■ HYPOKINETIC MOVEMENT DISORDERS
Parkinsonism
Parkinsonism is the most common hypokinetic disorder. It is usually characterized by two or more of the usual parkinsonism signs: (1) rest tremor at 4 to 6 Hz that may also occur with sustained posture, (2) bradykinesia (slowness of movement) or more rarely akinesia, (3) rigidity in which muscle tone is increased in all directions of movement and which is not altered by movement velocity, and (4) postural instability in which dysregulation of postural reflexes may lead to retropulsion (multiple steps backward) when the patient is pulled backward (pull test). There are multiple causes of insidious onset parkinsonism. Parkinson’s disease is common in adults and is a primary type of parkinsonism. Juvenile Parkinson’s disease is rare, and it often presents with dystonia, rigidity, and bradykinesia without the classic rest tremor seen in adults (2,3). In children, parkinsonism is often secondary to other neurologic problems, and often presents along with other symptoms and signs (4).
A child presenting with parkinsonism that started in the preceding few days or weeks and is already pronounced is unlikely to have a degenerative disease and urgent evaluation for acute or subacute illness causing secondary parkinsonism is indicated. There will often be clinical clues to the underlying diagnosis provided by the constellation of symptoms and signs. Subdural hematoma and hypothyroidism may mimic parkinsonism.
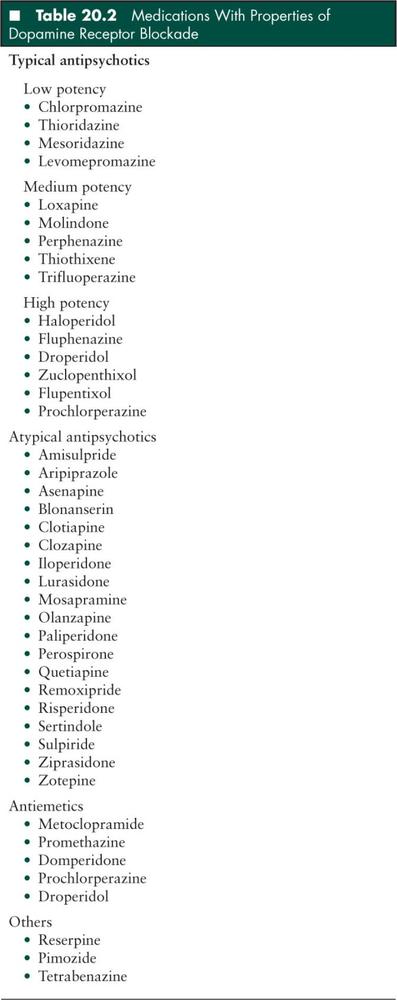
Drug-induced disease is most commonly caused by antiemetic medications including metoclopramide and neuroleptic medications (Table 20.2), but may also occur with amiodarone, calcium channel blockers, isoniazid, divalproex, and chemotherapeutic agents. In some cases, chemotherapy-induced parkinsonism is responsive to levodopa (5). Parkinsonism may occur as a delayed complication after bone marrow transplant in patients on chemotherapy (6).
Parkinsonism can be secondary to acute structural lesions such as stroke and tumor of the frontal lobes, substantia nigra, or thalamus (7–10). Parkinsonism may occur with hydrocephalus including due to ventriculoperitoneal shunt malfunction (8,11) and may also occur after shunt placement or third ventriculostomy procedures (12–14). Acute parkinsonism has been described following global hypoxemic injury (15–17). Demyelinating disorders including acute disseminated encephalomyelitis may cause parkinsonism (18). Subdural hematoma may present with parkinsonism (19).
Acute parkinsonism can also be a feature of toxic exposures. Carbon monoxide poisoning frequently causes necrosis of the globus pallidus. After recovery from the initial insult and coma, a phenomenon called delayed demyelination can result in profound, rapidly developing parkinsonism (20–22). Pallidal necrosis can also occur as a rare late complication of wasp stings (23). Acute parkinsonism was seen in a mini-epidemic of drug users who took the synthetic opiod desmethylprodine MPPP or 1-methyl-4-phenylproprionoxypiperidine, an analog of meperidine that was contaminated with MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) (24).
Mycoplasma pneumoniae (25) and streptococcal pharyngitis (26) infections has been associated with parkinsonism. Similarly, many viral encephalitides can cause an acute parkinsonian syndrome: Epstein-Barr virus (EBV) (27), influenza (including H1N1) (28), coxsackie, measles, polio, St Louis encephalitis, and Western equine encephalitis. In HIV disease, acute parkinsonism can be seen with opportunistic infections including toxoplasmosis, Cryptococcus, progressive multifocal leukoencephalopathy, and tuberculosis. It can also be seen with the HIV associated encephalopathy spectrum (29,30). As a historical note, in the early 20th century, von Economo described encephalitis lethargic, a disorder in which various acute forms including stupor or coma, hyperkinetic chorea and athetosis, or parkinsonism would often lead to death, and among survivors a postencephalitic parkinsonism would develop 5 to 10 years later (31–33). Recent cases have also been described (34).
Huntington’s disease usually appears in adults and includes choreoathetosis and dementia. However, the Westphal variant occurs in childhood and includes bradykinesia, rigidity, seizures, and decline in mentation. This disorder is not acute in onset, but it can be more rapidly progressive than in adults and rarely presents in an urgent setting, eventually being diagnosed after secondary etiologies are ruled out.
Catatonia
Catatonia is characterized by extreme slowness of movement and altered responsiveness sometimes to the point of a stuporlike state. There may be catalepsy, in which the patient maintains unusual postures for prolonged periods of time, and “waxy flexibility,” in which the patient maintains postures set by the examiner. Generally no structural disease is found and catatonia usually occurs in the setting of serious psychiatric disease, although it may also occur in the context of various neurodevelopmental and autoimmune disorders including childhood disintegrative disorder, Kleine-Levin syndrome, Prader-Willi syndrome, tic disorders, and autoimmune encephalitis (35,36). Malignant catatonia can mimic neuroleptic malignant syndrome and is discussed in other chapters (Hyperthermic Drug Induced Disorders and Neurotoxicology).
■ HYPERKINETIC MOVEMENT DISORDERS
Classifying a hyperkinetic movement disorder is challenging since there are many types. The initial assessment of these patients should distinguish between movements which are involuntary, abnormal, and excessive and other movements which may appear abnormal but are actually purposeful (such as guarding muscle contractions in the setting of pain). Once the movements are determined to be involuntary, they can be classified through careful observation, as discussed below.
Dystonia
Introduction
Dystonia is an involuntary abnormal posture of a limb or the torso. It is sometimes accompanied by twisting or repetitive movements or these movements may occur in isolation. Dystonia is caused by disease of the basal ganglia and is the result of abnormal persistent muscular contraction. An example is torticollis, where the head is persistently turned and tilted to one side or slow repetitive movements to the side or a combination of the two. Focal dystonia may occur at other locations along the torso, at a limb, the face, and the larynx. It can be widespread along the torso and all limbs. Some patients obtain temporary relief from sensory stimuli, as when the patient with torticollis has some neck relaxation in response to light touch to the face. Dystonia can resolve in sleep. Many of these conditions are hereditary, slow in onset, and progressive. This section focuses on acute dystonia requiring urgent assessment.
Acute Dystonic Reactions to Medications
Acute dystonic reactions to neuroleptics (Table 20.2) affect 2% to 3% of patients soon after initiation of dopamine receptor antagonist therapy (37), often within 1 to 5 days of starting therapy. Younger patients and males tend to be more susceptible, and the incidence of an acute dystonic reaction increases to almost 50% with high potency neuroleptic treatment (38,39). While dystonia can be one of the earliest side effects of dopamine receptor blockade, it can also be seen in the setting of chronic neuroleptic use, constituting tardive dystonia, where the incidence may be as high as 10% (40). It is often referred to as a toxic effect but can occur even with standard therapeutic doses. Other medications that occasionally cause dystonia include phenytoin, carbamazepine, levodopa, calcium channel blockers, and cetirizine. In addition to acute isolated dystonia, drug-induced neuroleptic malignant syndrome can include dystonia.
Acute dystonic reactions typically involve the muscles of the eyes, face, mouth, tongue, jaw, and neck. Less frequently the trunk and limbs are involved. For example, an acute prominent torticollis may appear. The sustained muscle contractions can be painful and severe. Cervical, oral, or laryngeal dystonia can be life-threatening if they affect respiration or result in dysphagia with aspiration. Oculogyric crisis is an acute dystonia that commonly includes forced eye deviation, jaw opening, tongue protrusion, and arching of the neck and/or trunk (41). Acute dystonic reactions have been associated with stridor, presumably due to dystonic involvement of the larynx or pharynx (42). In one patient acute dystonia led to self amputation of the tongue (43).
Treatment of acute dystonic reactions involves administration of oral, intramuscular, or intravenous anticholinergics or antihistamines such as benztropine or diphenhydramine (44). Intravenous diazepam has also been used as an effective alternative therapy (45). Even untreated, most acute dystonic reaction will resolve spontaneously within 12 to 48 hours after the last exposure to dopamine receptor antagonist. However, these reactions are often painful for the patient and potentially dangerous, so treatment is a consideration depending on the severity of the condition. Recurrence may occur, so often continued administration of an oral anticholinergic medication for 5 to 7 days or more is indicated.
Acute Dystonia—Other Etiologies
New structural disease in the basal ganglia and acute withdrawal of medications including intrathecal baclofen, tetrabenazine, and lithium may produce acute dystonia (46,47). Dystonia may occur in bacterial, viral, and fungal meningoencephalitis, including HIV, tuberculosis (TB), and celiac disease. Dystonia occurs in Wilson’s disease, vitamin E deficiency, and autoimmune diseases. Organic acidemias may not present until a time of metabolic stress and then present with severe and rapid onset dystonia. Toxic disturbances caused by carbon monoxide, ethylene glycol, methanol, cyanide, stimulants such as amphetamines, and wasp stings may all involve dystonia. Dystonia can be psychogenic and occur as a component of a conversion disorder.
Initial management is with anticholinergics, benzodiazepines, dopamine receptor blockers. Rarely general anesthesia and paralysis are required as a temporizing measure. Management is mostly supportive and involves sedation, antipyretics, pain management, management of rhabdomyolysis, and appropriate cardiopulmonary support. In more refractory cases, particularly in patients with idiopathic torsion dystonia, management options include intrathecal baclofen or surgical interventions such as thalamotomy, pallidotomy, and deep brain stimulation (48).
There is a group of hereditary and acquired kinesigenic (provoked by movement especially exercise) and nonkinesigenic paroxysmal movement disorders that include dystonia or choreoathetosis and occur in children and adults. Episodes last from minutes to a few hours. Depending on the particular condition, there may be a response to antiepileptic drugs or benzodiazepines (49).
Status dystonicus (dystonic storm) is a rapidly developing and severe hyperkinetic movement disorder involving dystonia and chorea. It may occur in children with pre-existing dystonia, such as primary dystonia or dystonic cerebral palsy, who miss medications, undergo medication adjustments, or develop intercurrent infections. The condition is painful and may cause rhabdomyolysis or respiratory compromise. Treatment is difficult, and dystonic storm may persist for several months and recur with future infections. Trihexphenidyl and tetrabenazine may be tried, and anesthesia with paralysis is sometimes needed as a temporizing measure.
Pseudodystonia mimics dystonia. Atlantoaxial subluxation can cause pseudotorticollis (head tilt, contralateral neck rotation, and neck flexion), particularly in children with trisomy 21 or following head/neck trauma. The patient may not be able to rotate the head past midline. Neck muscles are found to be relaxed on palpation, as opposed to the usual hyperactive state noted in dystonia (50). Other structural disease in the posterior fossa or cervical spine and also diseases of the soft tissues of the neck (for example, pharyngitis, tonsillitis, mastoiditis) may simulate dystonia. Tetanus can mimic dystonia and delayed diagnosis can be potentially disastrous. In a patient who is unimmunized or underimmunized, it can present as focal spasm usually close to the site of injury. Trismus and other cephalic forms of tetanus may resemble oculogyric crisis. Focal tetanus of a limb may resemble a focal dystonia. The disorder is generally progressive, and a high degree of suspicion must exist. Treatment is with immunoglobulin and antibiotics (51). Other disorders that can produce pseudotorticollis are neoplastic or infectious processes of the head, neck, or spinal cord (52–54). Trochlear nerve palsy often results in head tilt. Sandifer syndrome is a childhood condition of dystonia associated with gastrointestinal reflux.
Chorea, Athetosis, and Ballismus
These are presented as a group because it is useful to compare the movements and etiologies, and because classification may be difficult with overlapping movements in a patient. Choreic movements are typically brief, rapid, small to moderate size movements that occur randomly at the limbs, torso, and face. The movements are involuntary, nonrhythmic, and direction-changing. The patient may try to mask a choreic movement by adding on a voluntary purposeful movement as the choreic movement ends, referred to as parakinesias. Athetosis is slower, more writhing, and continuous compared to chorea. Ballismus refers to large, brief, rapid, flinging irregularly timed movements at the shoulder or hip joint. It is often unilateral (hemiballismus). In some patients it is difficult to classify the movements in one of the three categories. Choreoathetoid movements have mixed characteristics. Chorea and athetosis and occasionally ballismus may be seen in the same patient, and they have a similar differential diagnosis.
Chorea and its related movements may occur with toxic, metabolic, vascular, infectious, postinfectious, and endocrine etiologies. Sydenham chorea is related to an autoimmune poststreptococcal process (see below). Focal lesions in the basal ganglia, including infarction, hemorrhage, tumor, and demyelination may produce acute onset or progressive chorea. Vascular etiologies include stroke, moyamoya disease, and vasculitis. Both hyperglycemia and hypoglycemia can present with chorea. Common systemic etiologies for chorea are the antiphospholipid antibody syndrome and systemic lupus erythematosus, both of which may present with neuropsychiatric symptoms including a variety of movement disorders often including chorea (55–59). Other systemic etiologies are hyperthyroidism, pheochromocytoma, Henoch-Schönlein purpura, and neuroacanthocytosis. Infections including Lyme disease, HIV, and mycoplasma may involve chorea. Medications that can cause these movements include anticholinergics, phenytoin, carbamazepine, stimulants including amphetamines and methylphenidate, tricyclic antidepressants, clonidine, L-dopa, lithium, and oral contraceptives. Toxins which may produce chorea include manganese, ethanol, toluene, and carbon monoxide. Neuroleptics sometimes cause chorea. Chorea may follow cardiac bypass (post-pump chorea) and may be transient or persistent. Chorea gravidarum usually occurs during the first or early second trimester and generally resolves later in the pregnancy or after delivery. Primary causes of nonacute chorea are unlikely to present for urgent care and include Huntington’s disease and ataxia-telangiectasia.
Sydenham chorea should be considered in every child with chorea (60). It is the neurologic manifestation of rheumatic fever, as diagnosed by the Jones Criteria for Rheumatic Disease. It presents with a 1- to 8-month delay after group A beta hemolytic streptococcal infection. Onset is often over hours to days, and many families can identify the exact date of onset. Diagnosis of Sydenham chorea requires evidence of a prior clinical streptococcal infection or elevated antistreptolysin O or anti–DNase-B antibody titers as markers of prior infection. The typical age of presentation is 5 to 15 years, and there is a female preponderance. Brain magnetic resonance imaging (MRI) is typically normal but there are reports of reversible basal ganglia hyperintensities (61). There are often other psychiatric comorbidities seen, such as personality changes, attention deficit disorder, and obsessive compulsive features. It is critical to evaluate for the other rheumatic disease features including the systolic murmur characteristic of cardiac disease which generally prompts echocardiographic evaluation. Treatment goals are prevention of recurrence of rheumatic fever and management of the chorea. Antibiotics are used to prevent recurrence of rheumatic fever and may include several years of monthly injections of penicillin G, daily penicillin, or daily sulfadiazine. There are differences of opinion regarding treatment of the chorea. Benzodiazepines and valproic acid is sometimes helpful. Neuroleptics have also been used, but typically are used sparingly to avoid tardive abnormal movements (62,63). Depending on the severity of the chorea, immunomodulatory therapy with prednisone and more rarely intravenous immunoglobulin or plasmapheresis can be considered (64,65).
Hemiballismus may occur with stroke or other focal lesions in or near the subthalamic nucleus and with nonketotic hyperglycemia.
Myoclonus
Myoclonus is characterized by rapid, shocklike, involuntary, and irregularly timed movements of a limb, segment of the body, or large part of the body. The movements are much more rapid than in chorea. It may be physiologic as in sleep myoclonus, hereditary, part of a progressive degenerative condition, or secondary to other disease. It may be epileptic, cortical but not epileptic, or arise from disease of subcortical structures, the brainstem, or the spinal cord.
Myoclonus is a common component of neurodegenerative disorders including the progressive myoclonic epilepsies, in which case myoclonus occurs in the context of encephalopathy and other neurodevelopmental abnormalities, and does not present acutely. Additionally, myoclonic seizures are a common component of many epilepsy syndromes including juvenile myoclonic epilepsy, myoclonia with childhood absences, and Lennox-Gastaut syndrome. Rarely myoclonus can occur within the spectrum or jerking movements associated with epilepsia partialis continua.
Acute onset myoclonus or symptomatic myoclonus generally occurs in the context of encephalopathy and other neurologic problems (66). It may occur after severe brain injury, most commonly following hypoxic-ischemic brain injury. When myoclonic status epilepticus occurs after hypoxic ischemic encephalopathy, it suggests an unfavorable prognosis. However, nonepileptic myoclonus may occur after cardiac arrest and may be associated with favorable outcome (Lance-Adams syndrome) (67,68). Myoclonus may occur with stroke or tumor, infectious meningoencephalitis (including bacterial, arboviruses, herpes virus, EBV, Lyme disease, hepatitis, HIV, fungal) (69–71), autoimmune processes such as acute disseminated encephalomyelitis, hepatic and uremic encephalopathy, celiac disease, hypocalceima, hypomagnesemia, hypothyroidism, hyperglycemia, hypoglycemia, hyperthyroidism, vitamin E deficiency, and serotonin syndrome (discussed in the chapter on Hyperthermic Syndromes). It may be caused by medications including monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, opiates, levodopa, triptans, some antibiotics (penicillin, cephalosporins, quinolones), and by illicit drugs including lysergic acid diethylamide, amphetamines, cocaine, and 3,4-methylenedioxymethamphetamine (ecstasy). Myoclonus may be caused by intoxication with lead, carbon monoxide, mercury, and bismuth. Wilson’s disease should be considered. Psychogenic myoclonus occurs. A variety of epilepsy syndromes involve myoclonic seizures, and rarely some anticonvulsants (lamotrigine, carbamazepine, phenytoin, gabapentin, and vigabatrin) can worsen myoclonic seizures.
Myoclonus may occur as a component of opsoclonus-myoclonus syndrome. This syndrome may present with myoclonus that is diffuse, multifocal, and low amplitude. Opsoclonus, often considered the hallmark of the syndrome, may be intermittent, late occurring, or subtle, and this may not be readily apparent. Onset is often in children younger than 5 years of age. Consideration and evaluation is essential since it may be associated with neuroblastoma. Testing for urine catecholamines and a complete and often repeated evaluation for neuroblastoma is indicated. As described above, opsoclonus-myoclonus may also occur in the context of many infections and celiac disease.
Clonazepam, valproic acid, and levetiracetam are sometimes helpful for management, especially if the myoclonus is cortical, but their use is off label.
Tremor
Tremor is a rhythmic rapid oscillating movement at a fixed point caused by alternate contractions of antagonist muscles. It can be seen at rest (as in parkinsonism) or while maintaining a sustained posture (action tremor). Tremor can be divided into three broad categories. First, enhanced physiologic tremor refers to tremor which becomes enhanced or first visible in certain situations including emotional stress, fatigue, or stimulating medications/substances (such as caffeine, amphetamines, or thyroid hormones). Second, essential tremor which refers to a primary tremor that is often suppressed by alcohol. Third, symptomatic tremor in which tremor generally occurs in the context of other symptoms and signs.
Symptomatic tremor is generally caused by disorders affecting the corticostriatopallidothalamic or cerebellar-thalamic circuits, and this involves generally subcortical and posterior fossa disorders. Lesions may include cerebellar malformations and cysts (72–74), neoplasms, stroke, and demyelinating disease. Rubral tremor may arise with lesions of the red nucleus. Systemic causes of symptomatic tremor include endocrine disorders [hyperthyroidism (75), hyperadrenalism], low magnesium, and hepatic encephalopathy. Drug-induced parkinsonism can include tremor. Other drugs that can cause tremor include tricyclic antidepressants, selective serotonin re-uptake inhibitors (SSRI) medications, lithium, amiodarone, cyclosporine, divalproex, and some antiviral medications. Exposure to heavy metals such as lead or mercury as well as toxicity from recreational “sniffing” or inhalation of volatile vapors can cause tremor. Acute onset tremor can occur with Wilson’s disease.
Tic Disorders
Tic disorders are seldom movement disorder emergencies, but they are important to recognize and distinguish from other movement disorders. They are involuntary, brief, rapid, and often stereotyped movements or vocalizations performed in response to an internal urge. Tics differ from other movement disorders in that they can often be suppressed completely for a period of time. Simple tics that involve a sudden movement of a limb can often be confused with myoclonus, and the history of being suppressible is an important distinguishing factor. Tics can also involve a complex series of movements.
Ataxia
Ataxia is not typically classified as a movement disorder but is included here since it does involve abnormal movement and must be distinguished from other abnormal movements. Ataxia is usually due to disease of the cerebellum or tracts connecting the cerebellum to other structures. Ataxic movements are inaccurate volitional movements with incoordination of the multiple muscle contractions and multiple joint rotations that normally are carried out such that the terminal point of the limb is guided directly and smoothly to a target. Symptoms and signs are dysmetria, gait unsteadiness with a wide base, dysarthria, and titubation. Dysmetria, also called intention tremor, can be seen as inaccuracy, with repeated undershooting and/or overshooting of corrective movements, as the hand or foot approaches a target, often demonstrated with the “finger-nose” and “heal-shin” tests. Titubation is wavering movement of the trunk.
Primary ataxia is often genetic, including the spinocerebellar ataxias, ataxia-telangiectasia, and Friedreich ataxia. Secondary ataxias usually require urgent care. The most common etiologies of acute onset ataxia are ataxia due to intoxication or ataxia associated with a viral illnesses. Ataxia associated with intoxication may occur with exposure to alcohol, anticonvulsants, antihistamines, and benzodiazepines. Ataxia may occur after a variety of clinical and subclinical infections and generally presents with gait ataxia, and less commonly with truncal ataxia or nystagmus. Onset may be abrupt or slowly evolving. These are likely caused by autoimmune molecular mimicry between the cerebellum and viral proteins. MRI may demonstrate enhancement in the cerebellum consistent with a cerebellitis, and cerebrospinal fluid may show pleocytosis. Acute ataxia generally resolves, but this may take many months.
Other causes of acute ataxia include encephalitis, ataxic cerebral palsy, metabolic disorders (congenital disorders of glycosylation, mitochondrial disorders, urea cycle disorders, Refsum’s disease, Hartnup’s disease), vitamin E deficiency, and opsoclonus-myoclonus syndrome (which can also present with ataxia in the absence of opsoclonus or myoclonus), Wilson’s disease, thiamine deficiency, Miller Fischer variant of Guillain-Barré disease, and hypothyroidism. Acute focal cerebellar lesions, for example due to stroke, tumor, and demyelination, may also present with acute ataxia, and neuroimaging is often indicated. These often present along with posterior fossa signs such as headache, emesis, and cranial nerve palsies, but may occur with just ataxia initially. Functional ataxia as a component of conversion disorder must also be considered.
Acute Torticollis
Acute torticollis may occur in children with processes involving the posterior fossa and cervical spine including tumors, hemorrhages, and infection. Acute infectious torticollis may occur after pharyngitis, tonsillitis, mastoiditis, or other infections involving the head or neck. Patients have a painful, fixed torticollis. Prompt recognition is required so specific therapy can be instituted. Management involves neuroimaging of the brain and cervical spine, infection evaluation of the head and neck structures as well as brain, and then specific therapy.
Bobble-Head Doll Syndrome
Persistent or episodic side-to-side or forward-and-back head movements like a bobble head doll can be seen in infants and children. These movements are often seen with third ventricular lesions and include third ventricular cysts, tumors, and aqueductal stenosis (76–78) and may occur with shunt malfunction (79). Neuroimaging is required.
Wilson’s Disease
Wilson’s Disease is often diagnosed when a movement disorder and neuropsychiatric symptoms appear. Usually liver disease is also present by that time. It requires a high degree of clinical suspicion and accurate tests are available. Treatment can alter the patient’s outcome, particularly if initiated early. It is an autosomal recessive disorder characterized by copper accumulation. Clinically, there is elevated urinary copper excretion and low serum ceruloplasmin. Copper deposition is seen on liver biopsy. Ophthalmologic slit lamp exam reveals Kayser-Fleischer rings. The initial presentation is often subtle but progressive decline in cognitive and school performance, and behavioral changes are common. It is the movement disorder that often leads to medical attention. The abnormal movements are highly variable, involving tremor, bradykinesia, dystonia, dysarthria, dysphagia, incoordination, chorea, and athetosis (80). Tremor can be present at rest but often is much more prominent and proximal when the arms are held outstretched (wing beating tremor). There can be persistent grinning appearance (risus sardonicus), caused by dystonic facial muscles. Copper chelation therapy with penicillamine or trientine is standard, although both of these medications can make a patient’s neurologic symptoms temporarily or persistently worse (81). Recently, penicillamine has fallen out of favor due to the side effect profile, and trientine is more widely used. Intestinal copper absorption may be reduced with zinc or tetrathiomolybdate (82,83).
Paraneoplastic Disorders With Prominent Movement Aspects
A brief review of the paraneoplastic disorders is presented here because these patients often present acutely. The presentation can be varied, so the clinician needs to have a high clinical suspicion for these disorders. In recent years anti-NMDA receptor antibody mediated encephalitis has been more widely recognized. In adults, this disorder was initially described in young women with ovarian teratomas (84), and recently it has been described in children with and without neoplasms (85). In children, the disorder should be suspected in patients who present with behavioral changes, abnormal movements, and seizures. These patients can have a nonspecifically abnormal electroencephalogram, a frequently mild CSF (cerebro-spinal fluid) lymphocytic pleocytosis, and typically a normal MRI, so diagnosis must be driven by clinical suspicion. Evaluation for tumors is essential, although none are identified in many children. Management may involve tumor removal, immunomodulation with corticosteroids and immunoglobulins, and, in more severe cases, cyclophosphamide and rituximab (62).
Opsoclonus myoclonus ataxia syndrome is another rare disorder that presents in children. This syndrome most commonly is associated with neuroblastoma, can be seen in up to 3% of patients with neuroblastoma, and may be the presenting sign (86). Rarely, it can precede the appearance of a tumor by up to 4 years. In some cases a tumor is never found and the disorder is hypothesized to be a parainfectious autoimmune process. Within the name of the diagnosis are the three cardinal features. Opsoclonus describes random, multidirectional, often “bouncing,” conjugate eye movements. Myoclonus is often in the face and neck. Ataxia in these patients is often truncal and appendicular. Not all features need to be present, and some may be intermittent, lacking at presentation, or subtle. Treatment involves identifying and treating the neuroblastoma and immunomodulation for the symptoms of the disorder. Immunomodulation may include immunoglobulin and corticosteroids, as well as more aggressive therapies such as cyclophosphamide and rituximab (87).
Psychogenic Movement Disorders
Psychogenic movement disorders are common in children (1). These may have abrupt onset with severely abnormal looking movements, and thus may present to the acute setting. Identification is essential to avoid unnecessary testing and to rapidly initiate appropriate management. These are considered within the spectrum of conversion disorder, in which symptoms affecting motor or sensory function suggesting a neurologic cause are actually caused by psychological factors. Importantly, psychogenic movement disorders and organic disorders can coexist. Psychogenic movement disorders occur in about 2% to 5% of children with movement disorders (88–91). A review of 14 children with psychogenic movement disorders found that 29% presented with two or more movement disorders and 80% presented with unexplained symptoms in addition to the movement disorder. The most common movement disorders were tremor and dystonia (91). Although young children may present with psychogenic movement disorders, most children are aged 7 to 18 years (88–90). In general, outcome is favorable. Many resolve within several months, and most children achieve complete remission (92–94). Many children present with other psychiatric comorbidities including anxiety and mood disorders, and in about half of children a specific stressor can be identified. Involvement of psychologists, psychiatrists, and sometimes rehabilitation programs is essential.
■ CONCLUSIONS
Acute movement disorders are uncommon but they signal serious underlying disorders requiring rapid diagnosis and management. Careful observation and description of the movement abnormality (see Table 20.1) is important since identifying the specific movement abnormality will aid in differential diagnosis. A detailed history including focus on medication and toxic exposures is important, and brain MRI to search for an acute focal lesion is often indicated. For many of the conditions, outcome will be improved with early recognition and intervention.
■ REFERENCES
1. et al. A prospective study of acute movement disorders in children. Dev Med Child Neurol. 2010;52:739–748.
2. , , . Diagnostic considerations in juvenile parkinsonism. Mov Disord. 2004;19:123–135.
3. , . Juvenile parkinsonism. Semin Pediatr Neurol. 2003;10:62–67.
4. et al. Clinical spectrum of secondary parkinsonism in childhood: a reversible disorder. Pediatr Neurol. 1994;10:131–140.
5. et al. Chemotherapy-induced parkinsonism responsive to levodopa: an underrecognized entity. Mov Disord. 2003;18:328–331.
6. , , . Acute parkinsonian syndrome with demyelinating leukoencephalopathy in bone marrow transplant recipients. Pediatr Neurol. 1991;7:457–463.
7. et al. Simple and complex movements in a patient with infarction of the right supplementary motor area. Mov Disord. 1986;1:255–266.
8. , . Parkinsonian syndromes associated with hydrocephalus: case reports, a review of the literature, and pathophysiological hypotheses. Mov Disord. 1994;9:508–520.
9. . Delayed onset mixed involuntary movements after thalamic stroke: clinical, radiological and pathophysiological findings. Brain. 2001;124:299–309.
10. . Involuntary movements after anterior cerebral artery territory infarction. Stroke. 2001;32:258–261.
11. et al. Pathophysiology of parkinsonism due to hydrocephalus. J Neurol Neurosurg Psychiatry. 2004;75:1617–1619.
12. et al. Severe parkinsonism following endoscopic third ventriculostomy for non-communicating hydrocephalus—case report. Neurol Med Chir (Tokyo). 2011;51:60–63.
13. et al. Reversible parkinsonism following ventriculoperitoneal shunt in a patient with obstructive hydrocephalus secondary to intraventricular neurocysticercosis. Clin Neurol Neurosurg. 2008;110:718–721.
14. et al. Parkinsonism and midbrain dysfunction after shunt placement for obstructive hydrocephalus. J Clin Neurosci. 2006;13:373–378.
15. , . Hypoxic-ischemic damage of the basal ganglia. Case reports and a review of the literature. Mov Disord. 1990;5:219–224.
16. et al. Delayed parkinsonism associated with hypotension in a child undergoing open-heart surgery. Dev Med Child Neurol. 1993;35:1011–1014.
17. et al. Postanoxic parkinsonism: clinical, radiologic, and pathologic correlation. Neurology. 2000;55:591–593.
18. et al. Acute reversible parkinsonism in Epstein-Barr virus–related encephalitis lethargica–like illness. Mov Disord. 2006;21:564–566.
19. , , . Parkinsonism secondary to subdural haematoma. Neurosurg Rev. 2012;35(3):457–468.
20. . Carbon monoxide poisoning: systemic manifestations and complications. J Korean Med Sci. 2001;16:253–261.
21. . Parkinsonism after carbon monoxide poisoning. Eur Neurol. 2002;48:30–33.
22. et al. The brain lesion responsible for parkinsonism after carbon monoxide poisoning. Arch Neurol. 2000;57:1214–1218.
23. , , . Parkinsonism after a wasp sting. Mov Disord. 1999;14:122–127.
24. et al. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219:979–980.
25. , , . Reversible parkinsonism and dystonia following probable mycoplasma pneumoniae infection. Mov Disord. 1995;10:510–512.
26. , . Case report: severe acute parkinsonism associated with streptococcal infection and antibasal ganglia antibodies. Mov Disord. 2005;20:1661–1663.
27. et al. Reversible parkinsonian syndrome associated with anti-neuronal antibodies in acute EBV encephalitis: a case report. Parkinsonism Relat Disord. 2006;12:257–260.
28. et al. Hypothalamic abnormalities and parkinsonism associated with H1N1 influenza infection. J Neuroinflammation. 2010;7:47.
29. , , . Movement disorders and AIDS. Neurology. 1987;37:37–41.
30. , , . Parkinsonism with HIV infection. Mov Disord. 1998;13:684–689.
31. . Encepalitis lethargica. Weiner Klinische Wochenschrift. 1917;30:581–585.
32. . Encephalitis Lethargica, Its Sequelae and Treatment. Oxford University Press, London; 1931:I–XIV, 1–200.
33. , . Encephalitis and parkinsonism. Arch Neurol. 1965;12:227–239.
34. et al. Encephalitis lethargica syndrome: 20 new cases and evidence of basal ganglia autoimmunity. Brain. 2004;127:21–33.
35. , . Catatonia is hidden in plain sight among different pediatric disorders: a review article. Pediatr Neurol. 2010;43:307–315.
36. , . Update on anti–N-methyl-D-aspartate receptor encephalitis in children and adolescents. Curr Opin Pediatr. 2010;22:739–744.
37. . A survey of drug-induced extrapyramidal reactions. JAMA. 1961;175:1054–1060.
38. , , . Anticholinergic prophylaxis of acute haloperidol-induced acute dystonic reactions. J Clin Psychopharmacol. 1987;7:164–166.
39. et al. Acute accidental overdosage of haloperidol in children. Acta Paediatr. 1993;82:877–880.
40. , . Dyskinesia presenting as a respiratory emergency. Med J Aust. 1994;161:726–727.
41. , , . Acute dystonia induced by neuroleptic drugs. Psychopharmacology. 1986;88:403–419.
42. , . Acute laryngeal dystonic reactions to neuroleptics. Psychosomatics. 1989;30:359–364.
43. , . Auto-amputation of the tongue associated with flupenthixol induced extrapyramidal symptoms. Int Clin Psychopharmacol. 1999;14:129–131.
44. , . Severe extrapyramidal reaction to perphenazine treated with diphenhydramine. N Engl J Med. 1961;264:396–397.
45. , . Intravenous diazepam in drug-induced dystonic reactions. B J Psychiatry. 1972;121:75–77.
46. et al. Status dystonicus: the syndrome and its management. Brain. 1998;121 (pt 2):243–252.
47. , , . The treatment of severe dystonia in children and adults. J Neurol Neurosurg Psychiatry. 1984;47:1166–1173.
48. , . Review of the functional surgical treatment of dystonia. Eur J Neurol. 2001;8:389–399.
49. , . Paroxysmal dyskinesias: clinical features and classification. Ann Neurol. 1995;38:571–579.
50. et al. Current management of pediatric atlantoaxial rotatory subluxation. Spine. 1998;23:2174–2179.
51. , , . Cephalic tetanus: a case report and review of the literature. Am J Emerg Med. 1988;6:128–130.
52. , Moriarty RA. Atlantoaxial subluxation related to pharyngitis: Grisel’s syndrome. Clin Pediatr. 1999;38:673–675.
53. , . Inflammatory torticollis in children. Arch Otolaryngol Head Neck Surg. 1990;116:310–313.
54. et al. Torticollis as the presenting sign in cervical spine infection and tumor. Clin Pediatr. 1982;21:71–76.
55. et al. Long-term outcome of 32 patients with chorea and systemic lupus erythematosus or antiphospholipid antibodies. Mov Disord. 2011;26:2422–2427.
56. , , . Chorea as the presenting clinical feature of primary antiphospholipid syndrome in childhood. Neuropediatrics. 1999;30:96–98.
57. , , . Reversible chorea in primary antiphospholipid syndrome. Mov Disord. 1998;13:147–149.
58. , , . Pattern of neuropsychiatric manifestations and outcome in juvenile systemic lupus erythematosus. Clin Rheumatol. 2004;23:395–399.
59. et al. The incidence and prevalence of neuropsychiatric syndromes in pediatric onset systemic lupus erythematosus. J Rheumatol. 2002;29:1536–1542.
60. , , . Sydenham’s chorea: a practical overview of the current literature. Pediatr Neurol. 2010;43:1–6.
61. et al. Sydenham’s chorea: magnetic resonance imaging of the basal ganglia. Neurology. 1995;45:2199–2202.
62. et al. Comparison of the efficacy of carbamazepine, haloperidol and valproic acid in the treatment of children with Sydenham’s chorea: clinical follow-up of 18 patients. Arquivos de Neuro-Psiquiatria. 2002;60:374–377.
63. et al. Effectiveness of sodium valproate in the treatment of Sydenham’s chorea. Neurology. 1990;40:1140–1141.
64. et al. Treatment of Sydenham’s chorea with intravenous immunoglobulin, plasma exchange, or prednisone. J Child Neurol. 2005;20:424–429.
65. , , . Randomized double-blind study with prednisone in Sydenham’s chorea. Pediatr Neurol. 2006;34:264–269.
66. . Symptomatic myoclonus. Neurophysiol Clin. 2006;36:309–318.
67. , . Lance-Adams syndrome. Ann Rehabil Med. 2011;35:939–943.
68. , , . Myoclonus after cardiac arrest: pitfalls in diagnosis and prognosis. Anaesthesia. 2009;64:908–911.
69. , . Opsoclonus-myoclonus syndrome attributable to hepatitis C infection. Pediatr Neurol. 2010;42:441–442.
70. , Sinclair DB. Multifocal myoclonus following group A streptococcal infection. J Child Neurol. 2003;18:434–436.
71. , . Opsoclonus-myoclonus syndrome following Epstein-Barr virus infection. Neurology. 2002;58:1131–1132.
72. et al. Posterior fossa arachnoid cyst associated with an exertional tremor. Mov Disord. 2000;15:746–749.
73. et al. Resting tremor secondary to a pineal cyst: case report and review of the literature. Pediatr Neurosurg. 2008;44:234–238.
74. Colnat-Coulbois S, Marchal JC. Thalamic ependymal cyst presenting with tremor. Childs Nerv Syst. 2005;21:933–935.
75. et al. Surgical management of Graves disease in childhood and adolescence: an institutional experience. Surgery. 2006;140:1056–1061; discussion 61–62.
76. et al. Bobble-head doll syndrome associated with Dandy-Walker syndrome. Case report. J Neurosurg. 2007;107:248–250.
77. et al. Bobble head doll syndrome in a child with a third ventricular cyst and hydrocephalus. Childs Nerv Syst. 2005;21:350–354.
78. et al. Bobble-head doll syndrome: some atypical features with a new lesion and review of the literature. Acta Neurol Scand. 2003;108:216–220.
79. , , . Bobble-head doll syndrome associated with subduroperitoneal shunt malfunction. Childs Nerv Syst. 1997;13:234–237.
80. , . Wilson’s disease. Medicine. 1992;71:139–164.
81. . Treatment of Wilson’s disease with trientine (triethylene tetramine) dihydrochloride. Lancet. 1982;1:643–647.
82. et al. Treatment of Wilson’s disease with zinc: XV long-term follow-up studies. J Lab Clin Med. 1998;132:264–278.
83. et al. Treatment of Wilson’s disease with ammonium tetrathiomolybdate: III. Initial therapy in a total of 55 neurologically affected patients and follow-up with zinc therapy. Arch Neurol. 2003;60:379–385.
84. et al. Paraneoplastic anti–N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25–36.
85. et al. Anti–N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66:11–18.
86. et al. Opsoclonus-myoclonus-ataxia syndrome in neuroblastoma: clinical outcome and antineuronal antibodies—a report from the Children’s Cancer Group Study. Med Pediatr Oncol. 2001;36:612–622.
87. . Update on diagnosis, treatment, and prognosis in opsoclonus-myoclonus-ataxia syndrome. Curr Opin Pediatr. 2010;22:745–750.
88. Ferrara J, Jankovic J. Psychogenic movement disorders in children. Mov Disord. 2008;23:1875–1881.
89. Schwingenschuh P et al. Psychogenic movement disorders in children: a report of 15 cases and a review of the literature. Mov Disord. 2008;23:1882–1888.
90. Fernandez-Alvarez E. Movement disorders of functional origin (psychogenic) in children. Rev Neurol. 2005;40(suppl 1):S75–S77.
91. et al. Phenomenology of psychogenic movement disorders in children. Mov Disord. 2012;27(9):1153–1157.
92. , , . Somatoform disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:1329–1338.
93. . Treatment outcome for children and adolescents with conversion disorder. Can J Psychiatry. 1990;35:585–589.
94. , , . Clinical features of conversion disorder. Arch Dis Child. 1988;63:408–414.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


