start timer
 don’t drop them (use a towel if being passed to you – they’re very slippery when you have gloves on)
don’t drop them (use a towel if being passed to you – they’re very slippery when you have gloves on)
 dry vigorously and discard wet towel
dry vigorously and discard wet towel
 wrap in dry towel
wrap in dry towel
 assess:
assess:
– airway
– breathing
– heart rate
– tone
– colour.
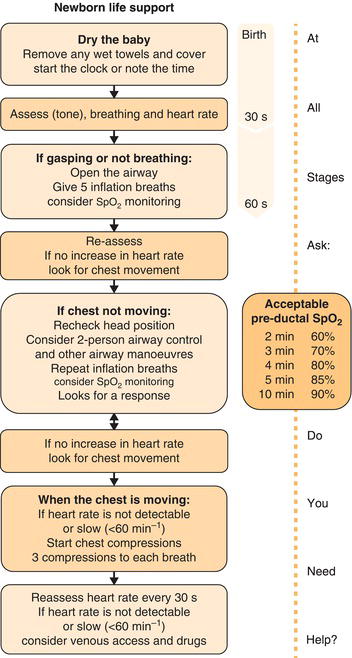
Figure 9.1 Newborn life support algorithm. Reproduced with permission from Resuscitation Council UK.
 At least two clean, dry towels should be laid out on the Resuscitaire.
At least two clean, dry towels should be laid out on the Resuscitaire. Turn on the heater (usually to a ‘prewarm’ setting) to start warming the towels.
Turn on the heater (usually to a ‘prewarm’ setting) to start warming the towels. Turn on the overhead light on the Resuscitaire.
Turn on the overhead light on the Resuscitaire. Check that there is a stethoscope on the Resuscitaire or you have your own with you.
Check that there is a stethoscope on the Resuscitaire or you have your own with you. Check that oxygen and air supplies are attached at the wall or to cylinders at the back.
Check that oxygen and air supplies are attached at the wall or to cylinders at the back. Make sure the air-oxygen ‘blender’ is initially set to 21% oxygen, i.e. air only.
Make sure the air-oxygen ‘blender’ is initially set to 21% oxygen, i.e. air only. Check masks of appropriate size are available (e.g. if baby is known to be preterm, get smaller masks out).
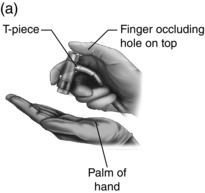
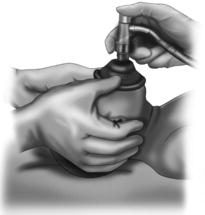
Check masks of appropriate size are available (e.g. if baby is known to be preterm, get smaller masks out). Check the inflation pressure is set to roughly 30 cmH2O (or 20–25 cmH2O for preterms). You can test this by taking the mask off and occluding the end of the T-piece with your hand before inflating (Fig. 9.2).
Check the inflation pressure is set to roughly 30 cmH2O (or 20–25 cmH2O for preterms). You can test this by taking the mask off and occluding the end of the T-piece with your hand before inflating (Fig. 9.2). Attach the Yankauer sucker (see Fig. 9.2) to suction and check it is working by obscuring the end (you should see the pressure gauge rise).
Attach the Yankauer sucker (see Fig. 9.2) to suction and check it is working by obscuring the end (you should see the pressure gauge rise). Check the oxygen saturation monitor is available and the sensor is connected to the machine.
Check the oxygen saturation monitor is available and the sensor is connected to the machine. Check that you have the appropriate laryngoscopes (one long and one short blade) and that they are both lighting up properly when opened.
Check that you have the appropriate laryngoscopes (one long and one short blade) and that they are both lighting up properly when opened. Check that tracheal tubes are available on the Resuscitaire for rare cases when the baby requires intubation (by someone experienced).
Check that tracheal tubes are available on the Resuscitaire for rare cases when the baby requires intubation (by someone experienced). Check you have oropharyngeal (GUEDEL) AIRWAYS available. Again, check that you have several sizes but you can usually anticipate likely size.
Check you have oropharyngeal (GUEDEL) AIRWAYS available. Again, check that you have several sizes but you can usually anticipate likely size. Top Tip
Top Tip Gestation of baby (if preterm, you may need help)
Gestation of baby (if preterm, you may need help) Risk factors for sepsis (prolonged rupture of membranes, maternal group B strep, maternal fever)
Risk factors for sepsis (prolonged rupture of membranes, maternal group B strep, maternal fever) Reason for emergency c-section/instrumental delivery/calling you to come to vaginal delivery (e.g. fetal bradycardia on cardiotocography [CTG] or meconium-stained liquor)
Reason for emergency c-section/instrumental delivery/calling you to come to vaginal delivery (e.g. fetal bradycardia on cardiotocography [CTG] or meconium-stained liquor)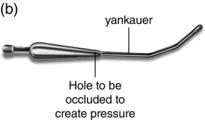
Figure 9.3 Opening the airway of an infant using a head tilt and chin lift. (a) Airway occluded. (b) Airway opened using head tilt and chin lift.

If the answer to any of these questions (particularly breathing and heart rate) is ‘no’ then you need to do something about it. Try each of the following in turn and reassess using the above questions every 30 sec.
Stimulate and airway manoeuvre
Stimulate by rubbing the back or soles of feet with the towel. To open the airway, you need to bring the baby’s head to a neutral position (i.e. so that their face is parallel to the surface on which they are lying). Newborn babies tend to have a prominent occiput which can make achieving this difficult; sometimes placing something under their shoulders can help with this. Be careful not to overextend the neck as this can occlude the airway.
Reassess
Most babies should have established spontaneous breathing by roughly 90 sec of age. If they are still not breathing or the heart rate remains low after stimulation and airway positioning, move to giving inflation breaths. Whilst you are still learning, it can be difficult assessing if breathing is adequate. If you are unsure, it is far better to give the inflation breaths than not.
Give five inflation breaths
Ensure that you have positioned the head so that the airway is open whilst delivering inflation breaths. These inflation breaths should be about 2 sec duration each. Use the T-piece apparatus (which should be available on virtually all RESUSCITAIRES now) (see Fig. 9.2) as it allows you to deliver more accurate pressures and is less cumbersome than the bag and mask. Your eyes need to be on the baby’s chest to check that it is moving as you deliver the breaths so to keep track of time count ‘1 and 2 and 3 and’ as you give each breath. This takes about 2 sec even if you’re stressed and talking quickly! You can keep track of how many breaths you’ve given this way too by counting ‘2 and 2 and 3 and… 3 and 2 and 3 and…’ etc. up to 5.
Reassess
If the baby’s condition has still not improved at this stage, consider putting out a crash call (if you haven’t already) in order to get more help.
Consider oxygen saturation monitoring
Ask for help from whomever is already in the room to put an oxygen saturation probe on whilst you continue to manage the airway. This can give you an objective measure of progress and will also give you the baby’s heart rate. Make sure that you place the probe on the right hand in order to record PREDUCTAL readings. Acceptable preductal oxygen saturation levels increase gradually over the first few minutes of life:
 2 min 60%
2 min 60%
 3 min 70%
3 min 70%
 4 min 80%
4 min 80%
 5 min 85%
5 min 85%
 10 min 90%.
10 min 90%.
Further inflation breaths or regular breaths
If you have delivered your inflation breaths successfully then you should start to see a rapid increase in the baby’s heart rate. If the heart rate remains low then assume that this is because your inflation breaths weren’t successful and try again (possibly using the two-person technique, with a jaw thrust, for delivery of breaths to improve chances of success – see Fig. 9.4). Watch carefully to see if the chest rises.
If you are sure that you saw the chest rise when delivering the inflation breaths and/or the baby’s heart rate has increased but the baby is not yet breathing spontaneously then continue regular breaths at a rate of 30–40 per minute until the baby establishes spontaneous breathing.
 Top Tip
Top TipCalculating Apgar scores
Apgar scores are still used as an approximation of how well or otherwise a baby is progressing in the minutes immediately following delivery. Their primary aim is to show how successful resuscitation efforts have been and over what period of time. They are recorded as scores at 1, 5 and 10 min. They are not really used at the time to inform resuscitation decisions but instead are calculated afterwards to give others an idea of the baby’s condition and response to resuscitation. The score given to a baby can be a rather subjective measure and the important thing is to see improvement over time. Some labour notes will contain a specific table in which to record the Apgar scores.
| > 100 | 2 points |
| <100 | 1 point |
| Absent | 0 points |
| Crying | 2 points |
| Slow (irregular) | 1 point |
| Absent | 0 points |
| Active motion | 2 points |
| Some flexion of extremities | 1 point |
| Limp | 0 points |
| All pink | 2 points |
| Pink body, blue extremities | 1 point |
| Pale, blue | 0 points |
| Strong cry | 2 points |
| Weak cry | 1 point |
| No response | 0 points |
Adapted from Dr Virginia Apgar’s original paper published in 1953.
Newborn baby checks
This is a screening process to help rule out any clinically detectable abnormalities before the baby is discharged from hospital. It is also an opportunity for parents to ask questions about the baby so be prepared to be asked all sorts of weird and wonderful things. Be honest if you don’t know the answer and also bear in mind that for questions about the minutiae of childcare, the answer may well be ‘It probably doesn’t matter which you choose to do’. It may be helpful to suggest that they refer to a parenting book, such as Your Baby Week by Week (Cave and Fertleman 2007), for these kinds of details.
In order to be able to detect abnormalities, you need to know what they look like! A useful website for learning about some of these, with great photos and explanations, is http://newborns.stanford.edu/Residents/Exam.html.
Different hospitals will have different methods of recording outcomes of the baby check. currently an electronic system for recording baby checks (Newborn and Infant Physical Examination Programme) is being piloted at some centres. Make sure that you know how your hospital expects you to record findings of the baby checks. It is also important to know what to do about any abnormalities that you do find. Many hospitals will have guidelines on how and what follow-up to arrange for common findings (e.g. sacral dimple or risk factors for developmental dysplasia of the hips). See Table 9.1 for common normal and abnormal findings.
At first baby checks can take quite a long time to do but you will soon develop ways of performing them more efficiently. Here are some pointers for what to include.
First of all, check through the maternity notes for any problems you need to be aware of and ask the mother about any problems during pregnancy or delivery. Specific things to look for in the notes and to ask the parents are as follows.
 At what gestation was baby born?
At what gestation was baby born?
 Any anomalies identified on 20-week scan?
Any anomalies identified on 20-week scan?
 Down syndrome screening performed? Less than 1 in 150 is defined as low risk (e.g. 1 in 200 is low risk)
Down syndrome screening performed? Less than 1 in 150 is defined as low risk (e.g. 1 in 200 is low risk)
 Maternal antenatal screening blood tests (e.g. rubella, HIV, Hep B, blood group etc.)
Maternal antenatal screening blood tests (e.g. rubella, HIV, Hep B, blood group etc.)
 Maternal Group B strep
Maternal Group B strep
 Maternal diabetes, genital herpes, HIV, Hep B or other chronic conditions
Maternal diabetes, genital herpes, HIV, Hep B or other chronic conditions
 Family history of developmental dysplasia of the hip?
Family history of developmental dysplasia of the hip?
 Family history of congenital heart disease?
Family history of congenital heart disease?
 Family history of any inherited disorders?
Family history of any inherited disorders?
 Baby lying breech in third trimester?
Baby lying breech in third trimester?
 Method of delivery?
Method of delivery?
 Any social concerns?
Any social concerns?
Also check in the baby’s notes or postnatal notes and ask the parents the following.
Table 9.1 Common findings at newborn checks – normal and not normal.
| Organ | Normal finding | Follow-up or senior advice needed |
| Skin | Dermal melanosis (‘blue spots’) Erythema toxicum Milia Sebaceous hyperplasia Dry skin | Naevus flammeus (port-wine stain) – can be associated with other abnormalities |
| Head and skull | Moulding – abnormal shaped skull, resolves spontaneously Fontanelles soft Caput – resolves spontaneously | Small head circumference (50th centile 35 cm) – plot on growth chart along with birth weight, should be on similar CENTILES Cephalohaematoma – at risk of jaundice |
| Ears | Low-set – if you draw an imaginary line from eyes out around the skull, the ears should cross or touch this line Incomplete folding of helices of the ears | |
| Eyes | Subconjunctival haemorrhage Oedema of eyelids | Conjunctivitis Cataracts |
| Mouth | Epstein pearls Tongue tie – rarely needs division | Cleft palate |
| Neck and clavicles | Clavicular fracture | Goitre |
| Chest | Breast buds (influence of maternal hormones) | Widely spaced nipples |
| Arms and hands | Symmetrical movements and normal posture of both arms | Syndactyly Polydactyly Single palmar crease |
| Abdomen | Small liver edge palpable | Spleen palpable Other abdominal mass |
| Umbilical cord | Dried out Small, reducible umbilical hernia | Discharge, odour or erythema of skin surrounding umbilical cord |
| Genitalia | White vaginal discharge Small spots of vaginal blood (pseudomenses) Patent anus, normal position and size | Hydrocoele – GP follow-up to ensure resolution One undescended testicle – GP follow-up to ensure resolution Bilateral undescended testes – check carefully for other signs of ambiguous genitalia, needs senior review and abdominal ultrasound Hypospadias – warn parents child must not be circumcised |
| Legs and feet | Both femoral pulses palpable | Talipes equinovarus (club foot) Syndactyly Polydactyly Dislocatable hips (pressure on flexed knees to push hip posteriorly out of joint) or dislocated hips (clunk of hip back into joint on abduction of hips) – needs urgent referral |
| Back and spine | Small shallow dimple (can see the base) in midline in gluteal crease with no associated skin changes Dermal melanosis over buttocks | Prominent tuft of hair over sacral spine Deep dimple over sacral spine |
| Reflexes | Moro reflex – should have symmetrical movement of both arms |
GP, general practitioner.
 Required resuscitation at birth?
Required resuscitation at birth?
 Apgar scores at delivery?
Apgar scores at delivery?
 Vitamin K given? If yes, was it intramuscular or oral? (If given orally then the baby will need to be given two further oral doses – you may be responsible for arranging this or making the GP aware)
Vitamin K given? If yes, was it intramuscular or oral? (If given orally then the baby will need to be given two further oral doses – you may be responsible for arranging this or making the GP aware)
 Method of feeding and is the baby feeding well?
Method of feeding and is the baby feeding well?
 Has the baby passed urine and meconium within first 24 h?
Has the baby passed urine and meconium within first 24 h?
 If observations have been done for the baby, are they normal?
If observations have been done for the baby, are they normal?