CHAPTER 3 Laparoscopy
History
Examination of the body cavities using instrumentation has been practised by clinicians over many centuries. Most of the early techniques involved inspection of the bladder and urethra (Bozzini 1805). Light sources were introduced initially with alcohol flames (Desmoreaux 1865), and subsequently the incandescent light bulb. The first inspection of the peritoneal cavity was through the posterior fornix in the early 20th Century (von Ott 1901). Examination of other cavities was described soon afterwards (Jacobaeus 1910), with carbon dioxide used for insufflation more than a decade later (Zollikoffer 1924). The first diagnosis of an ectopic pregnancy followed (Hope 1937), as did female sterilizations. Veress first reported the spring-loaded insufflation needle as a technique for introducing a pneumothorax in patients with tuberculosis (Veress 1938).
Further advances were relatively slow with few clinicians inspired by the new techniques. The first description of sterilization in English was not until 25 years later (Steptoe 1967). Few therapeutic procedures were performed laparoscopically, although the technique gained widespread support for diagnosis.
The revolution in therapeutic techniques probably started with the report of the first laparoscopic hysterectomy (Reich et al 1989) and, with advances in instrumentation, light sources and camera systems, continued apace throughout the 1990s. However, a few practitioners attempted procedures that were beyond either their surgical training or ability, and responsible bodies rapidly concluded that regulation was required. The Royal College of Obstetricians and Gynaecologists (RCOG) established its training guidelines in 1994 with certification for those trained to perform at different levels. This has been repeatedly modified to bring the UK training into line with practice in other European countries.
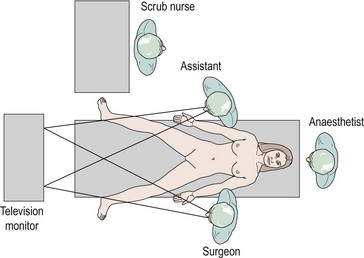
Theatre Set-Up
The authors believe that the television screen should be placed between the patient’s legs if the camera is inserted at the umbilicus. Figure 3.1 demonstrates that the view displayed on the screen is in the same direction in which the patient is lying and the surgeon operating. Many experienced surgeons place the television screen directly in front of themselves and behind the assistant. Under these circumstances, the surgeon is operating in a different direction to which he or she is looking; not only is this uncomfortable and ergonomically disadvantageous, but all images have to be transposed through 90 degrees, adding to the difficulties of hand–eye coordination. The additional advantage of placing the monitor between the patient’s legs is that only one screen is required.
The scrub nurse should stand in a consistent position, and instrumentation such as bipolar diathermy, scissors, graspers and suction irrigation should be placed reliably within easy reach of the surgeon. The scrub nurse should be within sight of the television screen, enabling anticipation of the next instrument required. A protective bar placed across the table prevents the assistant’s arm from resting on the upper part of the patient and potentially dislodging the endotracheal tube (Figure 3.2).
Equipment
The following items are essential.
Trocars
Many different types of trocar are available, which vary in size, length and design of the tip (Figure 3.3). The 12 mm, 10 mm and 5 mm trocars are used most commonly in gynaecological surgery. When performing complicated surgery, there can be many changes of instrument down any individual port. For this reason, the trocars have to be able to grip the abdominal wall, and there are various designs to facilitate this. Some of the more modern trocars have a type of ‘fish scale’, whilst others utilize a screw thread which can grip more effectively but increases the diameter of the incision. The trocar tip can be conical, pyramidal or a single flat blade in design. They create different sized and shaped incisions in the fascia, with the single flat blade and conical dilating tip producing the smallest defect. Optical trocars have a blunt clear dome-shaped tip housing a crescent-shaped blade. They allow a controlled sharp dissection of the abdominal wall layers under direct vision. These trocars can be inserted prior to insufflation and may be useful in obese patients with thick abdominal walls. Trocars may be disposable or reusable. Many laparoscopic surgeons have been persuaded to use disposable trocars because of their constantly sharp tips, the so-called safety devices to retract the tip when through the full thickness of the abdominal wall and to avoid contamination between patients. However, most surgical units find the cost of disposable trocars prohibitive for use with every case.
Camera system
Modern camera systems are an essential part of the laparoscopic surgeon’s equipment. There are few surgeons around the world who continue to operate by looking directly down the eyepiece of the laparoscope, even for minor diagnostic procedures. There is a clear advantage in being able to project the image on to a television screen that is visible to all members of the surgical team. Together with the ergonomic advantages of not having to stoop over the patient, this means that camera systems are now commonplace. The image seen through the eyepiece of the laparoscope is converted into electrical signals by a charge-coupled device housed in the camera head. These electrical signals are then processed by the camera control facility which is, in turn, connected to the television monitor. Cameras may contain one or three charge-coupled devices, each of which is colour specific, recording only one of the three primary colours. Most modern camera systems enable collection of digital images which are projected on to a digital monitor, although hybrid set-ups can co-exist. Some camera heads incorporate remote buttons to allow the operator to control various features of the imaging system, such as taking prints, operating the video recorder or white balancing. Some cameras are autoclavable but the majority of surgeons will place the camera system inside a sterile plastic sheath before connecting to the laparoscope (Figure 3.4).
Operating instruments
There are innumerable types of operating instruments, and individual surgeons will have their own preferences. Essentially, the instruments can be divided into the jaws, the shaft and the handles. Jaws have been designed which mimic all the instrumentation available for open surgery, plus many others. Examples are shown in Figure 3.5. The shafts may be of 10, 5 or 3 mm diameter and may or may not contain a diathermy attachment. For non-disposable instrumentation, it is often the shaft that is the most difficult part of the instrument to keep clean and maintain. Handles come in a variety of ergonomic designs, according to surgeon preference. Handles may be ratcheted or non-ratcheted in a variety of ways. Most non-disposable instruments have a detachable handle in order to convert an instrument into one with or without a ratchet. Surgeons have their favourite graspers and, as with most situations, it is more important to be familiar with an instrument and to know its limitations than it is to have a wide variety of instrumentation that is less familiar.
Port Entry
A variety of techniques have been described for insufflation in order to allow the surgeon to view the pelvic and abdominal contents through the laparoscope. A great deal of discussion has occurred, particularly in medicolegal circles, regarding which is the safest technique. Complication rates for laparoscopy are so low that individual surgeons are unlikely to be able to evaluate the various entry techniques in their own practice. However, the number of laparoscopies performed is so high that the overall effect of an inferior technique could be significant for a number of patients around the country each year. Traditionally, gynaecologists are familiar with the closed technique, having performed many diagnostic laparoscopies in their training. General surgeons perform fewer laparoscopies, and these are usually for major procedures. They are usually more familiar with the open technique. Each technique has its persuasive advocates basing their arguments on a combination of scientific evidence and personal bias. Methods of port entry were examined by a recent Cochrane review which concluded that there was no evidence that one method was superior (Ahmad et al 2008).
Site of entry
At the umbilicus, the abdominal wall is at its thinnest. A subumbilical incision is preferred by some clinicians, but there appears to be no logic to this. If the umbilicus is to be used, there is little point in inserting either the Veress needle or primary trocar at a point where the abdominal wall has expanded. In addition, an intraumbilical incision is cosmetically superior (Figure 3.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree