Introduction
Nausea and vomiting of pregnancy (NVP) affects about 75% of pregnant women, with 25% reporting nausea alone and 50% reporting both nausea and vomiting. Hyperemesis gravidarum (HG) occurs in 0.3–2% although populations with significantly higher rates have been reported. It is identified by otherwise unexplained intractable vomiting and dehydration. Significant weight loss, usually > 5% of pre-pregnancy weight, confirms the diagnosis.
Maternal mortality was about 10% until the middle of the 20th century. Maternal death is now uncommon but it still does occur, either related directly to HG or to therapeutic interventions. It is the most common cause of hospitalization in the first half of pregnancy and the cost of hospitalization alone is estimated to be more than $500 million annually.
Hyperemesis gravidarum is clearly related to a product of placental metabolism since it does not require the presence of the fetus and it occurs commonly in molar gestation. More than 20 studies about hormonal changes in NVP have been published in the last 30 years and despite some conflicting information, the evidence points towards hCG and estradiol as having a role.
There is a strong temporal association between hCG concentrations and the time of peak symptomatology. hCG is also a thyroid stimulator and biochemical hyperthyroidism is commonly seen in HG. It has been difficult, however, to directly link total hCG concentrations with the severity of NVP because its concentrations vary widely in the normal and NVP populations. This occurs because hCG is actually a family of isoforms which differ in their half-life and in their binding potency to the hCG, LH and TSH receptors. Isoforms lacking the carboxyl-terminal portion, for example, are more potent stimulators of the TSH and LH receptor but have shorter half-lives. Hyperglycosylated hCG, on the other hand, has a longer half-life and a longer duration of action.
A link between the action of hCG and estradiol has been suggested because concentrations of hyperglycosylated hCG correlate with estradiol and the severity of nausea and vomiting (NV). It is hypothesized that stimulation of maternal ovarian production of estradiol (and possibly fetal production as well) increases maternal estradiol concentration. NV in women taking the combined oral contraceptive pill increases in direct correlation with the estradiol dose and a history of NV while taking estrogens is a risk factor for the development of HG.
Epidemiologic studies have in general identified some common threads between women with HG and other common NV syndromes such as postoperative and chemotherapy-related NV and include younger age, a history of motion sickness, history of migraines and earlier hour of the day. Of interest is that smoking is associated with decreased concentrations of hCG and estradiol and with less NVP while fetal female gender is associated with greater concentrations of hCG and more severe HG.
Evidence in support of a genetic predisposition to NVP includes the concordance in frequency of nausea and vomiting of pregnancy in monozygotic twins; that siblings and mothers of patients with NVP are more likely to be affected; the variation in the frequency of NVP among different ethnic groups; and the occurrence of NVP in women with inherited glycoprotein hormone receptor defects. The paternal genome may have a role as well since women with HG in one pregnancy for whom there was a different father in the next pregnancy had a 60% lower rate of recurrence HG.
For many years it was presumed that women suffering from HG were predisposed by something in their own psychologic make-up or by the circumstances of their lives. Numerous theories, drawn mostly from psychoanalysis, identified these women as rejecting the father of the baby, ambivalent about the pregnancy, rejecting their own feminity and either being too dependent on their mothers . . . or not dependent enough! One of the most influential studies concluded that women with HG had a hysterical personality type. At present, HG is not believed to be due to any particular psychologic state. In a recent survey, 93 of 96 women believed that HG had a biologic basis and that psychologic problems were secondary to the severe illness. Nevertheless, most of them also reported that friends, family members and caregivers implied that they were somehow in control of their disease state.
The development of food aversions in pregnancy (present in about 50% of women) is closely linked to the onset of nausea. In 64% of cases, the first occurrence of nausea was reported either in the week preceding the first food aversion or in the same week. These findings are consistent with a taste aversion learning mechanism, where foods paired with illness are subsequently avoided. The fact that cravings common in pregnancy do not follow this pattern is supportive of the same concept. Anticipatory vomiting associated with chemotherapy is thought to have a similar mechanism. Interestingly, the food aversions in pregnancy are similar to those that develop with chemotherapy in that they do not generally persist after the acute course of the primary stimulus ends; this is distinct from other conditioned responses which may persist for years. Uncontrolled case series have suggested a benefit of behavioral therapy or hypnosis in treatment of HG.
Embryo protection hypothesis
In the view of evolutionary biology, NVP is a mechanism that has evolved, along with food aversions, to prevent pregnant mothers from ingesting substances that may be harmful to the developing fetus such as infections in the food supply or other toxins. However, even if NVP and HG evolved as a protective phenomenon, this fetal benefit is no longer applicable.
Nausea and vomiting of pregnancy as a syndrome
Nausea and vomiting of pregnancy is better thought of as a syndrome with the final phenotype arising from different pathways. Thus, for example, the stimulus to HG is affected by placental mass (more common in multiple gestation) as well as by aberrant hCG production as in advanced molar gestation or in carriers of trisomy 21 fetuses. The paternal genotype within the placenta must play a role, as is shown by the effect of changing fathers on the recurrence risk of HG. Equally important, the way an individual mother responds to this stimulus is genetically mediated, as is shown by family studies of HG. The susceptibility of the mother varies depending on a number of factors that are recognized as mediating NV in other settings such as postoperative NV and chemotherapy-induced NV.
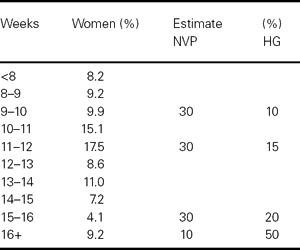
Prospective studies show that virtually all women who develop NVP will have some symptoms by 9 weeks’ gestation; 7% have symptoms before the time of the first missed period and 60% are symptomatic by 6 weeks. For the subset of women with HG, there is a tendency for early onset of symptoms and much greater overall duration. The timing of end of symptoms for NVP and HG is shown in Table 36.1.
Table 36.1 Time to cessation of NVP and HG
In addition to NV, associated complaints include excess salivation (ptyalism) in up to 60%. There is a common perception that women with more severe NVP are very sensitive to olfactory stimuli, but it has not been documented in objective studies. Rather, there is a change in the pleasurable (or, rather, lack of pleasurable) rating of odors, something similar to what is seen during chemotherapy-induced nausea.
Recent population-based studies have found that low pre-pregnancy BMI was associated with a higher risk of HG and that the effect was even stronger for women requiring hospitalization. Obesity appeared to decrease the risk of hospital admission for HG.
Laboratory abnormalities
A wide variety of laboratory abnormalities can be seen with HG, including suppressed TSH and/or elevations in free T4, elevated liver enzymes as well as bilirubin, amylase and lipase. These abnormalities resolve when the vomiting stops and do not require specific treatment. There is still insufficient awareness of the spectrum of these transient abnormalities, sometimes resulting in unnecessary antithyroid treatment, cholecystectomy or even termination of pregnancy. Rare cases of hepatic or renal insufficiency have been reported with HG but these are usually transient as well or due to other underlying disease.
Virtually all patients with transient hyperthyroidism related to HG will have a normal TSH after the vomiting stops. In such patients there is no history of symptoms preceding pregnancy, no goiter, no other systemic signs of hyperthyroidism (except occasionally tachycardia) and negative thyroid antibodies.
Severe metabolic/nutritional maternal complications of HG may include Werrnicke’s encephalopathy, beriberi, central pontine myelinolysis, hepatic insufficiency, acute tubular necrosis and peripheral neuropathy. Complications due to the mechanical stress of vomiting may include Mallory–Weiss tear of the esophagus, esophageal rupture, pneumomediastinum, retinal detachment and splenic avulsion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


