Chapter 65 Nephrology
ACUTE RENAL FAILURE
ETIOLOGY
What Is Acute Renal Failure?
 Prerenal conditions impair renal perfusion.
Prerenal conditions impair renal perfusion.
 Intrinsic renal diseases affect glomeruli, tubulointerstitium, or microvasculature.
Intrinsic renal diseases affect glomeruli, tubulointerstitium, or microvasculature.
 Postrenal states cause obstruction beyond the renal parenchyma.
Postrenal states cause obstruction beyond the renal parenchyma.
Table 65-1 has examples of oliguric ARF in each category. Remember that not all ARF is associated with oliguria.
Table 65-1 Causes of Acute Renal Failure
| Prerenal | Intrinsic Renal (Most Common Category in Children) | Postrenal |
|---|---|---|
| TBW depletion Gastroenteritis IV volume depletion Septic shock Nephrotic syndrome Mechanical failure of renal perfusion Congestive heart failure Cardiac tamponade Critical coarctation of the aorta Renal artery thrombosis | Glomerulonephritis Tubulointerstitial diseaseAcute tubular necrosis Toxic (e.g., aminoglycosides)Ischemic (prolongedprerenal state) Tubulointerstitial nephritisDrug-induced (e.g., NSAIDs) Infectious (e.g., EBV) Microvascular disease Hemolytic-uremic syndrome | Blood clots Bilateral stones Intraabdominal tumors (e.g., Burkitt’s lymphoma) Posterior urethral valves |
EBV, Epstein-Barr virus; IV, intravascular; NSAIDs, nonsteroidal antiinflammatory drugs; TBW, total body water.
EVALUATION
Can Renal Function Be Estimated Easily?
The most reliable, straightforward, and simple method to estimate renal function in children uses height and serum creatinine to calculate creatinine clearance with the formula in Table 65-2. Height serves as a surrogate of muscle mass. This approach should only be used when the patient is in a steady state with respect to renal function.
Table 65-2 Formula for Estimation of Glomerular Filtration Rate (GFR) in Children*
| Age of Child | Mean Value of k |
|---|---|
| Low-birth-weight infant (< 1 year) | 0.33 |
| Full-term infant (< 1 year) | 0.45 |
| 2–12 years | 0.55 |
| 12–17 years (female) | 0.55 |
| 12–17 years (male) | 0.7 |
* GFR (ml/min/1.73 m2) = [k × length or height (in cm)] ÷ serum creatinine (mg/dl). From Schwartz GJ, Brion LP, Spitzer A: The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents, Pediatr Clin North Am 34:571, 1987.
How Might a Patient with Acute Renal Failure Present?
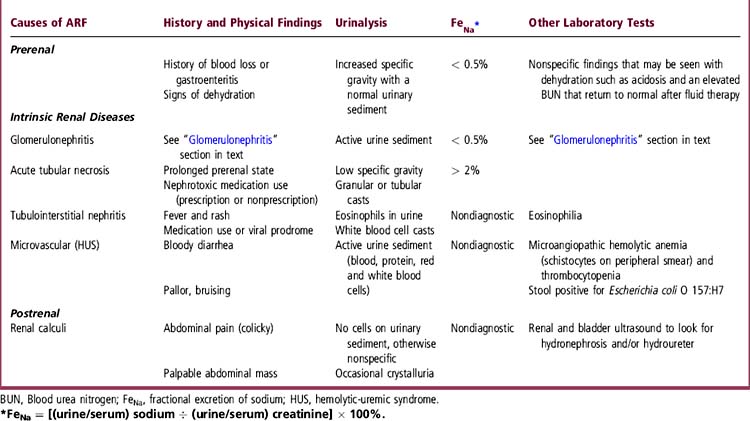
ARF commonly presents with oliguria, edema, hypertension, and fatigue or lethargy. Absence of hypertension may indicate low circulating volume, as in dehydration. ARF can occur with either normal or elevated urine output, the latter especially with tubulointerstitial disease. A patient with ARF might have only vague symptoms, so it is important to consider renal causes in the differential diagnosis of the symptom complex, to look for hypertension and edema, and to consider blood and urine tests. Lethargy and altered mental status can result from accumulation of “uremic” toxins. ARF can occasionally occur in a completely asymptomatic patient. Table 65-3 lists causes, presenting features, and evaluation of ARF.
How Can I Determine the Cause of Acute Renal Failure?
History, physical examination, and the initial laboratory tests used to diagnose the cause of ARF are listed in Table 65-3. The fractional excretion of sodium (FeNa) is particularly useful to differentiate acute tubular necrosis from prerenal causes, especially when urine output is low. This distinction is important because prompt intervention may facilitate renal recovery when ARF results from a potentially reversible cause, such as volume depletion. Even patients with intrinsic or postrenal causes for decreased GFR will benefit from appropriate fluid and electrolyte therapy if volume-depleted.
TREATMENT
How Do I Care for a Patient with Acute Renal Failure?
Management depends on the underlying cause. General measures include the following:
 Monitor blood pressure and manage hypertension
Monitor blood pressure and manage hypertension
 Limit fluid intake, except in prerenal ARF
Limit fluid intake, except in prerenal ARF
 Correct hyperkalemia with intravenous calcium, insulin and glucose, beta-adrenergic agonists, or oral potassium-binding resins
Correct hyperkalemia with intravenous calcium, insulin and glucose, beta-adrenergic agonists, or oral potassium-binding resins
 Prevent further insult to the kidneys by minimizing exposure to nephrotoxic agents and modifying drug dosages for the level of renal function
Prevent further insult to the kidneys by minimizing exposure to nephrotoxic agents and modifying drug dosages for the level of renal function
 Optimize nutritional intake to minimize the hypercatabolic state often associated with ARF
Optimize nutritional intake to minimize the hypercatabolic state often associated with ARF
CHRONIC KIDNEY DISEASE
ETIOLOGY
What Is Chronic Kidney Disease?
Chronic kidney disease (CKD) refers to impaired renal function, irrespective of the GFR, that persists for at least 3 months. The terms chronic renal insufficiency (CRI) and chronic renal failure (CRF) refer to the degree of GFR impairment and are no longer used. There are 5 stages of CKD based on the severity of renal impairment (Table 65-4). A patient does not need to have reduced GFR to be categorized as having CKD. A patient with stage I CKD has normal GFR with reduced renal mass, either acquired or congenital, and must be monitored for possible worsening of renal function. A patient with stage V CKD has end-stage renal disease (ESRD) and may need dialysis or renal transplantation. Loss of renal function causes impairment of other organ systems. Incidence of CKD and ESRD in children is less than 15 cases per million population in North America.
Table 65-4 Classification of Chronic Kidney Disease (CKD)
| Stage of CKD | Description |
|---|---|
| Stage I | Kidney damage with normal or even higher than normal GFR (> 90 ml/min/1.73 m2 surface area) (e.g., patients with renal scarring/reflux nephropathy, or diabetic nephropathy) |
| Stage II | Mild impairment of renal function (GFR 60–89 ml/min/1.73 m2 surface area) |
| Stage III | Moderate impairment of renal function (GFR 30–59 ml/min/1.73 m2 surface area) |
| Stage IV | Severe impairment of renal function (GFR 15–29 ml/min/1.73 m2 surface area) |
| Stage V | Kidney failure (GFR < 15 ml/min/1.73 m2 surface area or patient on dialysis) |
GFR, Glomerular filtration rate.
EVALUATION
What Is the Laboratory Evaluation for Suspected Chronic Kidney Disease?
The initial laboratory approach to CKD mirrors that for ARF (Table 65-3). Laboratory tests useful in the long-term management of children with CKD include serum electrolytes, blood urea nitrogen, serum creatinine, calcium and phosphorus, parathyroid hormone level, and the complete blood count (CBC). Other tests depend on the disease that caused the CKD.
How Can I Tell If Renal Failure Is Acute or Chronic?
Clues that a patient with renal failure has CKD include the following:
TREATMENT
How Do I Care for a Patient with Chronic Kidney Disease?
 Prevent or slow the decline in renal function, if possible
Prevent or slow the decline in renal function, if possible
 Treat complications of renal failure, such as
Treat complications of renal failure, such as
 Hyperparathyroidism, by limiting dietary phosphorus intake, using dietary phosphate binders, and prescribing vitamin D
Hyperparathyroidism, by limiting dietary phosphorus intake, using dietary phosphate binders, and prescribing vitamin D Prevent further insults to the kidneys by avoiding nephrotoxic medications and aggressively treating hypertension and proteinuria, if present
Prevent further insults to the kidneys by avoiding nephrotoxic medications and aggressively treating hypertension and proteinuria, if present
 Provide psychosocial and emotional support to the child and family
Provide psychosocial and emotional support to the child and family
GLOMERULONEPHRITIS
ETIOLOGY
What Is Acute Glomerulonephritis?
Glomerulonephritis (GN) is a syndrome of impaired renal function (elevated serum creatinine), some degree of oliguria, volume overload (edema, hypertension, and pulmonary vascular congestion), and hematuria of glomerular origin (see Chapter 52). It is caused by glomerular inflammation. In mild cases, hematuria may be the only sign of GN. When the onset is abrupt, GN is referred to as acute GN.
What Causes Acute Glomerulonephritis?
Causes of acute GN are listed in Table 65-5. Postinfectious GN is the most common form in children and occurs after infection by Streptococcus pyogenes (pharyngitis, or less commonly impetigo). Signs and symptoms of GN usually appear 10 to 14 days after the infection. The infection can sometimes be entirely asymptomatic. Postinfectious GN is mediated by an incompletely understood autoimmune process. In contrast, GN caused by IgA nephropathy (“Berger’s disease”) is exacerbated by infections, and symptoms appear at the same time as the intercurrent illness.
Table 65-5 Causes of Glomerulonephritis (GN) in Children
| Primary or idiopathic |
| Berger’s disease (IgA nephropathy) |
| Idiopathic membranoproliferative GN |
| Idiopathic FSGS |
| Idiopathic membranous nephropathy |
| Secondary |
| Postinfectious GN |
| Henoch-Schönlein purpura nephritis |
| Secondary membranoproliferative GN |
| Hepatitis B or C |
| Bacterial endocarditis/shunt nephritis |
| Systemic lupus erythematosus |
| Hereditary nephritis (Alport syndrome) |
| Antineutrophilic cytoplasmic antibody-positive conditions (vasculitides) |
| Wegener’s granulomatosus |
| Microscopic polyangiitis |
| Goodpasture’s disease (rare) |
Note: Although disease processes that fall under the category of hemolytic-uremic syndrome technically fulfill all the criteria for acute GN, they are not truly regarded as glomerulonephritides.
FSGS, Focal segmental glomerulosclerosis.
EVALUATION
How Do I Evaluate for Glomerulonephritis
 History: Tea- or cola-colored urine, oliguria, and edema
History: Tea- or cola-colored urine, oliguria, and edema
 Physical examination: Hypertension, peripheral edema, pulmonary vascular congestion or pulmonary edema, and heart failure
Physical examination: Hypertension, peripheral edema, pulmonary vascular congestion or pulmonary edema, and heart failure
 Serum total protein and albumin (see “Nephrotic Syndrome”)
Serum total protein and albumin (see “Nephrotic Syndrome”)
 Complete blood count (dilutional anemia; thrombocytopenia in autoimmune diseases)
Complete blood count (dilutional anemia; thrombocytopenia in autoimmune diseases)
What Further Tests Are Needed?
The cause of GN is identified from history, physical examination, and selected tests (Table 65-6). C3 complement and anti-neutrophil cytoplasmic antibody (ANCA) levels help differentiate amongst the various causes of GN. Renal biopsy, when indicated, can identify the underlying etiology, provide information about the severity of the GN, verify a clinical diagnosis, or determine the degree of chronicity. In some diseases, such as systemic lupus erythematosus, a biopsy can distinguish the subclasses of GN, which has therapeutic and prognostic importance.
Table 65-6 Etiologic Evaluation of a Child with Glomerulonephritis
| Disorder | History and Examination | Laboratory Tests |
|---|---|---|
| Postinfectious GN | Pharyngitis/impetigo (recent) | Transiently depressed C3 and C4 (6–8 weeks) |
| Gross hematuria preceding edema | Rapid streptococcal antigen; ASO titer | |
| IgA nephropathy | Recurrent gross hematuria precipitated by viral infections or exercise | None |
| Idiopathic MPGN | Not specific: fatigue, anemia | Persistently low C3/C4 |
| HSP | Syndrome: purpuric skin rash, periarthritis, abdominal pain, and glomerulonephritis | None: Clinical diagnosis Diagnosis confirmed by IgA deposits on skin and renal biopsy. If tested, ANA, C3/C4, and ANCA should be negative |
| Hepatitis B or C | Blood transfusions, sexual activity, or IV drug abuse | Hepatic transaminases |
| Jaundice | Hepatitis B surface antigen | |
| Maternal hepatitis | Hepatitis C antibody | |
| SSx of chronic liver disease (+/−) | C3/C4 (persistently depressed) | |
| SLE | SSx of SLE (see Chapter 70) | C3 and C4 (depressed) |
| ANA | ||
| dsDNA/Sm antibodies | ||
| Alport’s syndrome | Family history of renal failure | Genetic testing possible in some families |
| Hearing loss or ocular abnormalities | ||
| ANCA-positive GN | Respiratory problems, sinusitis, skin rash, constitutional symptoms | ANCA (c and p) |
ANA, Antinuclear antibody; ANCA, antineutrophilic cytoplasmic antibody; ASO, antistreptolysin O test; C3 and C4, third and fourth components of complement; dsDNA, double-stranded DNA; GN, glomerulonephritis; HSP, Henoch-Schönlein purpura; IgA, immunoglobulin A; IV, intravenous; MPGN, membranoproliferative glomerulonephritis; SLE, systemic lupus erythematosus; Sm, Smith; SSx, signs and symptoms +/−, variable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree