CHAPTER 16 NEUROPATHOLOGY
INTRACRANIAL AND SPINAL TUMORS
Overview
• Typing and grading of brain tumors is prescribed by the WHO classification of Tumors of the Central Nervous System
• The tumor location can also restrict the diagnostic possibilities, the following are the more common diagnosis by site in children
Specimen handling
• Best practice for specimen sampling is as described for pediatric soft tissue tumors (see Chapter 6)
• The completeness of resection is an important prognostic factor in many pediatric brain tumors but is usually assessed by postoperative radiology
Role of intraoperative diagnosis
• Overall accuracy of intraoperative diagnosis in predicting the final diagnosis is in the range of 85–95%
GLIOMAS
PILOCYTIC ASTROCYTOMA
Histopathological features
Diagnostically useful features
Morphological variations
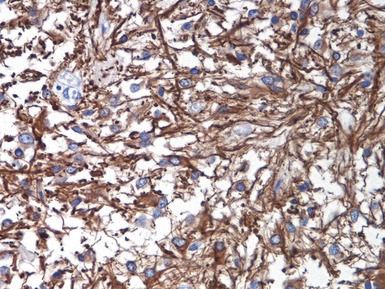
Immunohistochemical staining
• There is some evidence that WT-1 staining may help to distinguish neoplastic astrocytes from reactive astrocytes (Schittenhelm et al 2008, 2009)
Differential diagnoses and pitfalls
• In small biopsies, differential diagnosis from a low-grade diffuse astrocytoma (grade II) may be difficult
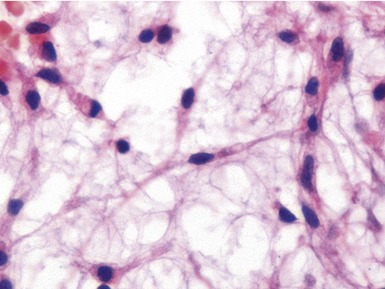
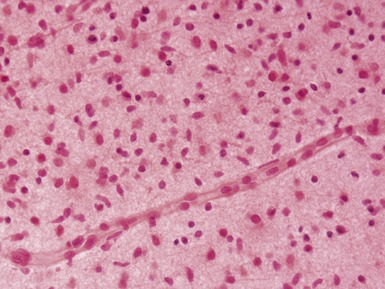
DIFFUSE ASTROCYTOMA (Fig 16.14)
Morphological types
Immunohistochemical staining
• There is some evidence that WT-1 staining may help to distinguish neoplastic astrocytes from reactive astrocytes (Schittenhelm et al 2008, 2009)
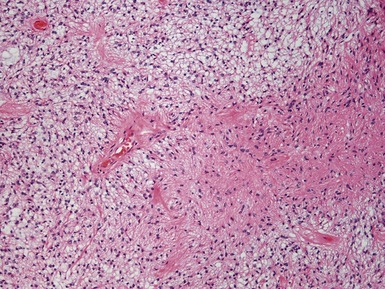
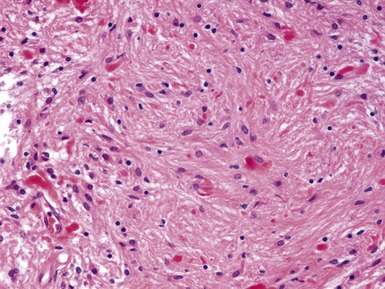
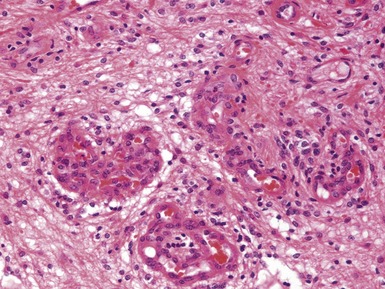
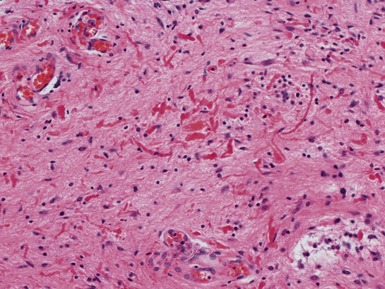
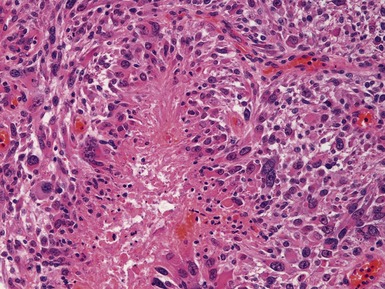
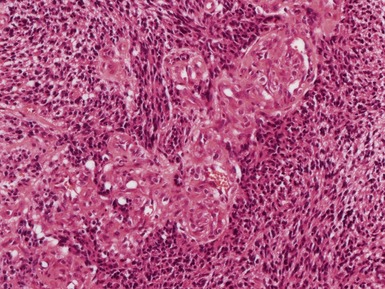
ANAPLASTIC ASTROCYTOMA (Figs 16.15, 16.16)
• Diffuse astrocytoma showing more cellularity and pleomorphism than a grade II diffuse astrocytoma with clear mitotic activity
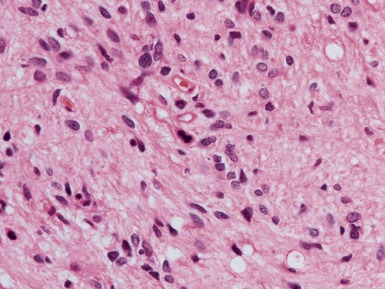
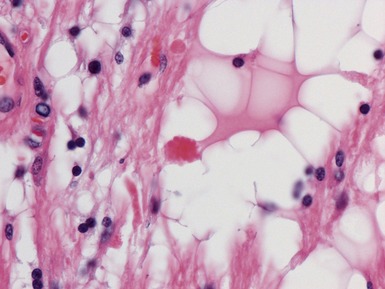
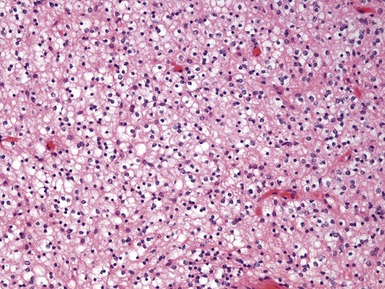
Fig 16.15 Photomicrograph of an anaplastic astrocytoma demonstrating increased cellularity and pleomorphism compared with a grade II tumor. (see Fig 16.14)
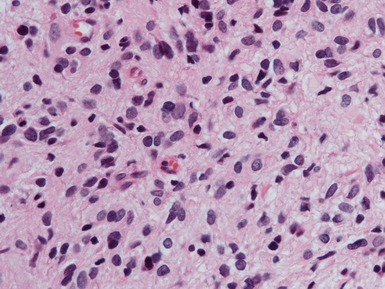
Fig 16.16 Photomicrograph of an anaplastic astrocytoma demonstrating increased cellularity, pleomorphism and mitotic activity compared with a grade II tumor. (see Fig 16.14)
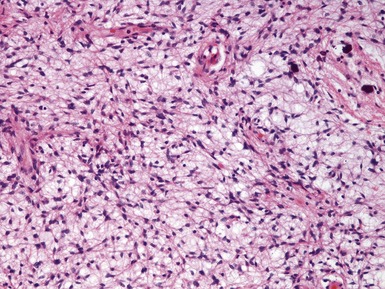
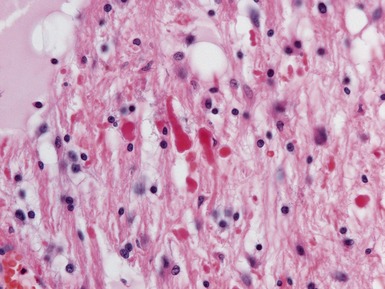
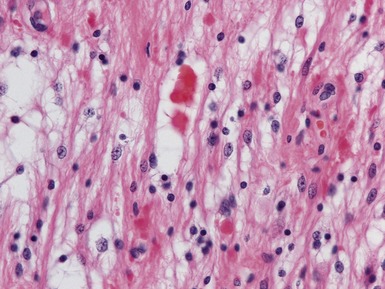
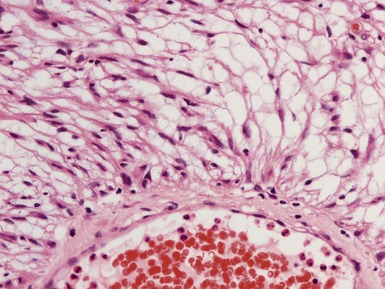
GLIOBLASTOMA (Figs 16.17–16.19)
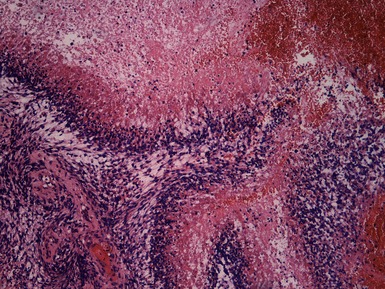
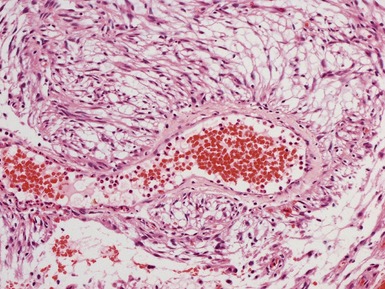
Fig 16.18 Photomicrograph demonstrating a glioblastoma with extensive tracks of pseudo-palisading necrosis.