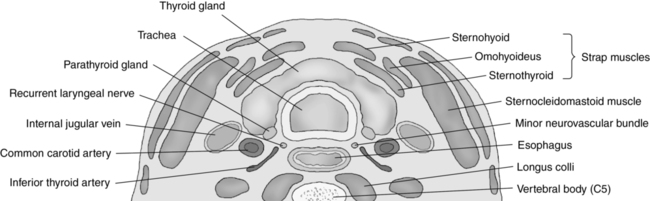
CHAPTER 17 a congenital diverticulum of the brachial cleft located directly below the angle of the mandible. bulging of the eyeballs; associated with hyperthyroidism. subacute thyroiditis secondary to a viral infection. a pronounced swelling of the neck caused by an enlarged thyroid gland. an excessive amount of calcium in the blood; associated with hyperparathyroidism. excessive function of the parathyroid glands; may lead to osteoporosis and nephrolithiasis. hyperactivity of the thyroid gland; associated with Graves disease. a deficiency of calcium in the blood; associated with hypoparathyroidism. decreased activity of the thyroid gland; associated with Hashimoto disease. a transient thyroiditis seen following pregnancy. an embryonic remnant cyst located between the isthmus of the thyroid and the tongue. • Maintain body metabolism, growth, and development. • Iodine is processed to manufacture, store, and secrete hormones: thyroxine, triiodothyronine, and calcitonin. • Secretion of thyroid hormones is primarily controlled by the thyroid-stimulating hormone produced by the pituitary gland. • Left originates from the aortic arch. • Right arises from the innominate (brachiocephalic) artery. • Ascend the anterolateral aspect of the neck. • Lie medial to the internal jugular vein and lateral to the thyroid lobe. • Course deep to the sternocleidomastoid muscles. • Bifurcate into the external and internal carotid arteries. • Arise from the first segment of the subclavian artery. • Provide blood to the posterior brain. • Lie in the posterior neck, ascending through the transverse processes of the spine. • Left and right vertebral arteries join to form the basilar artery at the base of the skull. • Basilar artery terminates in the posterior aspect of the circle of Willis. • The superior and inferior thyroid arteries supply arterial flow. • Superior thyroid artery arises from the external carotid artery. • Inferior thyroid artery arises from the thyrocervical artery. • Superior, middle thyroid veins drain into the internal jugular vein; inferior thyroid vein drains into the innominate vein. • Isthmus—0.2 to 0.6 cm in height. • Thyroid glands (adult)—4.0 to 6.0 cm in length, 2.0 cm in height, and 2.0 cm in width. • Thyroid glands (pediatric)—2.0 to 3.0 cm in length, 0.2 to 1.2 cm in height, and 1 to 1.5 cm in width. • Parathyroid glands—up to 6 mm in length, 2 mm in height, and 4 mm in width. • Thyroid lobes and isthmus appear as homogeneous solid structures demonstrating a medium-gray echo pattern. • Sternocleidomastoid and strap muscles appear hypoechoic when compared with the normal thyroid gland. • Longus colli muscles appear hyperechoic when compared with the normal thyroid gland. • Parathyroid glands are flat, bean-shaped hypoechoic structures located posterior and medial to the thyroid lobes. • Carotid arteries and jugular veins appear as anechoic tubular structures demonstrating internal vascular flow. • Use the highest-frequency linear transducer possible to obtain optimal resolution for penetration depth. • Focal zone(s) at or below the place of interest. • Sufficient imaging depth to visualize structures immediately posterior to the region of interest. • Increase the dynamic range setting when imaging the thyroid glands. • Harmonic imaging can be used to reduce artifactual echoes within anechoic structures. • Spatial compounding can be used to improve visualization of structures posterior to a highly attenuating structure. • Use Doppler settings for low-flow to medium-flow states. • Place the patient in a supine position with the neck extended. • A pillow may be placed under the upper back to hyperextend the neck. • Evaluate and document both thyroid lobes from the superior to inferior borders and the medial to lateral borders in two imaging planes. • Document length, width, and height of each thyroid lobe. • A convex abdominal transducer can be used to measure enlarged thyroid glands. • Document thickness of isthmus. • Document length, width, and height of any abnormality. • Demonstrate color Doppler flow within each thyroid lobe. • With multinodular goiters, include measurements of the largest nodules for serial comparison. • Documentation and measurement of any abnormality in two scanning planes with and without color Doppler should be included.
Neck
Physiology
Function of the thyroid glands
Vasculature of the neck
Common carotid arteries
Vertebral arteries
Vasculature of the thyroid glands
Size
Sonographic appearance
Technique
Preparation
Examination technique and image optimization