Fig. 21.1
Neuropelveologic assessment of dermatomes and trigger points of the pelvic nerves. L5 fifth lumbar root, S sacral nerve root, PN pudendal nerve, SN sacral nerve roots, GFN genitofemoral nerve
21.3 The Laparoscopy: The Tool of Choice in Neuropelveology
Because of the anatomical location of the nerves within the pelvis (near major pelvic blood vessels), classical pelvic nerve surgery is very invasive and risky, especially for massive blood loss and nerves damages. Open pelvic surgery is laborious and cumbersome. Laparoscopy overcomes all of the limitations. High-resolution video cameras provide necessary magnification and microneurofunctional procedures. Thanks to these developments, all pelvic nerves and plexuses are now easily accessible for morphologic (Possover 2004a; Possover et al. 2007a) and functional (Possover et al. 2004) exploration by laparoscopy (Fig. 21.2). In addition to evaluating the disease status and making functional assessments, laparoscopic examination of the pelvic nerves also makes it possible to identify and to treat potential causes of functional disorders and neuropathic pain (Possover 2010b): neurofunctional procedures, such as nerve decompression (relief of pressure), neurolysis (release of a nerve sheath), nerve reconstruction, or implantation of stimulation electrodes in direct contact to nerves for postoperative neuromodulation (Possover et al. 2007b, c), can be done in optimal conditions by laparoscopy.
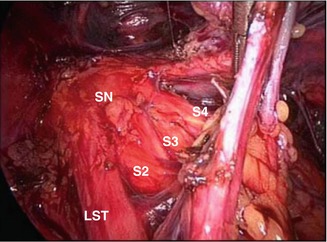
Fig. 21.2
Laparoscopic dissection of the left sacral plexus (supracardinal portion). SN sciatic nerve, LST lumbo-sacral trunk, S sacral nerve root
21.4 Control to Sensoric Functions of the Pelvic Nerves and Plexuses: New Therapeutic Options for Urge Amount of Patients
Pudendal pain, proctalgia, coccygodynia, vulvodynia, and pudendal neuralgia are all pain situations reported as “chronic pelvic pain”. All these pain situations occur in 7–24 % of the population and are associated with impaired quality of life and high healthcare costs. Anoperineogenital pain are frequent complaint usually not only as a result of common and easily recognizable organic disorders such as anal fistula, thrombosed hemorrhoids, genitoanal cancer, or other dermatologic pathologies but can also occur under circumstances in which no organic cause can be found. Such pain syndromes are then poorly understood, with little research evidence available to guide their diagnosis and treatment. Also, lumbar pain with irradiations in the legs without any real spinal etiology is frequently treated by medical treatments on long-term or unnecessary surgeries; pelvic origins of such pain are very rarely evocated. Endopelvic lesions are less well known and because their diagnosis is difficult and surgical approach remained difficult and invasive, these etiologies are mostly managed by symptomatic treatments. In general, the number of patients suffering from pelvic nerve disorders is grossly underestimated. In the international literature, also the prevalence of pelvic nerve damage is estimated to be low. This is in stark contrast to clinical reality: both bladder and bowel dysfunctions and neurogenic pain after pelvic surgeries are seen every day in many doctors’ offices around the world. This may be due to a lack of awareness of the existence of such diseases and to the complexity of the pelvic nerve anatomy. In our experience, the most frequent etiologies for pelvic nerve irritation or even damages are:
Deeply infiltrative sciatic nerve (plexus sacralis endometriosis as part of a parametric endometriosis or as an isolated condition) (Possover et al. 2011)
Surgical nerves damages, especially surgeries with mesh implantation (Possover 2009; Possover and Lemos 2011)
Vascular compression syndrome of the pelvic nerves
More seldom, pelvic nerve conditions such as schwannomas (Possover 2013a) and pathologies of the sacral bone
Procedures of laparoscopic nerve decompression have proven safe and effective. They are reported to achieve remarkable pain relief in 62 % of patients with postoperative nerve damage, in 78 % of patients with endometriosis involving the pelvic nerves, and in more than 80 % of patients with pelvic nerve compression by varicose veins in the pelvic area.
In axonal nerve pathologies, or in event of failure of the classical peripheral nerve surgical techniques, the neuromodulation is a well-known option to control both neural pain and dysfunctions of the lower intestinal and urinary tract. The surgical procedure is designed to implant an electrode in contact to the injured nerve proximal to the lesion, which is connected to a pacemaker that produces continuous low-level electrical current. The LION procedure to pelvic nerves in pain situation is only indicated in neurogenic nerves damages (axonal lesion) that represent only a small percent of indications.
21.5 The LION Procedure to the Pudendal Nerve to Treat Motor Pelvic Dysfunctions
Urinary and fecal dysfunctions affects millions of women and men all over the world and this condition encompasses overactive bladder, urinary/fecal incontinence, chronic constipation, and urination difficulties due to obstructions of the urinary tract or due to neurological central or peripheral nerve diseases. Continence and micturition/defecation involve a balance between urethral/anal closure and detrusor/rectal muscle activity. Disorders or troubles of coordination of both functions are responsible for bladder and intestinal dysfunctions.
The most common types of urinary disorders especially in women is stress urinary incontinence that is caused by loss of support of the urethra, which is usually a consequence of damage to pelvic support structures as a result of childbirth. Behind behavior changes and pelvic floor training, treatment focuses on the surgical reconstruction of the normal pelvic anatomy using techniques of vaginal repair or sling procedures. In all other conditions, treatments target on efferent effects by using neuroregulator pharmacotherapies with two aims: the first to reduce high vesical pressures (to avoid retrograde reflux) and the second to restore normal micturition. So alpha blockers target on reduction urethral pressure, whereas antimuscarinics and parasympathomimetic drug respectively reduce or active detrusor contractility. Despite the fact that pharmacological treatments are currently first therapeutic options, adherence on long term is low because of side effects and patient tolerability often challenging (Abrams et al. 2000). Also, intradetrusor injections of botulinum toxin A constitute a powerful treatment of overactive bladder in patients being able and willing to return for frequent postvoid residual evaluation (risk for infections) and to perform self-catheterization if necessary (elevated postvoid residuals). Elevated postvoid residuals responsible for urinary tract infections and repetition of injections for life lead to discontinuation of treatment (Kantartzis and Shepherd 2012). Electrical stimulation of the pelvic nerves has emerged as an alternative and attractive treatment for refractory cases of urinary disorders, as well those due to a hypo- or a hypercontractility of the detrusor and/or of the sphincter, as those due to trouble of urethra-vesical coordination (Tanagho and Schmidt 1988; van Kerrebroeck 1998). Pelvic nerve neuromodulation has been proven effective and is today an established treatment option for patients refractory to or intolerant of conservative treatments for urinary disorders. The method, known as the LION procedure (Laparoscopic Implantation Of Neuroprothesis), allows the surgeon to place an electrode directly on the pelvic nerves of interest. Neuromodulation is absolutely minimal invasive and preserves the anatomical integrity of the pelvic nerves, the lower urinary, and intestinal tracts and can be readily reversed. In the technique of Sacral Nerve Neuromodulation, implantation of the stimulation’s electrode can be obtained by percutaneous puncture technique. However, behind the fact that most gynecologists are not familiar with such techniques, SNM present several important inconvenience and disadvantages (Possover 2014a). Behind technical aspects, SNM present two major problems:
Not all pelvic nerves and plexuses are suitable for puncture techniques, only the superficial nerves outside the pelvis or below the pelvic floor.
SNM do not offer etiologic treatment; once neuromodulation is indicated, possible etiologies are omitted. Conservative treatment options and SNM should be classically considered before surgical options are considered. However, when any etiological treatment may exist, even a surgical one, medical and neuromodulative treatment options should be only considered after such an etiologic treatment option has failed. When no etiology can be found, patient’s disorders are classified as “idiopathic” or “nonneurogenic.” However, some etiologies can only be diagnosed by laparoscopy: so deeply infiltrating endometriosis of the bladder, vesicointestinal adhesions, endometriosis/fibrosis/vascular entrapment of the sacral nerve roots or of the pudendal nerve are all conditions that can induce such urinary disorders, but can only be diagnosed and treated by laparoscopy (Possover and Forman 2012). Etiologic treatment is then not only the treatment of choice but also avoids unnecessary costs for symptomatic treatment options on long term. When by laparoscopy no any etiology can be found, the procedure can be directly used for placement of an electrode to the nerve(s) of interest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


