Chapter 668 Leg-Length Discrepancy
Leg-length discrepancy (LLD), or anisomelia, in children can result from a variety of congenital or acquired conditions (see Table 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ). Congenital conditions include asymmetrical growth from hemihypertrophy, vascular and lymphatic anomalies, Beckwith-Wiedemann syndrome, hemiatrophy, bone dysplasias (proximal femoral focal deficiency [PFFD]), fibular and tibial hemimelia (see Fig. 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com
). Congenital conditions include asymmetrical growth from hemihypertrophy, vascular and lymphatic anomalies, Beckwith-Wiedemann syndrome, hemiatrophy, bone dysplasias (proximal femoral focal deficiency [PFFD]), fibular and tibial hemimelia (see Fig. 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ), and Proteus syndrome. Associated acquired causes of limb length inequality include physeal fractures, infections involving the growth plate, fractures whose healing process stimulates growth, juvenile rheumatoid arthritis, and coxa vara. Neurologic diseases including spina bifida, cerebral palsy, head injury, and spinal dysraphisms, can also lead to LLD. These etiologies lead to structural limb length discrepancies, but soft tissue contractures of the lower extremity can also cause functional limb discrepancies even though the bones are of symmetrical length. Hip dysplasia can cause apparent limb length inequality of a functional type.
), and Proteus syndrome. Associated acquired causes of limb length inequality include physeal fractures, infections involving the growth plate, fractures whose healing process stimulates growth, juvenile rheumatoid arthritis, and coxa vara. Neurologic diseases including spina bifida, cerebral palsy, head injury, and spinal dysraphisms, can also lead to LLD. These etiologies lead to structural limb length discrepancies, but soft tissue contractures of the lower extremity can also cause functional limb discrepancies even though the bones are of symmetrical length. Hip dysplasia can cause apparent limb length inequality of a functional type.
Table 668-1 CAUSES OF LEG-LENGTH DISCREPANCY
CONGENITAL CAUSES
Defects in Growth
Bone Tumors and Bone Disease
Vascular
Miscellaneous
ACQUIRED CAUSES
Trauma
Developmental
Developmental dysplasia of the hip
Neoplastic
Neurologic
Infections and inflammatory
Miscellaneous
Diagnosis and Clinical Findings
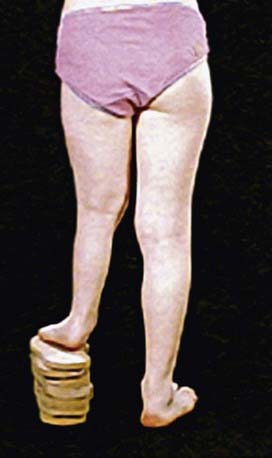
A diagnosis of leg-length inequality can be made by a pediatrician at a regular visit in infancy or early childhood or by a pediatric orthopaedic surgeon at a referral for an obvious limp in an older child. The initial diagnosis of LLD is made on physical examination, with gait asymmetry being the most common complaint. The traditional measurements of real and apparent leg-length inequality (measuring with a tape measure from the medial malleolus to the umbilicus or iliac crest) have led to inaccurate measurements. A more reliable method of clinically testing for limb length inequality is simple visual assessment of the posterior iliac crest level while the child is standing with his or her knees and hips in an extended fashion. Blocks of various sizes can then be placed under the short limb until the pelvis is level to give an estimate of the leg-length inequality (Fig. 668-2). Physical examination can also identify joint contractures and angular deformities that cause errors in clinical and radiologic measurements.
Radiographic Evaluation
Coupled with clinical examination, radiologic evaluation is used to guide the appropriate treatment decisions. Four different techniques are the most commonly used (Fig. 668-3): teleoroentgenogram, orthoroentgenogram, scanogram, and CT. Whichever method is initially used should remain consistent in all future studies in order to maximize accuracy and validity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree