7
Male Infertility
Where and How Sperm are Made
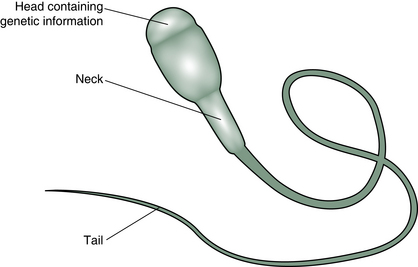
The sperm, known in biological circles as a ‘spermatozoon’, is a long thin cell with a head which contains the genetic material and a tail which propels the genetic material towards its destiny (Fig. 7.1).
The Sperm Factory
Sperm are made in the male gonads, which are known as the testes or testicles. These organs hang outside the body in the scrotum. The temperature in the scrotum is several degrees lower than that in the abdominal cavity just above it, and this low temperature seems to be important for the function of the sperm-making cells. Just 24 h of raised scrotal temperatures will cause malfunction of sperm production in animal studies.1
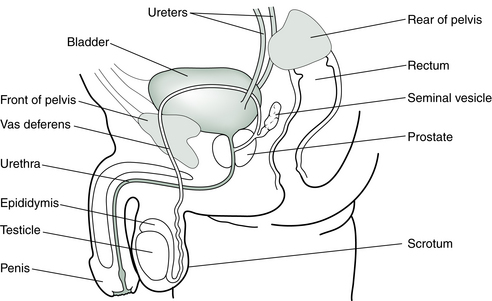
The sperm form over a period of about 48 days in the tubules in the testes, nurtured by the Sertoli cells, in sequential generations at different stages of development. They then spend 2 or more weeks in the epididymis (a fine, coiled tube 6 m long and about double the width of a scalp hair) to mature before moving into the vas deferens and the urethra on their way out of the body (Fig. 7.2). The ejaculate contains a mixture of sperm and fluid from the prostate gland and seminal vesicles.
To be considered fertile, the male of the human species needs to deposit a minimum of 40 million sperm in the female vagina during intercourse in the hope that just one will have a successful encounter with the egg. Once inside the acid environs of the vagina, few sperm can survive and within just a few minutes, the walls are littered with the corpses of millions. Over the next few hours all but a few are dead. The survivors are the sperm which were able to negotiate a passage through the cervix with the help of the protective cervical mucus and the dipping action of the cervix at orgasm, followed by the contractions of the uterus which propel the sperm into its higher reaches. Once inside the female reproductive tract, the sperm will be lured towards the egg in the tube by chemical signals.
Semen Analysis
Normal Parameters
Current World Health Organization (WHO) standards2 for assessing male fertility are:
• Volume: more than 1.5 milliliter (mL)
• Count: more than 15 million sperm per mL
• Motility: more than 50% moving vigorously and purposefully
• Morphology: more than 4% normal forms (i.e., no deformities of the head, midpiece or tail).
‘Normal’ parameters, as they were defined less than two decades ago, described sperm counts of twice this amount and a much higher percentage of normal forms. The average sperm count has decreased by 1–2% per year from a substantially higher number decades ago.3 Standards for deposits in sperm banks have thus had to be lowered, or too many donors would nowadays be rejected.
Another way of assessing male infertility is to do retrospective studies of couples achieving or not achieving pregnancy. When a large population of men was studied, those who had succeeded in fathering a child in the previous 2 years had more than 48 million sperm/mL, with more than 63% moving, and more than 12% with normal morphology. Infertility was most likely if a man’s sperm count was less than 13.5 million sperm/mL, with less than 32% moving, and less than 9% having a normal shape. Men falling between these two groups had borderline fertility but could still establish a pregnancy.4
Some couples, however, have no trouble getting pregnant with sperm counts lower than normal. Some researchers in the field have gone so far as to say that sperm density tests are not always useful in distinguishing fertile from infertile men and are not useful in diagnosis or in monitoring the progress of treatment for male infertility.5 Ultimately, all that is really needed is one sperm!
These men are encouraged to avoid pesticides and other environmental toxins, heat sources and smoking, and to increase antioxidant intake. (See Ch. 12 for more discussion.) Frequent ejaculation (i.e. daily) is recommended to reduce the length of time sperm are exposed to reactive oxygen species in the testicular ducts.
Declining Sperm Counts
There has been a lot of press about the precipitous decline in sperm counts over the last few generations. The average male sperm count dropped 45% from 113 million/mL in 1940, to 66 million/mL in 1990. Also the volume of semen dropped, effectively making the reduction in total numbers of sperm per ejaculation 50%. The number of men with low sperm counts (<20 million/mL) has tripled (from 6% to 18%), while the percentage with high sperm counts (>100 million/mL) has decreased. The more recently a man was born, the lower the average sperm count and the greater the number of abnormalities.6
Such figures lead some specialists to speculate that if the decrease in sperm counts were to continue at this rate, in a few years we will witness widespread male infertility.3
The cause of this decrease appears to be the increased exposure to environmental pollutants, either during the time in the womb or later in life. PCBs (polychlorinated biphenyls), dioxin, phthalates, phenols and several pesticides such as DDT, have been shown to have a harmful effect on sperm as have the solvents used in manufacturing adhesives and printing inks and paints. Pregnancies of the partners of men exposed to damaging substances are also affected, experiencing a higher rate of stillbirth and premature delivery.7 Many of these substances and other chemicals used in farming or industry act like estrogens or anti-androgens.8–10 We will revisit this topic in more detail in Chapter 12.
While the body is able to break down and excrete natural plant estrogens, many of the man-made compounds which act like estrogen resist normal breakdown and accumulate in the body, exposing humans and animals to low-level but long-term exposure. This pattern of chronic hormone exposure is unprecedented in our evolutionary experience and adapting to this new hazard is a matter of millennia not decades.11
Prescribed drugs may also be implicated in reduced sperm counts. In some cases, the effects of these drugs last for months after they have been discontinued. Testosterone replacement therapy, anabolic steroid use, cancer medications, certain antibiotics, some blood pressure medications, some ulcer or reflux medication, drugs for ulcerative colitis and some antidepressants have been observed to affect sperm production (Table 7.1).
Table 7.1
Some pharmaceutical drugs and their possible effects on sperm
| Class of drug | Effect on sperm |
| Drugs for high blood pressure: | |
| e.g., spironolactone | Lowers sperm count |
| e.g., calcium channel blockers | Interfere with binding of sperm to egg |
| Drugs for peptic ulcers or reflux: | |
| e.g., cimetidine | Lowers sperm count |
| Drugs for ulcerative colitis: | |
| e.g., salazopyrin (sulfasalazine) | Lowers sperm count |
| Testosterone and anabolic steroids | Lower sperm count |
| Some chemotherapy drugs | |
| e.g., methotrexate | Lowers sperm count |
| Drugs for epilepsy: | |
| e.g., phenytoin | Lowers sperm count |
| Drugs for urinary function: | |
| e.g., nitrofurantoin | Affects sperm motility |
| Drugs for gout; | |
| e.g., allopurinol, colchicine | Lowers sperm count |
| Antifungal medication: | |
| e.g., Grisovin and/or Griseostatin (griseofulvin) or ketoconazole | Lowers sperm count and increases abnormal forms |
| Drugs for depression | |
| e.g., SSRIs serotonin reuptake inhibitors | May lower sperm count and motility |
| Some antibiotics | |
| e.g., tetracycline, erythromycin, gentamicin and nitrofurantoin | Lower sperm count, affect morphology |
Age and Sperm
It has long been known that a woman’s reproductive capacity reduces as she ages. But until recently, it has been assumed that the age of the male partner was irrelevant to the question of fertility – there are plenty of stories of septuagenarians impregnating younger women. It has taken a long time for the researchers to take a hard look at the influence of age on male fertility. The first indications that age might be relevant emerged from studies of miscarriage rates in couples of different ages (see Ch. 8) and, more recently, research has examined the effect of male age on conception rates. This has shown that the older a man is, the longer it is likely to take his partner to conceive, irrespective of her age. The study concluded that in a couple who eventually have a baby, the probability that it will take more than 12 months to conceive nearly doubles, from around 8%, when the man is younger than 25 years, to around 15%, when he is older than 35 years. In other words, men as well as women have a biological clock that starts ticking (though perhaps not so urgently) as they get into their 30s (Fig. 7.3).12

Figure 7.3 The older a man is, the longer it is likely to take his partner to conceive, irrespective of her age.
IVF outcomes are significantly reduced in couples where the husband is more than 50 years of age.13 Particularly, it is the morphology and motility that declines with age.14
Constriction and Heat
Putting pressure on the testicles reduces sperm motility. Men whose sperm are not swimming so well are advised to stop putting pressure on them by avoiding tight underpants or cycling a lot.15
The effect of overheating the testicles with saunas or hot tubs or laptops has also been examined by various groups and it turns out that men with poor sperm quality are better off jumping in the ocean or a swimming pool rather than the hot tub or the sauna.16
More discussion of lifestyle and environmental effects on sperm count and quality can be found in Chapter 9.
Diagnosis of Male Infertility in TCM
Sperm are delivered to the female genital tract in a fluid called semen. This fluid contains constituents important for sperm function and survival and for conditioning the lining of the uterus to accept an embryo containing the father’s proteins. Sperm constitutes only about 1% of the semen volume. The dynamic and fast-moving sperm represent the Yang within the moistening and nourishing Yin of the seminal fluid. When doctors of Chinese medicine are treating a sperm disorder, it is important that both the Yin and the Yang aspects are considered, i.e., both the sperm and the fluid containing them. You will see from the examples of treatments given below that both Yin and Yang are treated concurrently, with individual emphasis where necessary.
Male infertility, like female infertility, has everything to do with the Kidneys in TCM terms. As you will be aware, the Chinese medicine term ‘Kidney’ embraces more functions and areas in the body than does our concept of the kidney organs in Western medicine. Nevertheless, in Western medicine too, it is recognized that kidneys can be related to reproductive function, but this only becomes apparent when kidney function is seriously compromised. For men, renal disease has dire repercussions on fertility and sexuality.19
The basic requirement for full reproductive potential is strong Kidney Jing and a normal balance of Kidney Yin and Yang. Most cases of male infertility will be diagnosed as Kidney Yin or Yang deficiency. There appears to be a genetic base for male infertility in about 60% of cases.20 This alerts TCM doctors to the possibility that Kidney Jing weakness underlies a majority of male infertility cases and will often need to be addressed in treatment protocols alongside the usual treatments for Kidney Yin and Yang. However, where exposure to environmental pollutants in later life has caused a drop in sperm count and quality, we would not assume a Kidney Jing deficiency, although Kidney Yin and Yang function will still play a part in our treatments.
Kidney Yin Deficiency
In addition, there may be some Kidney symptoms such as urination frequency, dark scanty urine, poor urine flow, tinnitus, and heel pain. There may be rather a high libido but this is not necessarily accompanied by strong sexual prowess. There may also be premature ejaculation and inability to sustain erections for long.
Kidney Yang Deficiency
Damp-Heat
As a cause of infertility, this is not so common in Western or developed countries because antibiotics are usually used promptly to address any genitourinary infections. But in China or other developing countries, low-grade untreated infections commonly contribute to the sort of inflammation which does not provide a conducive environment for sperm manufacture. In cases where there is infection in the urogenital tract, antibiotics may be appropriate and studies have shown that sperm counts can improve after such treatment.21
The nature of the antibiotic treatment is important, however, as some antibiotics may affect sperm function adversely.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree