Introduction
The rate of multiple gestations in the United States is rising dramatically. This is of concern because multiple gestations contribute disproportionately to the incidence of perinatal morbidity and mortality. Fortunately, recent advances in perinatal medicine have resulted in improved overall outcomes in pregnancies complicated by multiple gestations.
The fetus develops within the amniotic sac, which consists of two fetal membranes called the chorion and the amnion. The outer layer, which is in closer proximity to the mother, is the chorion. A segment of the chorion contains the chorionic villi, which invade the uterine decidua to eventually form the placenta. The villi in the remaining chorion undergo atrophy, thus forming the smooth opaque outer layer of the fetal membranes. The inner layer of the fetal membranes is the translucent amnion. In the case of twins, dichorionic twins have entirely separate placentas and fetal membranes, while monochorionic twins share the same placenta.
Multiple gestations should be classified based on chorionicity (Figure 5.1). Chorionicity can be diagnosed in the first or early second trimester with over 95% accuracy by ultrasound evaluation of the dividing membranes’ insertion site. Dividing membranes are defined as the portion of the fetal membranes in which the two separate twin gestational sacs are in contact. All twins, except monochorionic monoamniotic twins, have dividing membranes. In the case of dichorionicity, the dividing membranes have intervening chorion, thereby forming a “twin peak” or “lambda” sign at the junction between the two placentas. In the case of monochorionic diamniotic twins, the dividing membrane is composed of only two abutting amnions. Thus, the dividing membranes of a monochorionic placenta are thin and insert perpendicularly into the placenta in the so-called “T” sign.
Figure 5.1 First trimester ultrasound of dichorionic twins (left) and monochorionic twins (right). The image on the left shows the “twin peak” sign (arrow), which is indicative of dichorionic twins. The image on the right shows a thin dividing membrane inserting into the common placenta, called a “T sign”, which is an ultrasound marker for monochorionic twins.
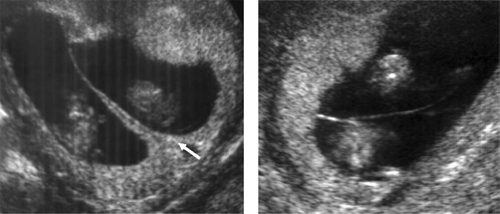
It is important that chorionicity be established as early in pregnancy as possible. Aside from gender discordance, which would confirm dichorionicity, all ultrasound markers of chorionicity become less accurate as the pregnancy progresses. Ultrasound views of the dividing membranes’ insertion site are hampered in the latter half of pregnancy. Also, the placentas in a dichorionic twin gestation often adjoin one another, appearing as one placental mass, in the late second and third trimester.
Clinical significance of monochorionicity
Monochorionic twins are associated with significant increased perinatal morbidity and mortality as compared to dichorionic twins and singletons. One factor associated with this increased risk is the presence of vascular communications in the shared placenta. The vascular communications are important in the development of twin–twin transfusion syndrome and twin reverse arterial perfusion sequence, both of which have high perinatal mortality rates. Also, because the circulatory systems of the twins are linked together by the vascular anastomoses, the death of one twin may lead to an immediate hypotensive episode in the live twin due to exsanguination into the dead twin. The acute hemodynamic instability may result in death or injury to the co-twin. Another placental factor that contributes to the disproportionate rate of perinatal complications in monochorionic twins is unequal partitioning of the single placental mass, which may manifest clinically as selective intrauterine growth restriction. Finally, the risk of structural or chromosomal anomalies is increased in monochorionic twins. Anomalies of the central nervous system, heart, gastrointestinal tract and anterior abdominal wall occur at a higher rate in monochorionic twins as compared to dichorionic twins and singletons. Despite being monozygotic, the rate of discordance in anomalies between monochorionic twins may reach 80%, meaning that only one “identical” twin may have a structural abnormality.
A zygote is a cell that results from fertilization of an ovum and a sperm. Dizygotic twins result from fertilization of two separate ova by two separate sperm. The twins are genetically distinct, with as much commonality as ordinary siblings. The two zygotes each develop their own placentas and surrounding membranes, resulting in dichorionic diamniotic twins.
Monozygotic twinning results from a “split” of a single zygote into two or more embryos. The etiology of this division is unknown, although some view it as an anomalous embryonic event. The timing of the division determines both the chorionicity and amnionicity. Division within 3 days of fertilization results in the development of a dichorionic diamniotic twin gestation because the division occurred prior to the differentiation of the chorion. Approximately 30% of monozygotic twins are dichorionic diamniotic. If the division occurs between days 4 and 8 after fertilization, monochorionic diamniotic twin gestation develops. In this case, the twinning happens after differentiation of the chorion but before differentiation of the amnion. Monochorionic diamniotic twins make up almost 70% of monozygotic twins. A monochorionic monoamniotic twin gestation results from division after day 9 from fertilization, after the differentiation of the amnion; this occurs in about 1% of monozygotic twins. Incomplete embryonic division occurs after day 13, resulting in the rare condition of conjoined twins. Although monozygotic twins typically have an identical genetic make-up, genetic and/or phenotypic discordance can arise due to postzygotic perturbations.
Zygosity testing is feasible during pregnancy. One method is via DNA testing of amniocytes (fetal cells suspended in amniotic fluid) using PCR to identify discordance between variable number tandem repeats and other polymorphisms. However, aside from rare uses in prenatal diagnosis of genetic diseases, zygosity testing is not often utilized during pregnancy. As already mentioned, it is primarily the chorionicity, not zygosity, which determines the risks of the pregnancy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


