CHAPTER 59 Lower intestinal tract disease
Introduction
These close relationships have led to joint working in outpatient clinics and operating lists, and also to the emergence of multidisciplinary meetings. These can be held locally and regionally. They provide education for the members into the understanding of symptoms and treatment within the multidisciplinary field; meetings can be used to plan treatment and joint procedures, as well as for education (Mirnezami et al 2008).
A basic understanding of the anatomy and physiology of the colon, rectum and anus is essential in order to understand the symptoms associated with the posterior compartment (see Chapter 50).
Investigations
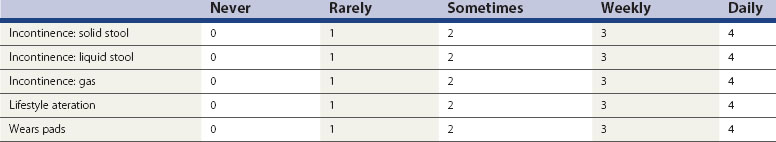
A detailed history and examination is often adequate to initiate basic treatment. It is always important to exclude serious pathology, and patients may require full bowel imaging of some sort (colonoscopy, barium enema or computed tomography colonography). In recent years, measurement of patient benefit from treatment has led to the use of incontinence and constipation scores which can be recorded before and after treatment. The Cleveland Clinic Incontinence Score (Table 59.1) is most commonly used.
The Cleveland Clinic Incontinence Score does not include aspects of urgency, but the Vaizey score (Vaizey et al 1999) attempted to address this. Vaizey et al reported that urgency of less than 15 min is not usually a problem; however, when patients are not able to hold for more than 2 min, this has a significant impact on quality of life. A recent study (Cotterill et al 2008) took comments from a panel of seven clinical experts and from patients, and reported five key issues related to anal incontinence. These were unpredictability, toilet locations, coping strategies, embarrassment and restriction of social activities. This group are working on a new instrument to help validate treatments for anal incontinence based around quality of life as well as symptom severity.
Anorectal manometry
Anal manometry is not a single test but a series of measurements used to assess anal sphincter function, rectal sensation, rectoanal reflexes and compliance of the rectum (Kourakalis and Andromanakos 2004). The use of pull-through anal manometry allows assessment of the length of the functioning sphincter, resting pressures give a good estimation of internal sphincter function, and squeeze pressures assess external sphincter function. The patient is usually placed in the left lateral position, and manometry can be performed either using stationery pull-through or continuous pull-through techniques. Many catheters have four or eight channels, and these can therefore record different pressures in different parts of the external sphincter and internal sphincter at different levels. Using vector analysis, it is possible to look at the symmetry of the anal canal pressure, and combining this with anal ultrasonography can show whether there is a structural as well as a functional problem in either of the sphincter muscles. The rectoanal inhibitory reflex is usually assessed during the physiology. Absence of this may indicate a longstanding problem such as Hirschsprung’s disease. Rectal distension is assessed by inflating a balloon within the rectum; measurements are taken when the patient first feels the sensation of rectal filling, the feeling when there is maximum fullness, and then the feeling of urgent desire to defaecate. This can be extended to when the volume is unbearable. If the rectal threshold is low, even with a normal anal pressure, continence may be impaired.
Anal skin sensation is usually assessed by some form of electrical stimulation. Pudendal nerve terminal motor latencies are performed by stimulating the pudendal nerve transanally through the lateral wall of the rectum as the nerve transverses the ischial spine, using a St Mark’s electrode on the tip of the examining finger. The normal delay between stimulation and recording is less than 2.2 ms and a longer delay suggests that there has been damage to the pudendal nerve. A lengthening of the pudendal nerve latency is often associated with poorer outcomes after surgery, and may suggest that the patient’s incontinence is associated with nerve damage. An important outcome measure for sphincter repair is whether there is any pudendal neuropathy, as patients with pudendal neuropathy only have a 10% chance of success compared with 80% in patients without pudendal neuropathy (Laurberg et al 1988).
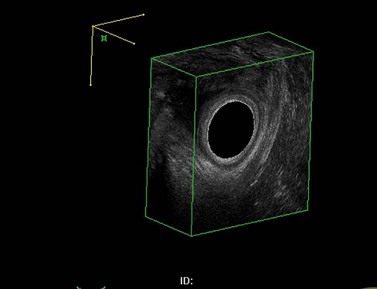
Ultrasound and dynamic imaging
The investigation of choice for structural abnormalities within the anal sphincter is a three-dimensional anal ultrasound. A data set can be captured and then manipulated at a later date to look at structural abnormalities throughout the anal canal (Figure 59.1).
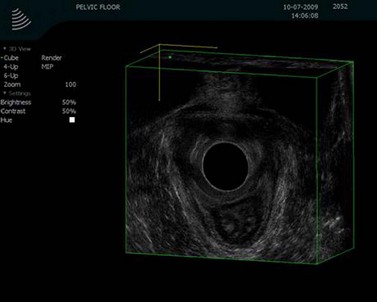
Using the same anal probe transvaginally, it is possible to examine the levator plate and many other anatomical aspects of the pelvic floor. Asymmetry within the levator plate suggests damage during childbirth and often leads to the anus being diverted to the side of the damage (Figure 59.2).
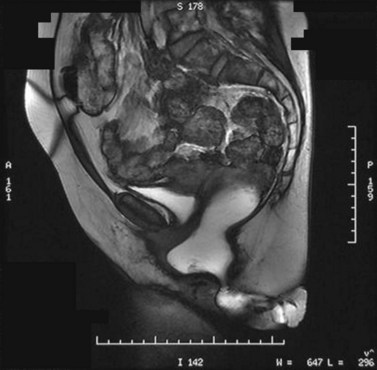
Further assessment of the pelvic floor often requires some form of proctography. In order to assess the whole pelvic floor using defaecating proctography, patients require not only contrast within the rectum but also in the small bowel, vagina and bladder. Defaecatory magnetic resonance imaging (Figure 59.3) can show all these parts of the pelvic floor. There are very few open magnets where a patient can sit and defaecate; therefore, the majority of these studies are performed with the patient lying prone.
It has been shown that magnetic resonance proctography shows increased evidence of other pelvic floor abnormalities over defaecating proctography. However, it underestimates the size of rectoceles and intussusception (Pilkington et al 2009).
Common Conditions and Treatments
Haemorrhoids
Piles often present with a combination of symptoms, including itching, soreness, postdefaecatory leakage and lumps around the anus. It is thought that the sliding anal canal theory proposed by Thompson (1975) is the most likely cause of piles, where Treitz’s muscle is stretched repeatedly resulting in fragmentation of the connective tissue. Haemorrhoids may be small and highly symptomatic, or large and asymptomatic. This is especially so in elderly female patients where normal anal canal pressures are low, and this can result in prolapse but little in the way of symptoms. Several classifications of haemorrhoids have been used over time. Goligher’s classification (Goligher 1976) describes the degree of prolapse and whether these reduce spontaneously (grade 2), require manual reduction (grade 3) or are permanently prolapsed (grade 4). However, although this is good for the description, it does not consider the symptoms of the piles. Work by Lunniss and Mann (2004) has produced a more accurate and useful classification of haemorrhoids, dividing them into non-prolapsing and prolapsing, looking at not only the morphological presentation but also any additional features such as pruritus or pain.
Treatment of haemorrhoids
Estimates of the proportion of the UK population affected with haemorrhoids range from 4.4% to 24.5%. In 2004–2005, approximately 23,000 haemorrhoidal procedures were carried out, and approximately 8000 of these were excision haemorrhoidectomies (National Institute for Health and Clinical Excellence 2007a).
Medical treatment for haemorrhoids
Patients with symptomatic but small internal haemorrhoids are best treated with dietary management; increasing the intake of fluid and fibre is the mainstay of this treatment. The typical symptoms of internal haemorrhoids are rectal bleeding and, sometimes, prolapse; avoiding straining by these dietary methods usually improves the symptoms. Dietary manipulation also improves rectal bleeding alone from grade 1 and grade 2 haemorrhoids, and this has been proven in three randomized controlled trials (Cataldo et al 2005).
Patients with persistent symptoms from grade 1, 2 or 3 haemorrhoids may benefit from an outpatient procedure. The most common procedure used and probably the most effective is haemorrhoidal banding. Other procedures that may be offered include sclerotherapy, infrared coagulation and cryotherapy. All of these treatments are aimed at decreasing the haemorrhoidal tissue volume and fixing the anal cushion back to the rectal wall. A meta-analysis of outpatient treatment suggested that rubber band ligation was the most effective of all outpatient procedures and was associated with a lower recurrence rate (MacRae and McLeod 1995). It is, however, relatively painful and the pain associated with the procedure increases with the number of rubber bands that are used to treat these piles. It is essential that the bands are placed well above the dentate line, or the immediate pain felt from the sensate epithelium is excruciating and patients will need to have these bands removed. Rubber band ligation is associated with a success rate of 65–85%, but follow-up at 5 years shows a relatively high recurrence rate. Following outpatient procedures for haemorrhoids, approximately 2% of patients report pain and less than 1% report urinary retention. Major complications include significant haemorrhage, which may take place immediately or as a secondary haemorrhage between postoperative days 7 and 10.
Operative procedures for haemorrhoids
Haemorrhoidectomy of any sort should only be offered to patients with large external haemorrhoids or significant prolapse, or those who have been resistant to outpatient procedures. Open haemorrhoidectomy is effective; however, it is associated with pain, infection and other complications, such as incontinence and stenosis of the anal canal. More recently, patients have been able to undertake a less painful form of surgical procedure called a ‘stapled haemorrhoidopexy’. The evidence for this has been reviewed by the National Institute for Health and Clinical Excellence (NICE) (2007a). A stapled haemorrhoidopexy is an intrarectal procedure that aims to reduce the prolapse of haemorrhoidal tissue by excising a band of the prolapse anal mucosal membrane above the dentate line using a specific circular stapling device (PPH03 Ethicon). The procedure is thought to interrupt the blood supply to the haemorrhoids and reduce the potential continuing prolapse of mucosa. The NICE review studied 27 randomized controlled trials of stapled haemorrhoidopexy and found that the procedure was associated with less pain up to 14 days following surgery, shorter wound healing times and significantly less postoperative bleeding. On the basis of the evidence in the literature, it was felt that a stapled haemorrhoidopexy offered benefits over a conventional haemorrhoidectomy in the reduction of short- and medium-term postoperative pain. However, although stapled haemorrhoidopexy is associated with a higher rate of recurrent prolapse, the committee concluded that ‘a stapled haemorrhoidopexy should be recommended as a treatment option for people in whom surgical intervention is considered appropriate for the treatment of prolapsed internal haemorrhoids’.
Anal fissures
Patients with pelvic floor straining and post childbirth often present with anal pain associated with an anal fissure. An anal fissure is a tear running longitudinally in the epithelium of the anal canal, the majority of which lie posteriorly in the midline. Acute fissures are usually superficial, whereas chronic fissures may be associated with secondary changes including a sentinel tag or hypertrophied anal papilla. As with all acute and chronic anal conditions, efforts should be made to identify any precipitating causes or associated diseases (Crohn’s disease or anal carcinoma). A recent consensus statement from the Association of Coloproctology of Great Britain and Ireland covers aspects of diagnosis and treatment (Cross et al 2008). The most common presenting features are pain during defaecation which may last for several hours afterwards, as well as rectal bleeding. The most consistent finding on examination is spasm of the anal canal, and it is uncertain whether this is the result of or due to ischaemia. Many of the management options have been based around reducing the internal anal spasm, but as with many benign anal conditions, one of the most important measures is to increase dietary fibre and adequate fluid intake. The majority of fissures, especially posterior fissures, are associated with a high resting pressure and a low blood flow to the anoderm resulting from this spasm. However, postpartum fissures are usually anterior and may be associated with a rectocele. The scar formation may be associated with ischaemia; however, the resting pressures in these patients are usually low. If there are multiple fissures or the fissures are not in the midline, a differential diagnosis of Crohn’s disease, ulcerative colitis, human immunodeficiency virus and associated infections as well as neoplasia should be considered. An anal fissure may occur at any time in life but is most common between the second and fourth decades, with an equal distribution between men and women and a lifetime incidence of just over 11%. Inspection of the anus will usually reveal the fissure, and it is not usually possible to carry out any further examination due to the pain associated with the fissure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree