Fig. 22.1
Anterior rhinoscopy demonstrating a pale mass obstructing the nasal cavity
Nasal congestion.
No pulsation or expansion of lesion with crying, coughing, or straining.
Compression of the ipsilateral jugular vein does not result in expansion or pulsation of the mass (negative Furstenberg test).
Laboratory Data
Patients with nasal glioma typically do not have other underlying conditions. Routine lab workup including CBC, electrolytes, and coagulation studies are expected to be normal. However, presentation of these lesions is often in the setting of infection in which case there may be an elevated white blood cell count.
Imaging Evaluation
Imaging of these lesions is one of the most critical aspects of the workup. Approximately 10–20 % of nasal gliomas may appear with a fibrous stalk extending toward the base of skull with an underlying bony defect [5]. Cross-sectional imaging through the area of interest provides information regarding the masses’ size, location, and contents. Computerized tomography (CT) with contrast is the imaging study of choice to initially evaluate these lesions (Fig. 22.2). The images should be fine cuts and reformatted in the axial, coronal, and sagittal planes. CT provides some soft tissue detail, but is ideally suited to evaluate the bony anatomy and the presence of a defect in the anterior skull base (Fig. 22.3). However, in young infants, the anterior skull base is either not ossified or only partially ossified; additionally, CT only provides minimal information of soft tissue extent. Therefore, thin-section, high-resolution MRI is indicated in the workup of all of these patients. These images give additional information regarding the soft tissue contents of the mass and the presence of intracranial extension.
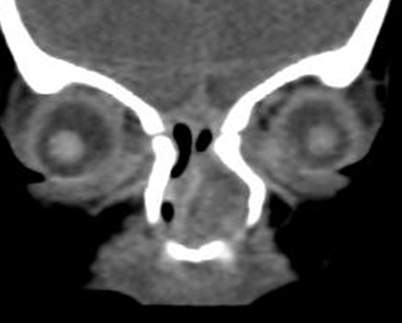
Fig. 22.2
Coronal CT scan demonstrating nasal glioma involving the left nasal cavity with extension toward the skull base
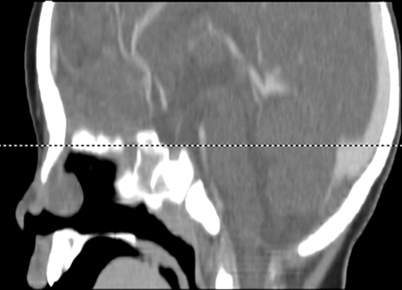
Fig. 22.3
Sagittal CT scan demonstrating nasal glioma with bony defect in the anterior cranial fossa. MRI would be needed to further characterize the soft tissue and intracranial extension
Pathology
Gliomas and encephaloceles are very difficult to distinguish on pathology alone . On histopathological examination, glial tissue may be the exclusive or predominant component in both lesions. Occasionally ependymal tissue will be identified in encephaloceles and can make the diagnosis of encephalocele more likely [7] (Fig. 22.4). Separation of the two entities is dependent largely on clinicopathologic correlation.
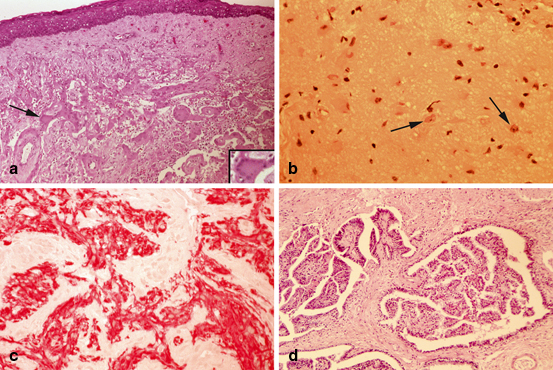
Fig. 22.4




Nasal glioma, light microscopy. a Meningothelial and glial tissue beneath squamous mucosa. A giant multinucleated meningothelial cell, indicated by an arrow, is seen at higher magnification in the inset. b Matured disorganized brain tissue with abundant glial component and occasional neurons (arrows). c Immunohistochemistry showing strong immunoreactivity of neuroglial tissue for glial fibrillary acidic protein (GFAP) is seen in red. d Cystic papillary structures in a background of neuroglial tissue represent choroid plexus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


