Figure 8.1 Schematic of depth and area of transection in laparoscopic Kasai procedure. The aim is to achieve a shallow transection within the bifurcation of the portal vein.
Figure 8.2 (a and b) Extracorporeal Roux loop. The jejunojejunostomy (arrowheads) is placed just below the umbilicus, and the distal end (E) of the limb is brought up to the xiphoid process. The customised Roux limb is then approximated to the native jejunum for about 6 cm cranially (arrows) to streamline flow into the distal jejunum, eliminate reflux and prevent stasis in the Roux limb.
Table 8.1 The Juntendo University Hospital postoperative protocol
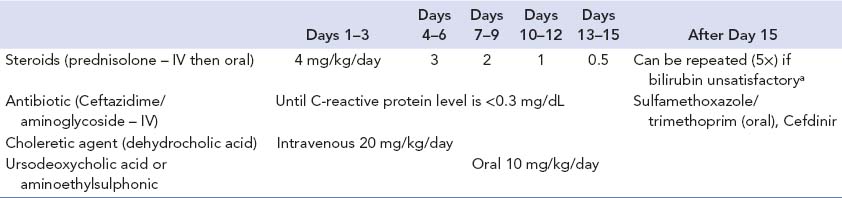
a Repetition is dictated by stool colour reverting to pale or white. If no clear response, then a maximum of five courses can be given and then should be considered for transplant.
A number of reasons have been suggested for the apparent disparity between the reported results of the LapKas and the standard open alternative.
The procedure is certainly technically demanding and probably unable to replicate the usual extended dissection of the porta hepatis. However, we believe that limited dissection, aiming to replicate Kasai’s original transection level, actually provides better results (Figure 8.1). We have accepted this, and indeed now make it a point of principle. Portal vein branches are ligated in the open Kasai, but monopolar hook cautery was used to coagulate and divide these laparoscopically, which may damage bile ductules [11]. The CO2 pneumoperitoneum may temporarily alter liver metabolism and function of various cells, including hepatic macrophages. This may be relevant in infants with BA [12–15].
Laparoscopic excision and reconstruction is becoming increasingly accepted as a valid and safe treatment in children with CCM.
The technique was first reported by an Italian team in 1995 [16] in a 6-year-old girl. They used an Endo GIA stapling device to divide the biliary tract, and a hepaticojejunostomy (HJ) was performed using interrupted 4/0 catgut sutures. Other case reports and small series followed, with the most recent huge series of well over 100 cases being reported from both China [17,18] and Vietnam [19] (Box 8.2).
Patient positioning
• Infant is positioned at the foot of the operating table. Surgeon works at the infant’s feet with the camera assistant on the infant’s right, and a working assistant on the left.
Port positioning (Figure 8.3)
• Supraumbilical (open Hasson* technique) 10 mm trocar for 30° or 45°, 5 or 10 mm laparoscopes.
• 5 mm trocars (3×) (Figure 8.1a) inserted in the right upper quadrant, left paraumbilical area and left upper quadrant. Maintain intra-abdominal pressure at 8–12 mmHg using a CO2 flow of 0.5–1.5 L/min.
Initial dissection of choledochal malformation
• Elevate and retract the liver.
• Percutaneous stay suture placed just below the xiphoid process to snare the umbilical ligament.
• Expose the porta hepatis by grasping the fundus of the gallbladder with Babcock forceps inserted through the left subcostal port in the anterior axillary line.
Intraoperative cholangiography
• Performed with a catheter inserted into the cystic duct. This may be unnecessary if the preoperative magnetic resonance cholangiopancreatography delineates appropriate anatomy of the proximal ducts and the pancreaticobiliary junction.
Figure 8.3 (a and b) Port sites in laparoscopic excision of choledochal malformation. Note that the umbilical port is a GelPOINT (Applied Medical, Rancho Santa Margarita, California).
Intraoperative endoscopy
• Place an additional 5 mm trocar in the left epigastrium, which will be used for insertion of a paediatric ureteroscope or cystoscope. Insert the tip into the common channel to irrigate and clear debris under vision. A similar manoeuvre is necessary using the left paraumbilical trocar for endoscopic visualisation of the hepatic ducts.
Removal of choledochal malformation
• Incise the anterior wall first, so that the posterior wall can be dissected free under laparoscopic control. Dissection is initiated by incising the overlying peritoneum using monopolar diathermy and a Maryland dissector to establish a plane of dissection. Begin on the anterior wall and continue to the medial and lateral sides, and then to the distal portion.
• Transect the distal common bile duct as close as possible to the pancreaticobiliary junction and ligate the stump with an endoloop. Excise the remaining proximal portion, leaving about 10 mm of common hepatic bile duct for the anastomosis.
Extracorporeal transumbilical jejunal Roux-en-Y (Figure 8.2)
• Exteriorise a segment of proximal jejunum by extending the umbilical port incision. Complete a sutured jejunojejunostomy with apposed limbs as for a LapKas using a relatively short, unstretched Roux limb.
• We make an antimesentric enterotomy about 5 mm in length, for the HJ near the closed end of the Roux limb, to allow the common hepatic duct to be anastomosed as close as possible to the closed end of the blind pouch. We avoid diathermy but temporarily oversew it to return it to the abdomen.
Hepaticojejunostomy
• Two further two ports (Figure 8.3) are used to facilitate intracorporeal suturing.
• Lateral right subcostal port
• Between the right subcostal and right upper quadrant ports for the laparoscope
• The port in the right upper quadrant is used for the needle holder in the right hand. Then, the anastomosis is performed in the same direction as for open surgery.
• The end-to-side HJ is performed using interrupted 5/0 or 6/0 absorbable sutures with the right upper quadrant port as a needle holder in the right hand, the 5 mm port for the scope and the 3 mm subcostal port as a needle receiver in the left hand.
• Exteriorise both the right and left edge sutures as traction sutures during anastomosis of the anterior wall.
• Usually, a tube drain is inserted in Morison’s pouch.*
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




