37 Musculoskeletal Disorders
 Anatomy and Physiology
Anatomy and Physiology
Long bones have a growth plate, or physis, at each end that separates the epiphysis from the diaphysis or shaft. Openings through this plate allow blood vessels to penetrate from the epiphysis. In the growth plate, chondrocytes produce cartilage cells, dead cells are absorbed, and the calcified cartilage matrix is converted into bone. The entire growth plate area is weaker than the remaining bone because it is less calcified. Because the blood supply to the growth plate comes primarily through the epiphysis, damage to epiphyseal circulation can jeopardize the survival of the chondrocytes. If chondrocytes stop producing, growth of the bone in that area stops (Fig. 37-1).
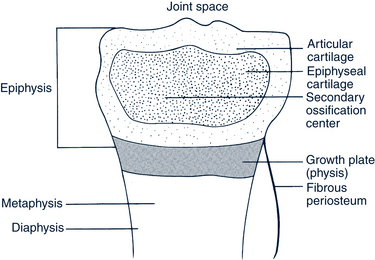
FIGURE 37-1 Anatomy of long bones.
(Modified from Shapiro F: Epiphyseal disorders, N Engl J Med 317:1702-1710, 1987.)
There are two ways that children’s bones grow. Longitudinal growth occurs in the ossification centers; changes in bone width and strength take place via intramembranous ossification. The length of long bones comes from growth at the epiphyseal plates while their diameter increases as a result of deposition of new bone on the periosteal surface and resorption on the surface of the medullary cavity. Growth of the small bones, hip, and spine comes from one or more primary ossification centers in each bone. Apophyses are the sites for connection of tendons to bone. In children these sites, similar to epiphyses, allow for growth and are weaker than bone. These sites can become inflamed with stress.
 Pathophysiology and Defense Mechanisms
Pathophysiology and Defense Mechanisms
Pathophysiology
Genetic Problems
Many orthopedic problems have a multifactorial inheritance pattern. Thus if one child in a family has a dislocated hip or scoliosis, the risks increase for other children. The pediatric provider needs to understand the genetic disorder to monitor related orthopedic problems, consider the genetic implications, and provide families with appropriate genetic information or refer them for genetic counseling (see Chapter 40).
Uterine Packing Deformations
The developing fetus moves its body parts frequently, and this movement influences musculoskeletal development. When the baby fills the uterine space, movements are restricted and body parts begin to assume a shape in which they are fixed. With in utero positioning, joints and muscle contractions can develop and are considered generally physiologic in nature. Orthopedic deformities of uterine compression include clubfoot, torticollis, hip dislocation, metatarsus adductus, equinovarus foot, calcaneovalgus foot, tibial bowing, hyperflexed hips, hyperextended knees, contractures, and internal tibial torsion (Wynshaw-Boris and Biesecker 2007). Fetal movement is required for proper development of the musculoskeletal system, and anything that restricts fetal movement can cause deformation from intrauterine molding. Two major intrinsic causes for deformations are neuromuscular disorders and oligohydramnios. Extrinsic causes are related to fetal crowding that restricts fetal movement. For a fetus in the breech position the incidence of deformations is increased 10-fold (Wynshaw-Boris and Biesecker, 2007). Infants with deformations caused by extrinsic causes have an excellent prognosis with corrections occurring spontaneously. Torsional and angular alignment issues can affect the long bones, most commonly those of the lower extremities. Because much of the bony structure is cartilaginous, molding occurs with relative ease. Thus in normal newborns, the tibias are normally bowed, and the hips have a 20- to 30-degree flexion (Hosalkar and Wells, 2007). Occasionally, a foot may be turned awkwardly, the legs might be fixed straight up with the feet near the ears, or the neck may be tipped to one side. Such positioning issues are outside the range of normal. The outcomes are deformities in various degrees. The longer the position is maintained, the more severe the problems are. In general, there is a tendency for bowing and late deformations to straighten; however, the effects related to in utero positioning may not fully abate until the child is 3 to 4 years old. More severe deformities (i.e., those significantly outside the range of normal) need to be referred to orthopedists for treatment as soon as they are found because a softer skeleton is easier to realign in a positive direction.
Injuries
There are approximately 2.6 million emergency department visits annually in the U.S. for sports-related injuries in children ages 5 to 24 years, with the highest percentage occurring in the 5- to 14-year-old male. This does not account for the children who present to their primary care physician for evaluation and treatment (Soprano and Fuchs, 2007). The unique differences in the pediatric skeletal system predispose children to injuries unlike those seen in adults. The important differences are the presence of periosseous cartilage, physes, and a thicker, stronger, more osteogenic periosteum that produces new bone called callus more rapidly and in great amounts. Joint injuries, dislocations, and ligament disruptions are infrequent in children (Gholve et al, 2007). Physeal fractures in preadolescent children are the most common musculoskeletal injuries seen. Clavicular fractures are seen at all ages ranging from a newborn birth injury to trauma in adolescence. They can occur as a result of direct or indirect injury and are most commonly associated with a fall (Benjamin and Hang, 2007).Tendinoses are seen infrequently in children but may occur in the young athlete in the rotator cuff from throwing motions and swimming, in the iliopsoas in dancers, and in the ankle of dancers, gymnasts, and figure skaters. Shoulder injuries can be acute or result from chronic overuse. Overuse injuries are common chronic injuries in children that are related to repetitive stress on the musculoskeletal system without sufficient time to recover. The repetitive use overwhelms normal reparative processes (Soprano and Fuchs, 2007). Management of traumatic injuries is discussed in Chapter 39.
Defense Mechanisms
Fracture Healing
Growth Plate Fractures
Fractures of the long bones can produce permanent deformities in children if the fracture occurs through the growth plate. The outcomes depend on the fracture location and type, the age of the child, the status of the blood supply to the physis, and the treatment. The Salter-Harris classification is based on the mechanism of injury, the relationship of the fracture line to the layers of physis, and the prognosis with respect to subsequent growth disturbance. There are five classifications (Fig. 37-2). Type I is the most frequent type of fracture that involves a fracture through the zone of hypertrophic cells of the physis with no fracture of the surrounding bone. Type II fractures are similar to type I except that a metaphyseal fragment is present on the compression side of the fracture. Growth disturbance in types I and II is rare.
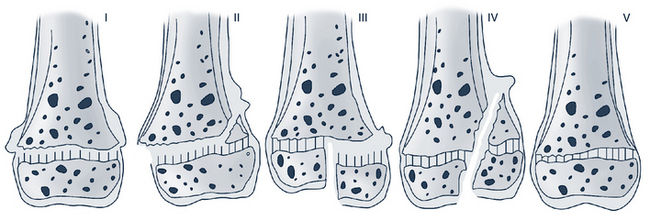
FIGURE 37-2 The types of growth plate injury as classified by Salter and Harris.
(From Salter RB, Harris WR: Injuries involving the epiphyseal plate, J Bone Joint Surg Am 45:587, 1963.)
Type III fracture involves physeal separation with fracture through the epiphysis into the joint. The fracture requires anatomic reduction, occasionally through an open approach. Type IV fracture involves the metaphysis, physis, and epiphysis. Type V fracture involves a compression or crushing injury to the physis. Type V fractures are rare and are difficult to diagnose initially due to the lack of radiologic signs. Types IV and V require anatomic reduction to prevent articular incongruity and osseous bridging across the physis. There are additional rare types of Salter-Harris fractures, types VI through IX. Type VI is an injury to the perichondral ring of LaCroix, a fibrous band that is continuous with the periosteum and a potential reservoir for growth-plate germ cells. Type VI fracture is seen in injuries about the medial malleolus and often requires later reconstructive surgery (Green and Swiontkowski, 2008).
 Assessment of the Orthopedic System
Assessment of the Orthopedic System
History
 Onset: Appearance of first symptoms; insidious or sudden; association with injury or strain; accompanied by any constitutional symptoms or signs (e.g., fever, malaise, swelling, ecchymosis)
Onset: Appearance of first symptoms; insidious or sudden; association with injury or strain; accompanied by any constitutional symptoms or signs (e.g., fever, malaise, swelling, ecchymosis) Pain: Location and character, course of radiation, severity, extent of disability produced, effect of various activities including weight bearing, relief measures, changes from day to night or from day to day, child’s refusing to move the painful part or assuming a pain-relieving position, effects of previous treatment, presence of pain or discomfort in other parts of the body
Pain: Location and character, course of radiation, severity, extent of disability produced, effect of various activities including weight bearing, relief measures, changes from day to night or from day to day, child’s refusing to move the painful part or assuming a pain-relieving position, effects of previous treatment, presence of pain or discomfort in other parts of the body Deformity: Character (swelling, inflammation, contracture, joint stiffness, unusual positioning, appearance); first appearance and who noted it; association with injury or disease; rate of change; extent of disability; a cosmetic problem or a cause of embarrassment
Deformity: Character (swelling, inflammation, contracture, joint stiffness, unusual positioning, appearance); first appearance and who noted it; association with injury or disease; rate of change; extent of disability; a cosmetic problem or a cause of embarrassment Injury: How, when (time and date), why, and where; mechanism or manner in which injury was produced; involvement in organized or competitive sports
Injury: How, when (time and date), why, and where; mechanism or manner in which injury was produced; involvement in organized or competitive sports Other factors or constraints: Type of shoe worn (e.g., platform shoes); use of backpack and amount of weight in backpack, amount of time spent at repetitive tasks or at computer station; sitting in TV squat or “W” position
Other factors or constraints: Type of shoe worn (e.g., platform shoes); use of backpack and amount of weight in backpack, amount of time spent at repetitive tasks or at computer station; sitting in TV squat or “W” position Pregnancy history and birth history: Breech delivery, shoulder presentation, multiple births, oligohydramnios, asphyxia at birth; maternal alcohol or substance abuse
Pregnancy history and birth history: Breech delivery, shoulder presentation, multiple births, oligohydramnios, asphyxia at birth; maternal alcohol or substance abuse Development history: Milestones met at appropriate age, such as first walking and sitting; delays in achieving gross or fine motor developmental milestones
Development history: Milestones met at appropriate age, such as first walking and sitting; delays in achieving gross or fine motor developmental milestonesPhysical Examination
Special orthopedic examination techniques are described in the following paragraphs.
Posture
• Pelvis and hips should be level. Place hands on the iliac crest to test for a pelvic tilt caused by limb length discrepancy.
• Legs should be symmetric in shape and size. The patellae should be straight ahead.
• The feet should point straight ahead, with an imaginary line from the center of the heel through the second toe. There should be an arch (except in babies, in whom a fat pad obscures the arch) and straight heel cords.
• The spine should be straight, and the back should look symmetric, with shoulder and scapula heights and waist angles equal. There should be slight lordotic curves at the cervical and lumbar areas.
 Special Examinations
Special Examinations
Hip Examinations
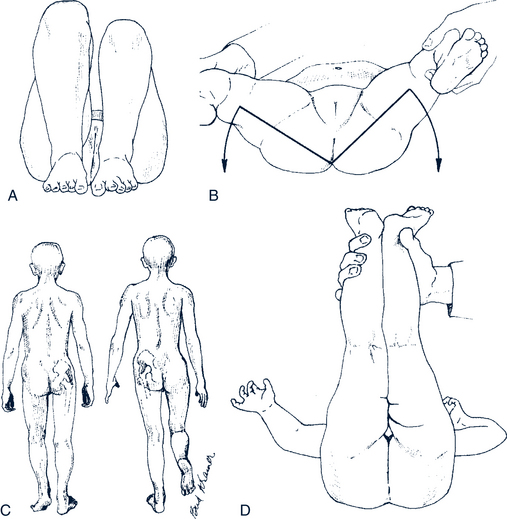
Galeazzi Maneuver
The Galeazzi sign can signal conditions that cause leg length discrepancies. The Galeazzi maneuver includes flexing the hips and knees while the infant or child lies supine, placing the soles of the feet on the table near the buttocks, and then looking at the knee heights for equality (Fig. 37-3, A). The Galeazzi sign is positive if the knee heights are unequal. However, it is not reliable in children with dislocatable but not dislocated hips or in children with bilateral dislocation.
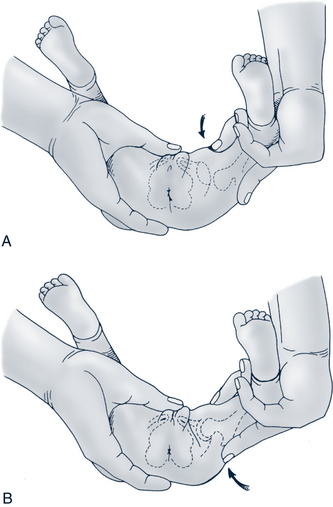
Barlow Maneuver
The Barlow maneuver dislocates an unstable or dislocatable hip posteriorly (Fig. 37-4, A). The infant is placed in the supine position with knees flexed. The hip is flexed, and the thigh is brought into an adducted position applying downward pressure. With hip instability the femoral head slips/drops out of the acetabulum or can be gently pushed out of the socket; this is termed a positive Barlow. The dislocation should be palpable as this maneuver is performed. The maneuver needs to be done gently in a noncrying neonate to keep from damaging the femoral head. The hips should be examined one at a time. The hip generally spontaneously relocates after release of the posterior force.
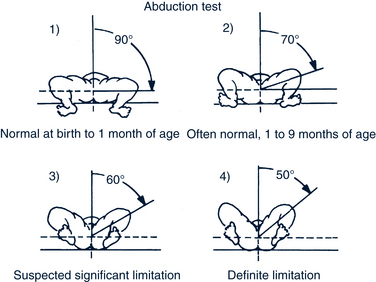
Ortolani Maneuver
The Ortolani maneuver can be done after the Barlow maneuver or separately (see Fig. 37-4, B). The Ortolani maneuver reduces a posteriorly dislocated hip. It is done to reduce a recently dislocated hip and is not done forcefully. The infant is in the supine position with both knees flexed and supported by the thumb and forefinger of the examiner. The thumb is placed near the lesser trochanter, and the pad of the second finger is positioned on the bony prominence of the greater trochanter. The leg is flexed at the hip and then abducted while pushing up with the fingers located over the trochanter posteriorly. The femoral head is lifted anteriorly into the acetabulum. A clunk and a palpable jerk are obtained as the femoral head is relocated. A mild clicking sound is not a positive Ortolani sign. These are common and normal sounds radiating from the knee or ankle that are fine, of short duration, and high pitched (Duderstadt and Schapiro, 2006). Of note, the hip may be dislocated easily only during the first month or two of life. The Ortolani maneuver is most likely to be positive in infants 1 to 2 months old. The examiner should not still be charting “no hip click” on examinations at 6 months old. Dislocation can occur late in infancy. However, if this occurs, the provider will note limited abduction on the side of the dislocation (Fig. 37-5).
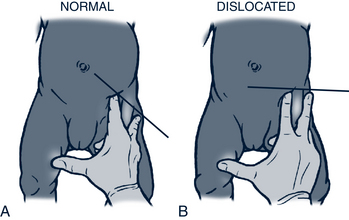
Klisic Test
The Klisic test provides an observational sign of hip placement. The examiner places the tip of the third finger of one hand over the greater trochanter and the index finger of the same hand on the anterior superior iliac spine. An imaginary line is then drawn between the index and third fingers. Normally, the imaginary line points to the umbilicus. If the hip is dislocated, the imaginary line points halfway between the umbilicus and the pubis (i.e., the line points below the umbilicus). The Klisic sign is another physical assessment marker of dislocation (Hosalkar et al, 2007b) (Fig. 37-6).
Trendelenburg Sign
The Trendelenburg test can be used to identify conditions that cause weakness in the hip abductors. The Trendelenburg sign is elicited by having the child stand and then raise one leg off the ground. If the pelvis (iliac crest) drops on the raised leg side, the sign is positive and indicates weak hip abductor muscles on the side that is bearing the weight. Normally the muscles around a stable hip are strong enough to maintain a level pelvis if one leg is raised (see Fig. 37-3, C). With bilaterally dislocated hips, a wide-based Trendelenburg limp is noted.
