Fig. 16.1
Suturing mesh to vaginal apex

Fig. 16.2
Opening peritoneum over the sacral promontory
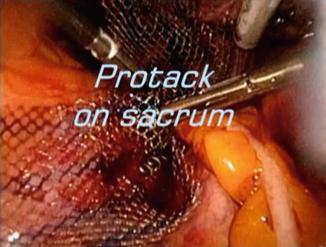
Fig. 16.3
Fastening the mesh to the sacral promontory with tacks
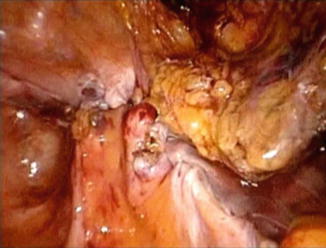
Fig. 16.4
End of the procedure with mesh covered by peritoneum
16.4 Urinary Tract Considerations
Cystoscopy should be routinely performed in pelvic organ prolapse repair surgery to ensure excellent ureteral flow at the end of surgery. However, cystoscopy is not a perfect indicator of bladder injury; a reassuring cystoscopy does not guarantee the absence of bladder injury, especially in the case of thermal injury. The possibility of injury must not be ruled out if symptoms present postoperatively. Isolation of the ureters prior to initiating any energy sources as well as maintaining direct visualization throughout the procedure are key factors in avoiding bladder injury (Jabs and Drutz 2001).
16.5 Postoperative Management
Postoperatively, the majority of patients have an uneventful recovery. Following laparoscopic prolapse repair, patients receive nonsteroidal anti-inflammatory medications along with narcotics by mouth as needed. They are generally ready for discharge the following morning. A vaginal pack may be placed over night and a Foley catheter left in place until the following morning. It is good practice to perform a voiding trial the morning after surgery prior to discharge as there is a small risk of urinary retention in these patients. It is important to remain vigilant for possible urinary tract injuries and mesh-related complications. Complications resulting from mesh use may present as fever, infection, dyspareunia, and chronic bloody vaginal discharge, and exposed mesh may be visible if erosion has taken place.
16.6 Conclusions
Laparoscopic treatment of pelvic organ prolapse is a viable option for patients desiring minimally invasive surgical management of their symptoms while also achieving optimal long-term results. More research is needed to better determine the surgical procedures and techniques of choice for various clinical scenarios.
References
Bensinger G, Lind L, Lesser M et al (2005) Abdominal sacral suspensions: analysis of complications using permanent mesh. Am J Obstet Gynecol 193(6):2094–2098
Committee on Gynecologic Practice (2011) Committee opinion no. 513: vaginal placement of synthetic mesh for pelvic organ prolapse. Obstet Gynecol 118(6):1459–1464CrossRef
Ehsani N, Ghafar MA, Antosh DD et al (2012) Risk factors for mesh extrusion after prolapse surgery: a case-control study. Female Pelvic Med Reconstr Surg 18(6):357–361
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


