>  , slightly. Decreases w/ age.
, slightly. Decreases w/ age.
• 75% of primary HA will ↓ in Preg. ∼40% PP → HA, esp 1st w.
Pathogenesis
• 90% are tension-type, migraine, or cluster HA. In  , 70% are a/w menses, but <20% are pure menstrual migraine.
, 70% are a/w menses, but <20% are pure menstrual migraine.
• Multifactorial initiation. Nociceptor activation/sensitization can → central sensitization, ↑ pain transmission, ↓ pain threshold. Minor role for genetics.
Differential Diagnosis
• Primary (most common): Migraine, tension-type HA, cluster, orgasmic HA (elevated estrogen, prolactin, oxytocin)
• Secondary: Ischemic stroke, hemorrhagic stroke (SAH, AVM, HTN), venous sinus thrombosis, carotid or vertebral artery dissection, vasculitides, reversible cerebral vasoconstriction syndromes (Call-Fleming syn [reversible cerebral vasoconstriction], PRES)
• Other: Preeclampsia/eclampsia, benign intracranial HTN, sinusitis, overmedication, PDPH, tumor, estrogen withdrawal, brain tumor
• Primary care: Meningitis, pseudotumor cerebri, trigeminal neuralgia, TMJ syn, temporal arteritis
Diagnostic Workup
• Hx: Age, aura, prodrome, frequency, intensity, duration, timing, quality, radiation, assoc sx, FHx, precipitating/relieving factors, changes w/ activity/food/EtOH, resp to rx, visual changes, h/o trauma, change in sleep pattern/exercise/weight/diet/contraceptives, environmental toxins/exposures, menstrual Hx
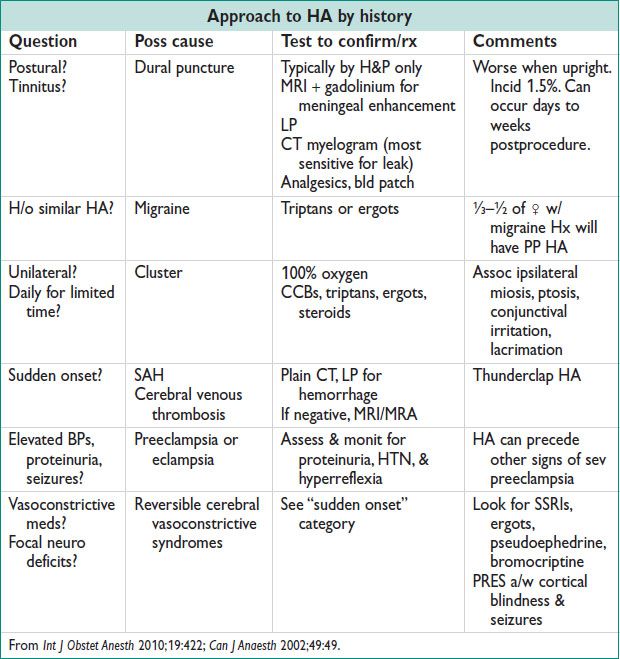
• Warning signs: Thunderclap HA, autonomic sx, 1st/worst HA of life, worsening, fever, change in mental status/personality, exercise assoc, very young or old age, h/o cancer/Lyme dz/HIV/Preg/PP, *focal neuro findings, *meningismus, *papilledema (* = imaging)
• Physical exam: BP, pulse, auscultation for bruits (neck, temporal), palpation (head, neck, spine), neuro exam w/ fundoscopy
• Labs: Usually not needed; TSH, ESR, CRP, toxicology screen, Lyme Ab, LP (if suspect SAH or infxn)
• Imaging: See warning signs. CT head/c-spine or MR ok. MRI/MRA head/neck if post fossa or vascular suspected.
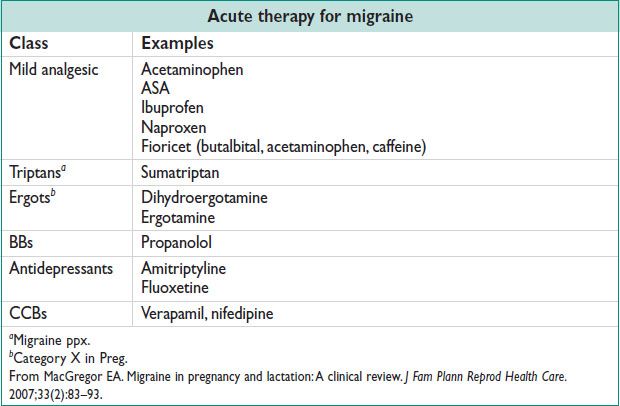
Treatment and Medications
• 1st line: Relaxation, ice packs, reassurance, acetaminophen, ibuprofen (not Preg). 2nd line: Add narcotics sparingly. 3rd line: Antiemetics (eg, chlorpromazine), IV magnesium. Avoid NSAIDs in 3rd trimester Preg (→ ductus arteriosus closure & oligohydramnios). Other treatments, see below.
• Tension-type HAs: Stress reduction, warm showers, massage, ice/heat packs, posture correction, physical therapy, prescription eyeglasses. NSAIDs, ASA, Tylenol, caffeine, muscle relaxants. Tricyclics for prevention.
MIGRAINE
Definition & Epidemiology
• Recurring syn of HA, nausea, vomiting, &/or other sx of neurologic dysfxn. Migraine w/ aura = visual sx occur/resolve w/ HA, risk factor for ischemic stroke.
• Increases w/ age in  : 22% at 20–24 yo; 28% at 25–29 yo; 33% at 30–34 yo; ∼37% for 35–39 yo. Overall ↓ in Preg, but 8% of pregnant women (esp w/ h/o aura) have increased attack frequency.
: 22% at 20–24 yo; 28% at 25–29 yo; 33% at 30–34 yo; ∼37% for 35–39 yo. Overall ↓ in Preg, but 8% of pregnant women (esp w/ h/o aura) have increased attack frequency.
• Risk for preeclampsia increased w/ HA (Am J Hypertension 2008;21(3):360). 2.4-fold ↑ w/ any HA Hx; 3.5-fold ↑ w/ migraine; 4-fold ↑ w/ migraines during Preg.
• Status migrainosus: >72 h → evaluate for secondary causes
Pathophysiology (Headache 2006;46:S49)
• Brain itself lacks pain receptors, but surrounding meningeal, muscle, skin, vessel, subcutaneous tissue, or mucous membrane inflammation/injury → HA pain
• Hormonal fluctuations in estrogen → menstrual migraine or PP migraine (withdrawal); ↓estrogen → increased in serotonergic tone
• Migraine phases: Prodrome → ± aura → main migraine pain → resolution
Treatment
• See conservative measures above. Narcotics not 1st line; abortive therapy needed early. Acute therapies used more than 2 d weekly can lead to rebound HA.
• Avoid combined OCPs if h/o migraine w/ aura or age >35 yo & no aura. D/c combination hormonal contraception if severity/frequency of HA increases or in setting of new onset migraine w/ aura.
SEIZURE DISORDERS
Definition/Epidemiology
• Abn discharge of neurons in the CNS; 5–10% of pop affected
• Epilepsy – recurrent seizures, 0.5–1% of pop; 41 cases per 100000 women
• Generalized seizures: Start in both cerebral hemispheres at onset
• Tonic–clonic: 10–20-s tonic phase (constant muscle contraction) followed by 30-s clonic phase (intermittent muscle contraction)
• Absence: Transient lapse of consciousness – no loss of posture, muscle tone
• Myoclonic: Brief contraction, sudden onset
• Atonic: Brief loss of complete muscle tone (also called “drop attacks”)
• Partial/focal seizures: Limited to 1 area of 1 cerebral hemisphere at onset
• Simple: Motor, sensory, or autonomic; no impairment of consciousness
• Complex: Impairment of consciousness + automatisms
Differential Diagnosis
• Syncope – no aura; motor manifestations <30 s; no postictal confusion; pt may have pallor & clamminess
• Psychogenic sz – asym limb movements, pelvic thrusting
• Other – metabolic (EtOH, hypoglycemia); migraine, TIA
• Eclampsia – generalized convulsions &/or coma in the setting of preeclampsia & w/o evid of other neurologic conditions. Preg assoc; pt often has elevated BPs, blurry vision, proteinuria, RUQ pain.
Pathophysiology/Etiology
• Alcohol withdrawal, ilicit drugs, meds (β-lactams, antidepressants, clozipine)
• Brain tumor; BP (a/w preeclampsia/eclampsia)
• Cerebrovascular dz (subdural hematoma, hypertensive encephalopathy)
• Degen disorders (Alzheimer’s)
• Electrolyte imbalance (HoNa, hypoglycemia)

Clinical Manifestations
• Aura – premonition, abn smells, tastes, oral automatism
• Postictal period – can last minutes to hours; slowly resolving period post sz. Pt may be confused, disoriented, lethargic.
• Status epilepticus – state of continuous seizures >30 min or repeated seizures w/o resolution of postictal periods. Assoc complications: Rhabdomyolosis, lactic acidosis, neuronal death.
Workup and Studies
• Obtain collateral Hx from witnesses as pt will often have amnesia of event
• Ask about loss of responsiveness, aura, unusual behavior, loss of autonomic control (urinary or fecal incontinence)
• Evaluate for etiology w/ h/o fever, illness, prev sz; in Preg, elevated BPs, prot in the urine, ext & facial swelling
• Exam to look for focal neurologic abnormalities or evid of injury from sz activity (oropharyngeal or musculoskeletal or secondary head injury & ecchymoses)
• Labs: CBC, CMP, LFTs, toxicology screen, medication levels
• Preg: Preeclampsia labs (CBC, LFTs, BUN/Cr, uric acid, LDH, proteinuria)
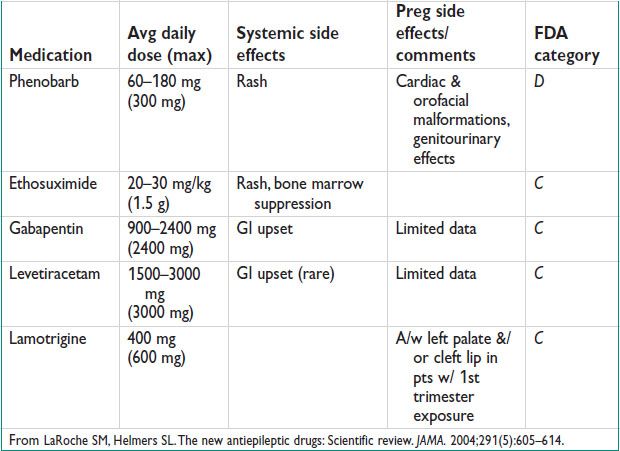
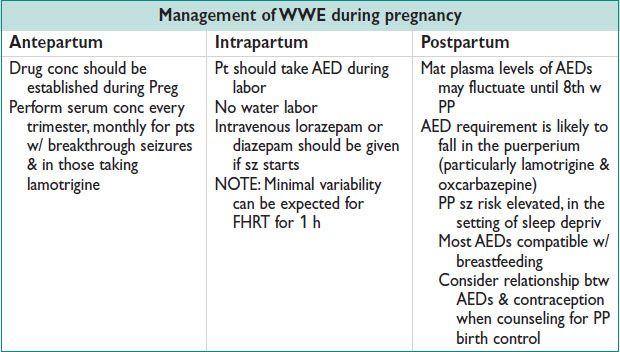
Pregnancy Care (Neurol 2006;66:354)
• 500000 WWE are of childbearing age; 3–5 births per 1000 will be to WWE (Neurol 2000;55:S21). Preg w/ AEDs → ↑ IUGR & hypertensive disorders, ↑ CS (Acta Obstet Gynecol Scan 2006;85:643). If sz free for 2 y, consider withdrawal of AEDs at least 6 mo prior to conception.
Contraception
• Anticonvulsants that Ø steroid levels: Phenobarbitol, primidone, phenytoin, carbamezapine (to lesser extent w/ oxcarbazepine, felbamate, topiramate)
• If OCPs are deemed necessary, use 50 mcg of estrogen component or extended cycle treatments (3 cycles followed by 4-d break)
• Emergency Contraception: Levonorgestrel 1.5 mg separated by 12 h (doubled dose).
• WHO recommends alternative form of contraception: Levonorgestrel IUD, copper IUD, Depo-Provera (a/w decreased sz frequency)
ECLAMPSIA
Definition
• New onset seizures in a woman w/ preeclampsia, not attributable to other causes
Epidemiology
• Accounts for 12% of mat deaths, worldwide (developing countries > developed countries) (Semin Perinatol 2009;33:130). ∼38% occur w/o preceding sx.
• 2% mortality; 23% will require ventilation; 35% have 1 major complication (pulm edema, renal failure, respiratory distress syn, dissem intravascular coagulation, stroke, cardiac arrest, acute respiratory distress syn)
• Seizures occur in 2–3% of pts w/ sev preeclampsia not receiving magnesium ppx; incid 1.6–10 cases per 10000 deliveries
• Distribution by GA:
<20 w GA: Consider molar Preg or antiphospholipid Ab syn
Antepartum: 38–55%
Intrapartum: 13–16%
Up to 48-h PP: 5–39%
>48 h PP: 5–17%, think AVM, ruptured aneurysm, carotid artery dissection, or idiopathic sz d/o
Pathophysiology (Am J Obstet Gynecol 2004;190:714)
• Cerebral autoregulation in resp to high systemic BP → vasospasm of cerebral arteries, intracellular edema
• Loss of autoregulation of cerebral bld flow in resp to high systemic BP → hyperperfusion, endothelial damage, extracellular edema
Clinical Manifestations (Obstet Gynecol 2011;118:995)
• HA – cerebral edema (sens to predict eclampsia 0.98 [95% CI 0.87–1]) (Acta Obstet Gynecol Scand 2011;90:564)
• Vision changes – vasospasm of cerebral & retinal vessels
• Neurologic sx – most common premonitory sx (rates vary from 50–90%)
• Full PIERS model – odds ratio of 2.92 for predicting adverse outcomes in preeclampsia; calculator at: piers.cfri.ca/PIERSCalculatorH.aspx (Lancet 2011;377:219)
• Note: Presence of HTN & proteinuria are poor predictors of eclampsia, rare event. See also chaps. 11 and 12 for preeclampsia.
Treatment and Medication
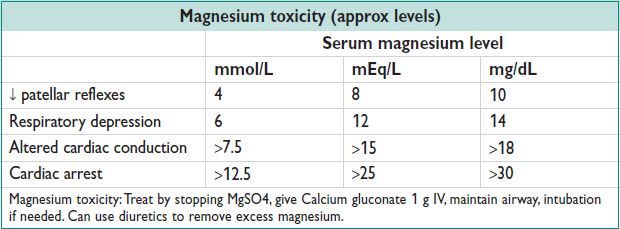
• Drug of choice = magnesium sulfate (calcium channel antagonism) 4–6 g IV bolus then 1–2 g/h. If no IV → 5 g IM in each buttock (10 g total; rpt 3 g alternating buttock q4h). If seizing on magnesium, rebolus 2 g IV. Therapeutic level 4–6 mEq/L.
• 2nd line: Phenytoin: Loading dose by weight (<50 kg = 1000 mg; 50–70 kg = 1250 mg; >70 kg = 1500 mg). Therapeutic level 12–20 mcg/mL. Check 2 h after loading → subseq dose; if <10 mcg/mL → 500 mg IV, if 10–12 mcg/mL → 250 mg. check level q12h.
• 3rd line: Diazepam 5–10 mg IV bolus, rpt q10–15min prn, max 30 mg in 8 h
• Diazepam, phenytoin were a/w increased recurrence of seizures compared w/ magnesium sulfate (Br J Obstet Gynaecol 1998;105:300; N Engl J Med 1995;333)
• Fetal brady occurs during eclamptic sz. Recover mom; no need for urgent CS
• MagPIE trial: International RCT, >10000  w/ at least mild preeclampsia randomized to magnesium sulfate or placebo. Magnesium sulfate decreases relative risk of eclampsia by 58% (95% CI 40–71). No documented adverse effects on mom or baby in short-term or long-term period (Lancet 2002;359:1877; British J Obstet Gynecol 2006;114:300)
w/ at least mild preeclampsia randomized to magnesium sulfate or placebo. Magnesium sulfate decreases relative risk of eclampsia by 58% (95% CI 40–71). No documented adverse effects on mom or baby in short-term or long-term period (Lancet 2002;359:1877; British J Obstet Gynecol 2006;114:300)
STROKE IN PREGNANCY
Epidemiology and Pathophysiology
• Stroke in Preg = 4–26/100000 (3–10/100000, nonpregnant women)
• Most common in 3rd trimester or puerperium, but also ↑ in PP (8.7× for ischemic stroke; 24× for hemorrhagic stroke). ∼10% of all mat deaths.
• Most common cause of stroke in Preg is preeclampsia/eclampsia
• ↑ due to hypercoagulable state of Preg; cerebral endothelial dysfxn
Diagnosis (Obstet Med 2011;4:2)
• Acute: Hx, PE (listen for murmurs, carotid & subclav bruits, & look for signs of periph emboli). Urgent CT, noncontrast, to rule out hemorrhage, followed by CT angio. MRI/MRA w/ gadolinium. Doppler scan of the LE → if negative, then MRV.
• Risk factors: Hypercoagulable state: Lupus anticoagulant, anticardiolipin antibodies, anti-β2 glycoprotein, Factor V Leiden, prothrombin, prot C & S, antithrombin III. Peripartum cardiomyopathy.
Post Reversible Encephalopathy Syn (Mayo Clin Proc 2010;85:427)
• Related to cerebral autoregulation & endothelial dysfxn. Seen in preeclampsia.
• Features: HA, altered consciousness, visual disturbances (hemianopia, visual hallucinations), seizures (often presenting manifestation)
• Radiology: Symmetrical white matter edema in the post cerebral hemispheres, rarely seen on CT, but better depicted on MRI
• Rx: Lower BP, fully reversible w/i days to weeks
Postpartum Cerebral Angiopathy (Am J Obstet Gynecol 2004;191:375)
• Reversible cerebral vasoconstriction syndromes
• Timeline: Few days post deliv. Features: Thunderclap HA, vomiting, seizures.
• Radiology: Multifocal segmental narrowing of cerebral arteries, resolution in 4–6 w
• CSF nml
Cerebral Aneurysm Rupture and SAH (N Engl J Med 1996;335:768)
• Relative risk of intracerebral hemorrhage during Preg & up to 6 w PP is 5.6 times that of the nonpregnant pt
• Surgical rx after SAH during Preg improves mat & fetal outcomes
• Favor vaginal deliv unless aneurysm is diagnosed at term or there has been neurosurgical intervention w/i the week before deliv
CEREBRAL VENOUS THROMBOSIS
Definition and Epidemiology (Stroke 2011;42:1158)
• Thrombosis of the venous sinuses, cerebral veins, or jugular veins
• Represents 2% of all Preg-related strokes; 12/100000 deliveries (Stroke 2011;42:1158). Risk is highest during 3rd trimester & PP.
Etiology/Pathophysiology
• Dehyd, puerpurial & PP infxn, thrombophilia inherent to Preg
• Risk increased w/ use of OCPs (22.1-fold increased odds [95% CI 5.9–84.2%]); increased odds for pts w/ thrombophilia (eg, prothrombin gene mut)
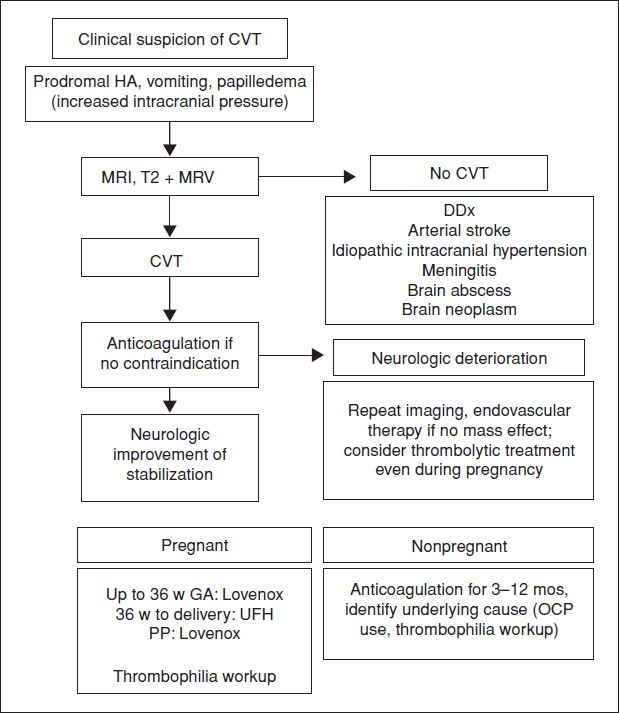
Diagnostic WorkUp
• Acute: Brain CT &/or MRI, bubble study & vascular US of the venous sinuses, cerebral veins, or jugular veins–Best is MRI T2 + MRV – better visualization, good detection of brain parenchyma, no radiation. Can evaluate for both thrombosis & stroke (Stroke 2011;42:1158).
• A nml D-dimer, high negative predictive value, low probability of CVT
• Empty delta sign on contrast-enhanced CT (hyperdensity of cortical vein or dural sinus, filling defect) seen in 25–50% of cases
• Venous infarction is flame-shaped
Figure 18.1 Management of cerebral venous thrombosis