerve injury: See table with summary above.
• Vascular injury: During entry (Veress needle or port placement) or intraop
Common vessels injured: Inferior/superior epigastric artery, aorta, vena cava, iliac vessels
Signs: Port site bleeding, intra-abdominal bleeding on entry, tachy, HoTN
Prevention: Correct needle placement & direct visualization of trocar sites
Open (Hasson) entry may minimize vascular injury risk (Aust N Z J Obstet Gynecol 2002;42:246)
Manage: Small vessels → tamponade or ligation, large vessels → laparotomy, abdominal packing & fluids if vascular surgeon not immediately available (J Min Invas Gynecol 2010;17:692)
• GI injury: Incid 13/1000, occurs during entry or intraop (Br J Surg 2004;91:1253)
Signs: If not recognized intraop, worsening abdominal pain, tachy, fever
Intraperitoneal air not reliable sign, occurs in 38.5% laparoscopy (J Reprod Med 1976;16(3):119)
RFs: Prior Surg, intra-abdominal pathology (endometriosis, PID, adhesions)
Prevention: NG or OG tube decomp of stomach. In high-risk pts consider nonumbilical entry point (Palmer’s point –3 cm below costal margin in left midclavicular line).
Mgmt: Surgical repair (oversewing or resxn), Abx
• Postop bleeding:
Signs: Tachy, > expected Hgb/Hct drop, HoTN, oliguria, AMS, increased abdominal pain, bleeding from incision or vagina
Abd compartment syn: Bleeding/ascites → ↑ intra-abdominal pres → ↓ lung compliance, ↓ venous return, ↓ kidney fxn → hypoxemia, oliguria, renal failure
Manage: Fluid resusc, monit UOP, NPO, trend CBC, poss surgical exploration
• Urinary tract injury: Incid in TLH up to 4% (JSLS 2007;11:422; AJOG 2003;188(5):1273)
Only 30% recognized during operation
Signs: Abdominal/flank pain, peritonitis, hematuria, oliguria/anuria, fever, leakage of urine from incision or vagina, elevated Cr. Consider CT ± urogram, sampling free fluid in abd if suspect urinoma; send fluid for BUN/Cr. If close to serum, then transudate (ascites); if higher, suspect urine leak.
Prevention: Decomp of bladder w/ foley, direct visualization during trocar placement, dissection & visualization of ureters (peristalsis), routine stenting not recommended
Mgmt: Closure for large cystotomy, postop bladder decomp, ureter repair
• Trocar site hernia: Incid 0.5% (Br J Surg 2012;99:315)
Signs: Bulging, small-bowel obst
RFs: Pyramidal trocars, size ≥12-mm trocars (3% vs. <1%) (AJOG 1993;168:1493)
Prevention: Close port defects >10 mm (Arch Surg 2004;139:1246)
Mgmt: Surgical vs. expectant depending on severity
• Shoulder pain: Common, referred pain from diaphragmatic irritation (CO2, bld, fluid)
COMPLICATIONS OF HYSTEROSCOPY
Complications and management (Obstet Gynecol 2011;117:1486; Best Pract Res Clin Obstet Gynaecol 2009;23:619)
• Fluid overload (5–6%): Excessive intrauterine Absorp of distending media
Main types of distending fluid:
Nonelectrolyte (glycine, mannitol, sorbitol): For use w/ monopolar instruments
Electrolyte (saline, LR): For diagnostic hysteroscopy & w/ bipolar or mechanical instruments
Pathophysiology: Vol overload: CHF, pulm edema; metabolic imbalance: HypoNa, ↓ serum osm, ↑ ammonemia, hyperglycemia, acidosis; ↓serum Na by ∼10 mmol/L/1000 mL glycine deficit (Lancet 1994:344:1187); neurologic sequelae: Cerebral edema, nausea, visual changes, sz, coma. Prevent overload: Select distending media that minimizes risk of overload (isotonic, electrolyte-containing solutions), monit fluid deficit frequently, use automated fluid monitoring system.
Manage: D/c infusion for (J Am Assoc Gynecol Laparosc 2000;7:167)
Nonelectrolyte solution >1000–1500 mL
Electrolyte solution >2500 mL
OR serum Na <130 mmol/L
If severely hyponatremic → hypertonic saline. Loop diuretics are not indicated unless there is clinical evid for vol overload; may exacerb electrolyte abnormalities. Low threshold for xfer to ICU for intensive monitoring.
• Hemorrhage (2–3%): From resection, cervical lacerations, tenaculum site, perforation
Manage: Electrocautery, inject vasopressin, suturing tenaculum site, balloon tamponade (AJOG 1983;147:869), laparoscopic suturing, hysterectomy, UAE
• Uterine perforation (1–1.5%) → retroperitoneal hematoma, bowel/bladder injury, or signs of acute bld loss
Prevention: Careful sounding, adequate cervical dilation, operate resectoscope toward user (not toward uterine wall)
Mgmt:
Hemodynamically stable → monit for bleeding, pain, infxn
Large perforation, unstable or perforation w/ electrocautery → surgical exploration w/ repair
• Infxn: Rare complication of hysteroscopy (<1%)
• Air/CO2 embolization (gas rarely used as distention medium) → circulatory collapse (sudden ↓ O2 sat, ↓ BP, dysrhythmia). Place pt in left lateral decubitus w/ head tilted down, cardiopulmonary support.
< div class='tao-gold-member'>