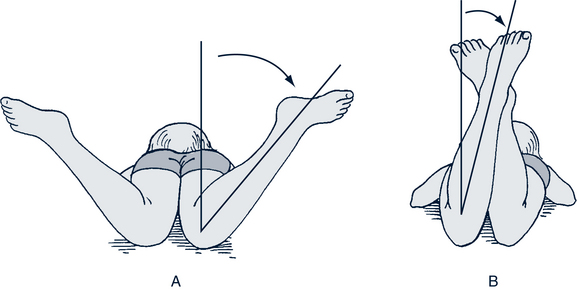
Medial (Internal) and Lateral (External) Rotations
The child is placed prone, and the knees are flexed 90 degrees. Medial rotation is measured as the legs are allowed to fall apart as far as possible, using gravity alone or with light pressure. The angle between vertical (0 degree) and the leg position is the medial rotation. It is measured for each leg (Fig. 37-7, A). Asymmetric hip rotation is abnormal. Lateral rotation is measured by allowing the legs to cross while the child is still prone. The angle between vertical and the leg position is measured for each leg (see Fig. 37-7, B). Again, asymmetric hip rotation is abnormal. By 1 year old, a normal child has approximately 45 degrees of internal and external hip rotation.
Back Examination
Adams Test or the Adams Forward Bend Position
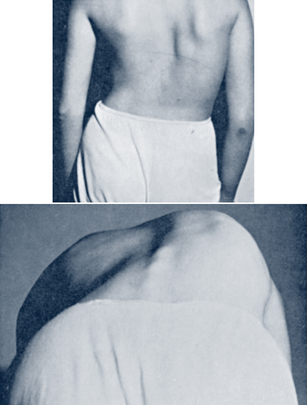
The Adams forward bend test (Adams test) looks for asymmetry of the posterior chest wall on forward bending. This position allows for evaluation of structural scoliosis. The child bends at the waist to a position of 90 degrees back flexion with straight legs, ankles together, and arms hanging freely or with palms together (in a diving position) but not touching the toes or floor (Fig. 37-8). The back is inspected for asymmetry of the height of the curves on the two sides or rib hump; the provider inspects the child’s back by looking at it from the rear and side positions. The examiner should be seated in front of the child to best visually scan each level of the spine. If a rib hump is present, a scoliometer, if available, can be used to measure the angular tilt of the trunk. A spinal rotation greater than 5 degrees measured by placing the scoliometer at the peak of the curvature indicates the need for further evaluation (Duderstadt and Schapiro, 2006). Other characteristics of scoliosis to look for include unequal scapula heights, unequal waist angles, unequal iliac crests or shoulders, asymmetry of the elbow to flank distance, and some deviation of the spine from a straight head-to-toe line. Looking primarily at the straightness of the spine, however, can be misleading because scoliosis involves both rotation and misalignment of the vertebrae. The Adams forward bending position accentuates the rotational deformity of scoliosis.
 Diagnostic Studies
Diagnostic Studies
Radiographs are an important diagnostic tool for the musculoskeletal system. Imaging should begin with standard radiographs of the area of concern. Anteroposterior and lateral views of the affected area, bone, or joint are typically ordered to analyze the anatomic structures. Views of both extremities may be ordered so that comparisons can be made. Computed tomography (CT) scans augment radiographs to detail specific areas of the body, especially in identification of soft-tissue lesions. CT is useful in detailing the relationship of bones to their contiguous structures. Magnetic resonance imaging (MRI) gives excellent visualization of joints, soft tissues, cartilage, and medullary bone. It can distinguish among various physiologic changes that occur in bone marrow related to age and disease process. Ultrasonography can provide information about cartilaginous areas or tissues not visible on radiograph. The test is highly sensitive for detecting effusion of the hip joint. Bone scans (scintigraphy) are more sensitive than radiographs, demonstrate abnormal uptake earlier than conventional radiographs, and are useful in detecting causes of obscure skeletal pain.
 Management Strategies
Management Strategies
Counseling
• The pathologic condition, including possible etiologies
• The prognosis with and without treatment
• Any genetic implications of the diagnosis
Exercise
With childhood obesity on the rise, there is a push to improve fitness and activity levels in children and adolescents. Physical activity needs to be promoted at home, in the community, and at school. Toddler and preschool-age children should participate in unorganized, supervised play including running, swimming, tumbling, throwing, and catching. School-age children can be encouraged to increase activity by unorganized outdoor free play, personal fitness (dance, yoga, running), recreational activities, and organized sports. During late childhood and adolescence, strength training may be added. Even children with disabling conditions can exercise in some way. (Refer to Chapter 13 for more in-depth discussion about activities and sports. Tables 13-2 and 13-5 provide some guidance regarding some specific medical conditions and sports participation.) Exercise for children should be fun and perceived as play, not work. Often physical therapists or the child’s orthopedist can provide ideas for safe, therapeutic play or sports activities. At school, children with orthopedic problems should engage in physical activities that are as much a part of the regular physical education class as possible.
Shoes
• Flexible sole—to allow as much free motion as possible; for young children, test to see if the shoe can be flexed in the parent’s hand
• Flat—do not allow high heels
• Foot shaped—avoid pointed toes or other shapes that are not the normal configuration of the foot
• Fitted generously—better to be too large than too small
• Friction similar to skin—the soles should have the same friction as skin so that they are not slippery
Care of Children in Casts and Splints
The child’s cast should be kept cool, clean, and dry. Cover the cast with plastic wrap or a plastic bag when the child bathes or is in a situation in which the cast may get wet. The only cast that can go in water is a Gore-Tex cast. If the cast becomes wet, a hair dryer set on cool setting can be used for drying small areas. If the cast becomes soiled it can be cleaned with a slightly damp washcloth and cleanser.
 Orthopedic Problems Specific to Children
Orthopedic Problems Specific to Children
Arm Problems
Brachial Plexus Injuries
Description
Brachial plexus injuries are typically classified using Narakas criteria types I through IV (Table 37-1). Brachial plexus injuries can also be classified as type I (Erb-Duchenne paralysis) with C5 through C6 involvement that includes the shoulder and upper arm; type II (Erb-Duchenne-Klumpke paralysis) involves the entire brachial plexus (i.e., C5 through T1 involvement) affecting the shoulder, arm, and hand; or type III (Klumpke paralysis) caused by injury to C8 through T1 with involvement of the lower arm and hand (Zafeirious and Psychogious, 2008).
TABLE 37-1 Brachial Plexus Injury Using Narakas Classification
| Name | Nerve and Muscle Involved | Prognosis |
|---|---|---|
| Narakas type I | C5 and C6; shoulder and biceps | Recovery usually complete |
| Narakas type II | C5-C7; shoulder, biceps, and forearm extensors | Recovery usually complete |
| Narakas type III | C5-T1 | Variable with complete paralysis of limb; shoulder and biceps recovery is fair to poor with hand recovery variable |
| Narakas type IV | C5-T1 | Complete paralysis of the limb and Horner syndrome; shoulder and biceps recovery is fair to poor with hand recovery variable |
Clinical Findings
History
History should include obstetric history, mode of delivery, and postnatal health of the infant.
Physical Examination
• Erb palsy, presenting with an adducted arm, which is internally rotated at the shoulder. The wrist is flexed, and the fingers extended, resulting in a characteristic “waiter’s tip” posture.
• Absent bicep reflex with absent Moro reflex on the affected side
• Limp wrist and hand with absent grasp reflex (lower plexus involvement)
• Horner syndrome (ipsilateral ptosis, miosis, enophthalmos, anhidrosis) if the sympathetic fibers of the T1 nerve root are involved
• Occasionally hand paralysis with normal shoulder movement, which is a rare occurrence of an isolated C8 through T1 injury
• Ruptured intraabdominal structures, especially the liver and spleen, which require careful abdominal examination
• Limited neck movement due to damage to the sternocleidomastoid muscle; skull fracture
• Impaired respiratory effort as a result of diaphragmatic paralysis and flaccidity
Differential Diagnosis
The differential diagnosis of upper extremity paralysis in a newborn includes epiphyseal separation of the humeral head, fracture of the clavicle or humerus, septic arthritis of the upper extremity, spinal cord injury, cervical cord lesions, and congenital varicella of the upper limb (Zafeirious and Psychogious, 2008).
Shoulder Problems
Clinical Findings
Physical Examination
In all children, look for the following:
Diagnostic Studies
Imaging studies are recommended. Radiography with routine clavicle views is sufficient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree