CHAPTER 19 Menopausal Health
PERIMENOPAUSE AND MENOPAUSE: AN OVERVIEW
In other cultures women do not report severe symptoms of menopause and menopause is not managed medically. Relying solely on a medical perspective (or disease model) of menopause does not account for the impact of culture and other social influences and may ignore the variety of patient perspectives on the menopausal transition.1
It is estimated that by the year 2015, 50% of all women in the United States will be menopausal. Women’s opinions and experience of menopause are changing. Until recent decades, menopause was a hushed topic for the 40 million American women going through “the change.” Times have changed and women today are openly looking for strategies to maintain their health and minimize discomforts. Women are also concerned about preventing the problems that commonly arise during and after menopause; for example, cardiovascular disease and osteoporosis, which may occur partly as a result of the decline in estrogen that is the hormonal hallmark of menopause. Although perimenopause—the commonly symptomatic phase leading to the permanant cessation of the menses—may be associated with varying degrees of discomfort from mild to severe, it is important to remember that this can be the beginning of a welcomed new phase of life for women. Social factors are sometimes more predictive than biologic factors of whether women will develop symptoms. A number of studies have found that women who report increased freedom, social status, and mobility after menopause are less likely to report negative symptoms. 2 3 4 5 6 In the United States, fear of aging and higher socioeconomic status are more frequently associated with negative menopausal symptoms than are body mass index or history of bilateral oophorectomy. A definition of menopause must take into account the impact of “social/cultural factors in order to encompass the range of experiences that women experience at the menopause transition. This biocultural definition permits exploration of the worldwide differences in menopause within the framework of the human life cycle and appropriately accounts for the influence of medico-cultural definitions of the menopausal transition.”1
WHAT IS MENOPAUSE?
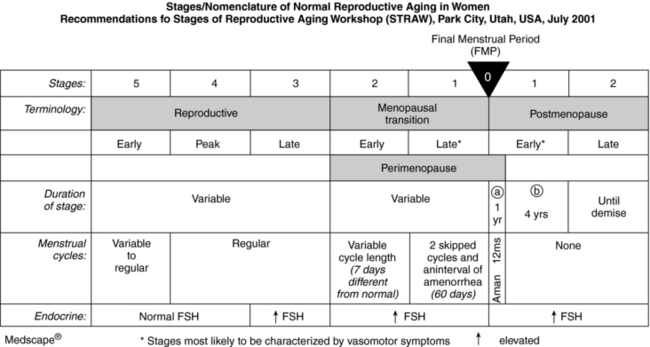
The term menopause is typically used to refer to what are actually three distinct phases: perimenopause, menopause, and postmenopause (Fig. 19-1). Perimenopause refers to the period of 2 to 8 years before the cessation of menstruation, during which regular cycles of ovulation and menses become irregular prior to terminating, a natural result of declining hormone levels, until one year after the cessation of menstruation. An elevated follicle stimulating hormone (FSH) level of 60 to 100 mIU/L on two tests done at least 1 month apart is considered indicative of menopause, although not definitive. Other hormonal indicators of the perimenopause are a luteinizing hormone (LH) level greater than 50 mIU/L and an estradiol level <50 pg/mL. The complete termination of menstrual bleeding for 12 months in the absence of another cause of amenorrhea heralds menopause and indicates that reproductive capabilities have ceased. Postmenopause is the time after complete cessation of menses. Despite ethnic, racial, and cultural variations, the median age around the world of 51 years for menopause indicates there are some common biological elements, although individuals range from ages 40 to 58 years old. However, there is a great deal of cultural disparity related to symptoms that arise during this period. For example, according to the World Health Organization (WHO), menopausal vasomotor symptoms are not as problematic for women worldwide as they are for women in the United States and other Westernized nations. Along with diet and exercise patterns, cultural attitude differences toward menopause may play some role in these epidemiologic differences.7
HERBAL STRATEGIES: AN OVERVIEW
Botanical treatments must also be placed in the context of a holistic approach that recognizes and addresses social, emotional, psychological, and other factors that can impact women, and must be proactive in helping women to prevent the development of symptoms during this time in their lives, especially heart disease and osteoporosis.
Depression and Anxiety
Hormonal changes, worries about aging, personal concerns, loss of sleep, inadequate nutrition, memory problems, and other physical complaints can fuel feelings of frustration and depression, and new concerns about health can lead to anxiety. Botanical therapies commonly used include adaptogens [see Chapter 6 Stress, Adaptation, the Hypothalamic-Pituitary-Adrenal-Axis (HPA) and Women’s Health], ashwagandha (Withania somnifera), eleuthero (Eleutherococcus senticosus), ginkgo (Ginkgo biloba), ginseng (Panax ginseng), dong quai (Angelica sinensis), motherwort (Leonurus cardiaca), St. John’s wort (Hypericum perforatum), and blue vervain (Verbena officinalis).
REFRAMING MENOPAUSE: THE WISE WOMAN PERSPECTIVE
The joy of menopause is the world’s best-kept secret. Like venturing through the gateway to enter an ancient temple, in order to claim that joy a woman must be willing to pass beyond the monsters who guard its gate… as thousands of women from all cultures throughout history have whispered to each other, it is the most exciting passage a woman ever makes.22
[Menopause] is not a natural condition; it is an endocrine disorder and should be treated medically with the same seriousness we treat other endocrine disorders, such as diabetes or thyroid disease.8
The medical definition of menopause is the end of menstruation. However, this definition fails to recognize women’s experience: that menopause, like puberty, is not a moment, not an end, but a metamorphosis that may take 5 to 10 years.1 Many practitioners—from both the scientific and alternative communities—define menopause as a state of loss, or an abnormal state. Menopause is described in disease terms as an endocrine disorder, estrogen deficiency, or simply hormonal imbalance. “This insistence on viewing menopause as a disease…defines older women as aberrant.”9 In contrast, the Wise Woman Tradition (woman-centered herbal medicine based on principles of nourishing the whole woman) defines menopause as a natural event occurring over several years, and during which the hormonal and nervous systems undergo cumulative and profound changes. In this woman-centered view, the menopausal years are an opportunity for conscious change and increased personal power, not a time of failure.
…the conventional view of menopause as a scary transition heralding ‘the beginning of the end’ couldn’t be farther from the truth.10
THE MEDICALIZATION OF MENOPAUSE
During the 1960s, with the popularization of hormone replacement, menopause became a treatable medical problem—and big business. Hormones became “the cure,” enabling women to remain “forever female.” The norm of care for middle- and upper-class white menopausal women in the United States from the mid-1960s to the present has been some form of hormonal supplementation: a combination of estrogen and progesterone for women who still have their uterus, estrogen for those without. It is now recognized that HRT increases the risk of endometrial and breast cancer. 11 12 13 15 16
Given the volumes of press devoted to HRT, one might assume that most US women use hormonal therapies at menopause; however, this is not the truth. One survey found that 52% of women wanted to avoid the use of hormones and 58% preferred alternative therapies for menopausal symptoms.17 Even before the recent cancellation of one large double-blind study of HRT, only half of all women over 50 had ever filled a prescription for estrogen or hormone replacement, and only one-third of those ever refilled the prescription. It is estimated that as many as 85% of the 37 million postmenopausal women [in the United States] do not want to use HRT.18 With growing concerns over the safety of HRT, many women—and even some physicians—are turning to alternatives. An understanding of the appropriate use of herbal medicines to nourish women during this transitional time and address common complaints associated with menopause, can ease this transition and promote health for women entering their “wisdom years.”
REFRAMING MENOPAUSE: WOMEN’S MYSTERY STORIES
Menopause is not simply an artifact of technology that has allowed us to expand our life expectancy and outlive our usefulness. Kristen Hawkes of the University of Utah studies hunter-gatherer cultures. Her “grandmother hypothesis,” based on observing the vigor and effectiveness of postmenopausal women in these cultures, demonstrates that postmenopausal women were critical to the health of their grandchildren, their community members, and the culture as a whole, and suggests that the presence of menopausal women in a society provides a survival advantage.19 The most industrious members of the Hazda culture are women in their fifties, sixties, and seventies says Dr. Hawkes. “The older woman knows the land, and its water, the seasons, the movements of the game, and the time to harvest each plant, she is not a sentiment, she is a requirement.”19 “Among many non-Western groups, the older woman enjoys increased status in the family and greater freedom in society at large. Menopause and the cessation of childbearing become positive events in a woman’s life. …“20 Reframing menopause from a “problem” to a “gift” is a direct help to most women. Women in cultures in which menopause is regarded as a gift have fewer problems with the physical and emotional changes that accompany it.21 A vigorous life keeps women vital. Vigorous exercise and a whole foods diet can help us live longer; reframing menopause can help us enjoy each passing year: gray hair, wrinkles, and all.
We have come to believe, patient and practitioner alike, that normal aging is a failure of our glands and that hormones—not just estrogen, but progesterone, testosterone, DHEA, and melatonin—are fountains of youth that will provide for us when our bodies fail. Reframing our view leads not only to a different attitude about normal menopausal symptoms, but to radically different treatments, in which herbs are not used as natural hormones, but as sources of the rich variety of helpful phytochemicals available from nature. Reframing menopause gives women a greater sense of self-worth. We reframe “loss of fertility” into “acquisition of postmenopausal zest.” This gives women something to look forward, a reward for passing through the gates of menopause. One manifestation of this reframing is the “Crone’s Crowning Ceremony.” This honoring ceremony, which celebrates a woman’s passage through the menopausal years, has become increasingly popular in the United States, especially among “the culturally creative” and women engaged in natural lifestyles. 2 23
A WHOLE FOODS DIET FOR MENOPAUSE AND BEYOND
Adequate, high-quality fat intake is essential; human steroid hormones are synthesized from cholesterol. Interestingly, studies have shown an inverse correlation between milk consumption and breast cancer. After tracking 4,697 Finnish women ages 15 to 90 for 25 years, researchers discovered that those “women who habitually drank the most milk had only half the breast cancer risk of those who drank the least.”25 A recent study done in the United States came to the same conclusion: Women who drank milk as children and continued to drink at least three glasses a day as adults had half the rate of breast cancer as those who drank little or no milk.26 Is it possible that cholesterol-rich foods, eaten as part of a healthy whole foods diet are health promoting, and that hydrogenated and partially hydrogenated vegetable fats are the real culprits in heart disease?27 A study of 61,000 Swedish women between the ages of 40 and 76 found that consumption of the monounsaturated fats, even from meat, milk, cheese, and butter, lowered the risk of breast cancer. For each 10 grams of monounsaturated fat [from dairy products and meat], the risk of breast cancer fell by 55%. For each 5 grams of polyunsaturated fat [from vegetable oil], the risk rose by 70%.28 Studies on the relationship between dairy and cancer, however, are often conflicting, with other studies demonstrating a direct correlation between dairy consumption and ovarian cancer.
The healthiest women in the world may be the women of Greece. They have some of the lowest rates of heart disease and breast cancer in the world.29 Their diets contain lavish amounts of olive oil, goat cheese, nuts, fresh vegetables, and meat. There is an inverse correlation between the amount of olive oil a Greek woman eats and her risk of breast cancer.30
HERBAL MEDICINES FOR THE MENOPAUSAL YEARS
Goals for helping women experience a healthy menopausal transition may include:
Nourishing Herbal Infusions
Nourishing herbal infusions provide nutritional, phytochemical support for menopausal and postmenopausal women with low cost and little effort. There is generally a high acceptance and follow-through rate among women of many ethnicities, cultures, education levels, and economic abilities.3 When amply extracted into boiling water, herbs such stinging nettle, oat straw, and red clover release generous amounts of vitamins, minerals, proteins, phytoestrogens, and other important constituents. 31 32 33 If the menopausal and postmenopausal diet is not mineral-rich, the entire woman suffers, not just her bones, but her heart, blood vessels, and immune and nervous systems. Minerals may be difficult to get, even in an adequate diet.32 Mineral values in commercial foodstuffs have decreased dramatically since the early part of the twentieth century.32 Regular use of nourishing herbal infusions can help to close this gap. 32 34 35 36
Cooked greens are also a rich source of minerals, as are edible seaweeds. Herbal vinegars are another great source of minerals and a way to encourage women to consume herbs daily, along with a healthful salad. Minerals are poorly absorbed from encapsulated herbs, and the amount taken is very small. Mineral-rich herbs are more like foods than medicines or drugs, and need to be consumed in dietary quantities—1 to 4 cups of infusion, not tea, or 1 to 3 tablespoons of infused vinegar daily. One cup of nourishing herbal infusion, prepared by steeping 35 g of dried herb in a liter of boiling water overnight, provides 100 to 400 mg of calcium. A tablespoon of medicinal herbal vinegar, prepared by macerating fresh herbs in vinegar for six weeks, may provide up to 50 to 100 mg of calcium.37
Supporting the Adrenals
Adrenal stress is often overlooked as a factor possibly contributing to a number of menopausal complaints including increased stress and irritability, panic attacks, emotional lability, fatigue, night waking, and possibly even night sweats. 38 39 Stinging nettle (Urtica dioica) is an excellent herbal ally. Fresh nettle leaves are eaten in soups, or as a cooked green or fresh or dried herb; 2 to 4 cups is a daily nourishing infusion. There is no scientific evidence exploring the effects of nettle on the adrenals; however, many herbalists corroborate the observation that nettle improves many symptoms associated with chronic stress and has rapid, reliable effects. Other adaptogenic herbs are also important for providing adrenal support. See Chapter 8 for a comprehensive discussion of adaptogens, as well as elsewhere throughout this book.
Supporting the Liver, Nourishing the Blood: A Vital Component of Menopausal Health
Traditional Chinese medicine (TCM) sees menopausal symptoms such as night sweats, hot flashes, memory loss, sleep disturbances, emotional swings, and even sometimes heart disease, as a result of liver qi stagnation, excess liver fire, and blood and yin deficiency.40 Many herbs are used in TCM to treat these “imbalances.” Among the most commonly used by Western herbalists as analogues for the Chinese herbs for moving liver qi and cooling heat are dandelion (Taraxacum officinale), yellow dock root (Rumex crispus), burdock root (Arctium lappa), motherwort (Leonurus cardiaca), and bupleurum (Bupleurum falcatum). Dong quai (Angelica sinensis) is perhaps the most popularly used herb for nourishing the blood. For use of traditional Chinese herbs, women can be referred to acupuncturists and TCM herbalists.
Phytoestrogens and Menopause
Phytoestrogens are hormones made by plants for their own biological needs. They weakly activate estrogen receptors in mammals and are found in ordinary foodstuffs such as whole grains, many legumes (not just soy), root vegetables including carrots and yams, seeds (e.g., flax), and nuts, as well as in herbs. 42 43 A diet rich in phytoestrogens confers benefits such as reduction of breast cancer risk, with little effect on premenopausal women’s cycles. 44 45 46 47 Phytoestrogens may also help prevent osteoporosis, high blood pressure, heart disease, and senility. 48 49 Phytoestrogens are ubiquitous in plants; only a totally plant-free diet would prevent exposure to them. Thus, phytoestrogenic foods are generally considered safe for long-term, daily use. Phytoestrogenic herbs and supplements, however, may not be safe for daily or long-term use for women at risk of developing estrogen-dependent cancers.50
A FEW WORDS ON EXERCISE
Although exercise alone is not sufficient to prevent heart attacks, osteoporosis, or fractures, it is vitally and tremendously important in their prevention and for the promotion of healthy hearts, healthy bones, and longevity.51 Exercise not only strengthens bone, it also increases muscular flexibility and improves balance. A broken bone can cause a fall, but poor balance leads to more falls and more broken bones. Plus, of course, exercise improves the functioning of the heart, counters depression, and may even help prevent breast cancer. The amount of exercise needed varies, but 30 minutes daily is a goal most women can easily achieve and maintain. Any kind of exercise helps, but best results are found with a mix of strength building (such as weight training), simple walking—brisk if possible, and flexibility improvement with tai chi and yoga. Best of all, we are never too old and never too unfit to begin benefiting from some form of exercise.
SUMMARY
Eclectic Specific Condition Review: Menopausal Symptoms
HORMONE REPLACEMENT THERAPY: RISKS, BENEFITS, ALTERNATIVES
Today, the main reasons for prescribing HRT are relief of menopausal symptoms and prevention or management of osteoporosis. Strong evidence from both observational studies and RCTs show estrogen to be highly effective for controlling hot flashes and genitourinary symptoms.54 Urogenital atrophy and vasomotor instability are improved with HRT.
CONVENTIONAL TREATMENT APPROACHES
Until relatively recently, the allopathic gold standard of treatment for menopause has been HRT. Approximately 38% of postmenopausal women in the United States in 1995 used HRT, estrogen with or without progestin, to treat symptoms of menopause and prevent chronic conditions such as cardiovascular disease and osteoporosis.55 In 2000, 46 million prescriptions were written for Premarin (conjugated equine estrogens), making it the second most frequently prescribed drug in the United States.56 HRT was indicated for the classic symptoms of hot flashes and night sweats, which related to declining estrogen levels and are reported by 85% of US menopausal women. 57 58 HRT can effectively treat menopausal symptoms such as vasomotor instability (hot flashes), mood swings, concentration difficulties, dyspareunia, and vaginal irritation caused by dryness.59
For women with an intact uterus, HRT includes both an estrogenic agent and a progestin. Progestins are generally indicated to offset the increased risk of endometrial cancer with the use of unopposed estrogen. For women using both an estrogenic agent and a progestin, there is a choice between cyclic and continuous dosing regimens. With the cyclic dosing regimens (intermittent high-dose progestin and estrogenic withdrawal), women can anticipate resuming a predictable (but artificial) menstrual cycle. With the continuous regimens (continual estrogen and low-dose progestin, without withdrawal), women can anticipate amenorrhea with occasional erratic spotting. Progestins are usually not recommended for women who have had a hysterectomy.60
The preventive effects of HRT on long-term health outcomes are now challenged by new data from clinical studies. In terms of beneficial effects, randomized clinical trials have proved that HRT is effective for vasomotor and urogenital symptoms.61 A meta-analysis of estrogen treatment (oral or intravaginal) for urinary incontinence revealed a significant improvement in subjective symptoms, but no improvement in objective measures such as urodynamic testing.62 It is unclear if HRT helps directly with depression and other nervous system disorders. A “domino” effect may occur; for example, relieving hot flashes may improve sleep, which may improve mood.63
Osteoporosis
Another area where HRT was found to be helpful was for the treatment of osteoporosis. In the United States, 4 to 6 million women have osteoporosis. The consequence is that more than 250,000 hip fractures occur annually, with a health care cost of approximately $14 billion per year. Hip fracture carries a 10% to 20% risk of death within a year and a 25% chance of institutionalization.64 After age 35 men and women start to lose approximately 1% of bone mass each year. However, bone loss is accelerated during the first 3 to 4 years after menopause. Estrogen therapy inhibits age-related bone loss after menopause by acting on osteoclasts (bone resorbing cells) and osteoblasts (bone-building cells) to decrease bone resorption. Estrogen also helps calcium to be absorbed in the gut. The daily dosage required to prevent bone loss is 0.625 mg of conjugated estrogen, but even 0.3 mg may suffice if taken with adequate calcium supplements.59 Estrogen must be taken for at least 7 years to provide significant benefit and the risk of osteoporosis reverts back to baseline once the estrogen is discontinued.54 Bone loss resumes within a year after stopping HRT, however, and bone turnover rises to the level of that in untreated women within 3 to 6 months.65 Randomized controlled trials have shown that HRT reduces bone loss at clinically relevant sites such as the spine and neck of the femur.66 The Women’s Health Initiative (WHI) study was the first randomized controlled trial to show a reduction in hip fracture with HRT.67 No herbal product studied has been proven effective in the prevention or treatment of osteoporosis.68
Nonhormonal therapies such as bisphosphates (e.g., Fosamax) and selective estrogen receptor modulators (SERMS) are as effective as HRT for preventing fractures. Bisphosphates inhibit osteoclast activity in the bone. Randomized controlled trials have demonstrated Fosamax efficacy increasing BMD and reducing fractures.69 Etidronate (Didronel) is another bisphosphate. It is FDA-labeled for the treatment of Paget’s disease, but has had an off-label use as a treatment for osteoporosis in patients who cannot tolerate Fosamax. Intranasal calcitonin is a polypeptide hormone that also inhibits osteoclastic activity; an intranasal form is now available for treatment of established osteoporosis. A selective estrogen receptor modulator, raloxifene (Evista), has been FDA labeled for prophylactic treatment of osteoporosis. For women whose main interest is prevention of osteoporosis, this agent offers an alternative to traditional HRT. Other selective estrogen receptor modulators pending FDA labeling include droloxifene and idoxifene.59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree