Chapter 8 Normal Labor, Delivery, and Postpartum Care
ANATOMIC CONSIDERATIONS, OBSTETRIC ANALGESIA AND ANESTHESIA, AND RESUSCITATION OF THE NEWBORN
 Anatomic Characteristics of the Fetal Head and Maternal Pelvis
Anatomic Characteristics of the Fetal Head and Maternal Pelvis
Vaginal delivery necessitates the accommodation of the fetal head to the bony pelvis.
FETAL HEAD
Sutures
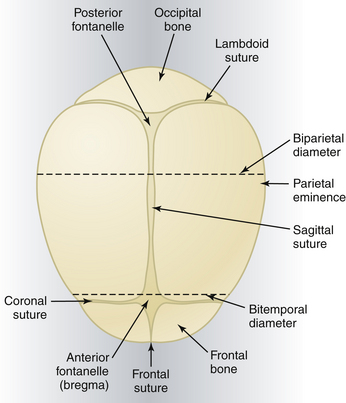
The membrane-occupied spaces between the cranial bones are known as sutures. The sagittal suture lies between the parietal bones and extends in an anteroposterior direction between the fontanelles, dividing the head into right and left sides (Figure 8-1). The lambdoid suture extends from the posterior fontanelle laterally and serves to separate the occipital from the parietal bones. The coronal suture extends from the anterior fontanelle laterally and serves to separate the parietal and frontal bones. The frontal suture lies between the frontal bones and extends from the anterior fontanelle to the glabella (the prominence between the eyebrows).
Landmarks
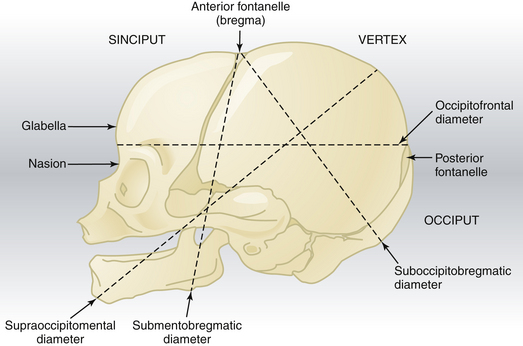
The fetal skull is characterized by a number of landmarks. Moving from front to back, they include the following (Figure 8-2):
Diameters
Several diameters of the fetal skull are important (see Figures 8-1 and 8-2). The anteroposterior diameter presenting to the maternal pelvis depends on the degree of flexion or extension of the head and is important because the various diameters differ in length. The following measurements are considered average for a term fetus:
The transverse diameters of the fetal skull are as follows:
The average circumference of the term fetal head, measured in the occipitofrontal plane, is 34.5 cm.
PELVIC ANATOMY
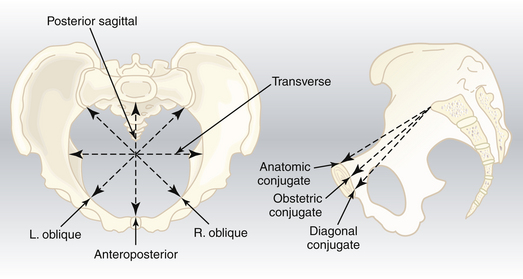
Pelvic Diameters
The average lengths of the diameters of each pelvic plane are listed in Table 8-1.
TABLE 8-1 AVERAGE LENGTH OF PELVIC PLANE DIAMETERS
| Pelvic Plane | Diameter | Average Length (cm) |
|---|---|---|
| Inlet | True (anatomic) conjugate | 11.5 |
| Obstetric conjugate | 11 | |
| Transverse | 13.5 | |
| Oblique | 12.5 | |
| Posterior sagittal | 4.5 | |
| Greatest diameter | Diagonal conjugate | 12.75 |
| Transverse | 12.5 | |
| Midplane | Anteroposterior | 12 |
| Bispinous | 10.5 | |
| Posterior sagittal | 4.5-5 | |
| Outlet | Anatomic anteroposterior | 9.5 |
| Obstetric anteroposterior | 11.5 | |
| Bituberous | 11 | |
| Posterior sagittal | 7.5 |
Pelvic Inlet
The pelvic inlet has five important diameters (Figure 8-3). The anteroposterior diameter is described by one of two measurements. The true conjugate (anatomic conjugate) is the anatomic diameter and extends from the middle of the sacral promontory to the superior surface of the pubic symphysis. The obstetric conjugate represents the actual space available to the fetus and extends from the middle of the sacral promontory to the closest point on the convex posterior surface of the symphysis pubis.
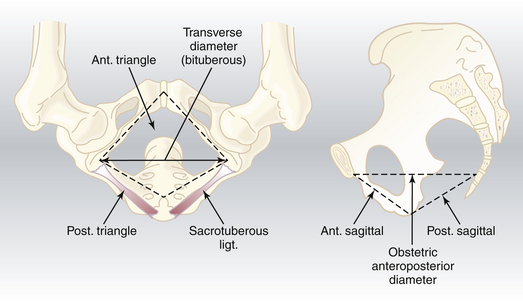
Pelvic Outlet
The pelvic outlet has four important diameters (Figure 8-4). The anatomic anteroposterior diameter extends from the inferior margin of the pubis to the tip of the coccyx, whereas the obstetric anteroposterior diameter extends from the inferior margin of the pubis to the sacrococcygeal joint. The transverse (bituberous) diameter extends between the inner surfaces of the ischial tuberosities, and the posterior sagittal diameter extends from the middle of the transverse diameter to the sacrococcygeal joint.
PELVIC SHAPES
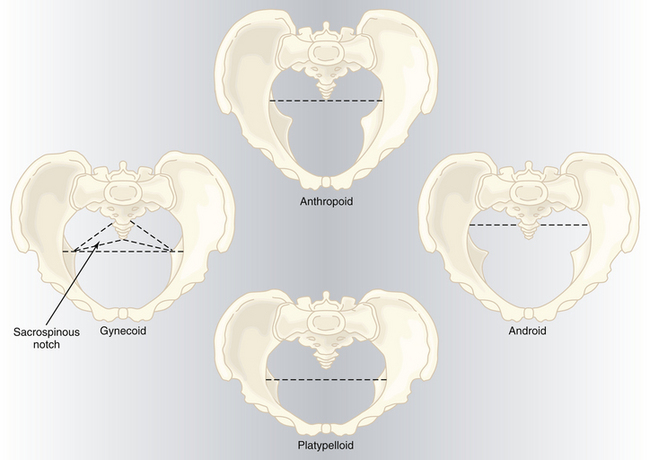
Based on the general bony architecture, the pelvis may be classified into four basic types (Figure 8-5).
Gynecoid
Android
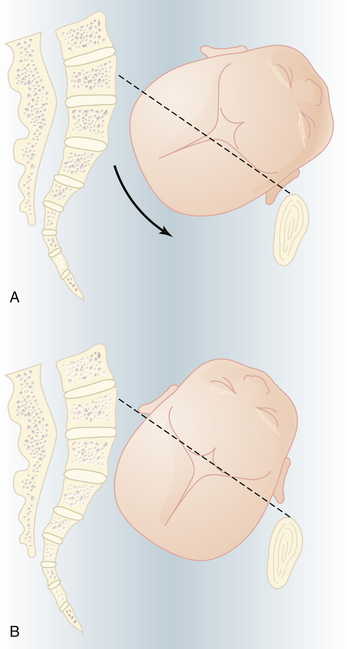
ENGAGEMENT
In most women, the bony presenting part is at the level of the ischial spines when the head has become engaged. The fetal head usually engages with its sagittal suture in the transverse diameter of the pelvis. The head position is considered to be synclitic when the biparietal diameter is parallel to the pelvic plane and the sagittal suture is midway between the anterior and posterior planes of the pelvis. When this relationship is not present, the head is considered to be asynclitic (Figure 8-6).
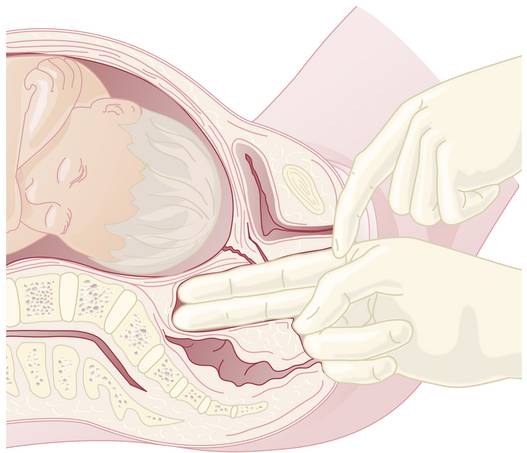
CLINICAL PELVIMETRY
The clinical evaluation is started by assessing the pelvic inlet. The pelvic inlet can be evaluated clinically for its anteroposterior diameter. The obstetric conjugate can be estimated from the diagonal conjugate, which is obtained on clinical examination (see Figure 8-3).
The diagonal conjugate is approximated by measuring from the lower border of the pubis to the sacral promontory using the tip of the second finger and the point where the base of the index finger meets the pubis (Figure 8-7). The obstetric conjugate is then estimated by subtracting 1.5 to 2 cm, depending on the height and inclination of the pubis. Often the middle finger of the examining hand cannot reach the sacral promontory; thus, the obstetric conjugate is considered adequate. If the diagonal conjugate is greater than or equal to 11.5 cm, the anteroposterior diameter of the inlet is considered to be adequate.
PREPARATION FOR LABOR
Before actual labor begins, a number of physiologic preparatory events usually occur.
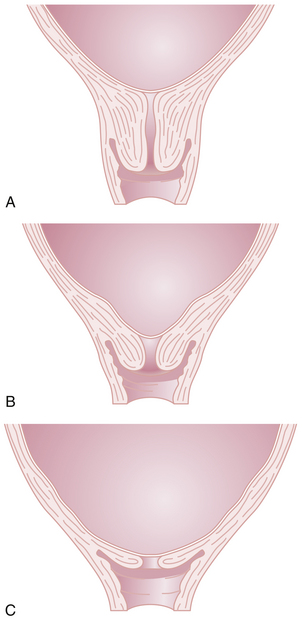
Cervical Effacement
Before the onset of parturition, the cervix is frequently noted to soften as a result of increased water content and collagen lysis. Simultaneous effacement, or thinning of the cervix, occurs as it is taken up into the lower uterine segment (Figure 8-8B). Consequently, patients often present in early labor with a cervix that is already partially effaced. As a result of cervical effacement, the mucous plug within the cervical canal may be released. The onset of labor may thus be heralded by the passage of a small amount of blood-tinged mucus from the vagina (“bloody show”).
STAGES OF LABOR
First Stage of Labor
PHASES
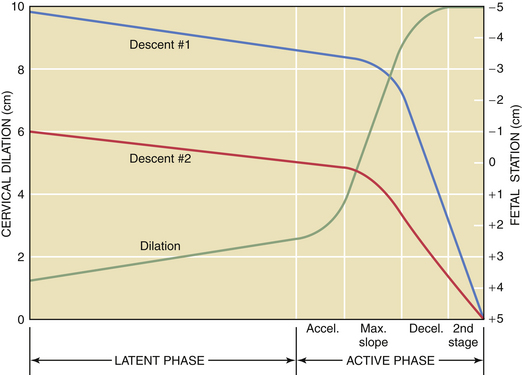
The first stage of labor consists of two phases: a latent phase, during which cervical effacement and early dilation occur, and an active phase, during which more rapid cervical dilation occurs (Figure 8-9). Although cervical softening and early effacement may occur before labor, during the first stage of labor, the entire cervical length is retracted into the lower uterine segment.
LENGTH
The length of the first stage may vary in relation to parity; primiparous patients generally experience a longer first stage than do multiparous patients (Table 8-2). Because the latent phase may overlap considerably with the preparatory phase of labor, its duration is highly variable. It may also be influenced by other factors, such as sedation and stress. The active phase begins when the cervix is 3 to 4 cm dilated in the presence of regularly occurring uterine contractions. The minimal dilation during the active phase of the first stage is nearly the same for primiparous and multiparous women: 1 and 1.2 cm/hour, respectively. If progress is slower than this, evaluation for uterine dysfunction, fetal malposition, or cephalopelvic disproportion should be undertaken.
TABLE 8-2 CHARACTERISTICS OF NORMAL LABOR
| Characteristic | Primipara | Multipara |
|---|---|---|
| Duration of first stage | 6-18 hr | 2-10 hr |
| Rate of cervical dilation during active phase | 1 cm/hr | 1.2 cm/hr |
| Duration of second stage | 30 min to 3 hr | 5-30 min |
| Duration of third stage | 0-30 min | 0-30 min |
CLINICAL MANAGEMENT OF THE FIRST STAGE
ANALGESIA
Adequate analgesia is important during the first stage of labor (see later in this chapter).