Menopause
DEFINING THE MENOPAUSE TRANSITION
Over the past two decades there has been much discussion about defining the terminology surrounding the last period. Sherry Sherman has aptly summarised some of the terminology, drawing together the WHO and International Menopause Society (IMS) recommendations (Box 53.1).1
BOX 53.1 Menopause terminology
Source: adapted from Sherman 20051
EPIDEMIOLOGY
In Western countries, the average age at FMP is 51 years, with a normal range of 40–60 years.2 The four or five years leading up to the FMP are characterised by menstrual irregularity, often initially cycle shortening, followed by cycle lengthening, although there is much normal variability. There are some minor variations in cycle patterns across different cultures but, as will be discussed later, quite marked differences in the symptoms are experienced across the menopause transition.
SYMPTOMS
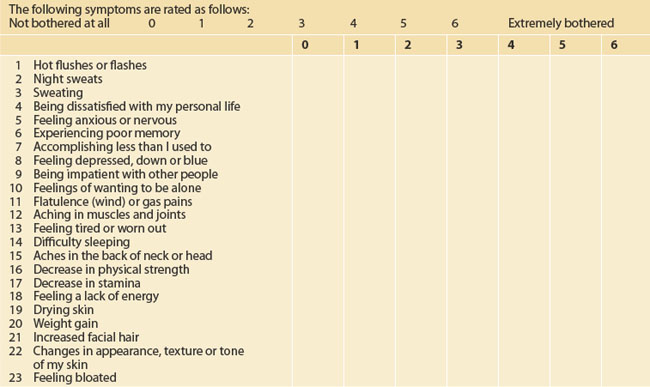
Some of the symptoms experienced by women in the menopause transition are listed in Box 53.2.
BOX 53.2 Symptoms that might be due to the menopause transition
Formication (a sensation of ‘ants’ crawling on the skin)
The Melbourne Women’s Midlife Health Project is a prospective, longitudinal study of healthy women passing through the menopause transition.3 The study began in 1991 and used random telephone dialling to recruit Australian-born women aged 45 to 55 years. One hundred and seventy-two women were premenopausal at the time at baseline, and by the end of the seventh year of annual follow-up had advanced to the peri- or postmenopausal interval.
CULTURAL DIFFERENCES
There appear to be marked cultural differences in attitudes to menopause. In a study of Sydney women, Asian women generally appeared to view menopause in a more favourable light than Western women, who linked menopause with ‘getting older’. Asian women were also less likely to admit to a healthcare professional that they were suffering from vaginal dryness, but if a doctor raised the issue, they were very grateful.4,5
Among Indian women, only 34% complained of hot flushes; more were concerned about depression and memory loss.6 Unemployment was associated with more flushing and depression. Lebanese Muslim women reported high rates of feeling tired and worn out, as well as aches and pains, as they went through the menopause transition.7 Sixty-three per cent reported hot flushes and more than half had noticed vaginal dryness during intercourse.
Chinese women largely see menopause as a natural process.8 A group of Sydney-based Chinese women had more vasomotor symptoms (34%) than those women who live in mainland China (10.5%) or in Hong Kong (10–20%). The top three symptoms reported by Sydney-based Chinese women were poor memory (76.4%), dry skin (69.1%) and aching in muscles and joints (68.3%). Some told the interviewers that their vaginal dryness problem was so severe that they had given their husbands permission to have sex with someone else.
Among Greek women, most were more concerned about back pain, aches, pains and fatigue than about hot flushes.9 Seventy-nine per cent of the postmenopausal Greek women had vaginal dryness, and there was a high rate of sexual problems.
THE MENOPAUSE CONSULTATION
HISTORY
The initial menopause consultation is a long session and often takes at least 30 minutes. It might be facilitated by some pre-reading and by using one of the many menopause-scoring charts that are available, such as the MENQOL (Menopause-specific Quality of Life Questionnaire, Table 53.1).10
The following should be particularly considered while taking a ‘menopause’ history:
TESTS
All that flushes is not menopause. Consider the differential diagnosis of ‘night sweats’ (see below) including viral infection, tuberculosis, neoplasm, hyperthyroidism, sleep apnoea, gastro-oesophageal reflux disease, alcohol excess and hypoglycaemia.12
If early menopause is suspected in a woman under 30 years of age, it might be prudent to measure her FSH levels three times over 2–3 months. In this way, the diagnosis is usually readily confirmed. Antimüllerian hormone (AMH) is a relatively new blood test that may give some information on ovarian reserve.
MANAGING MENOPAUSE
LIFESTYLE ISSUES: THE ESSENCE MODEL
Exercise
Regular exercise is particularly important during and after menopause, not only to help manage symptoms but also to help prevent a range of chronic conditions such as heart disease, cancer, dementia and osteoporosis. Regular moderate activity will help weight management and can help to improve sleep and maintain mental and physical vitality and performance in menopausal women.13,14 Vigorous aerobic exercise can precipitate hot flushes, in some women.
MANAGING HOT FLUSHES
In Western culture, the most common menopause symptom is the hot flush (referred to as ‘hot flash’ in American literature). This typically begins as a feeling of intense heat in the chest and neck which soon rushes up over the head and then over the rest of the body. It lasts a few minutes and might be associated with feelings of nausea, palpitations, dizziness and formication. The sufferer usually goes bright red and ends up with a drenching sweat, often followed by chills and shivering. The menopausal hot flush can be extremely unpleasant. The frequency varies considerably, from 1–2 a day to 10–20 an hour, day and night. During the flush, central temperature does not rise, but skin temperature goes up by 5–7°C.
DIFFERENTIAL DIAGNOSIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree