CHAPTER 26 Laparoscopic and Open Pyloromyotomy
Step 1: Surgical Anatomy
♦ The pylorus is identified as a smooth muscle mass that normally measures 1 to 1.5 cm in diameter and 2 to 2.5 cm in length. When hypertrophic pyloric stenosis (HPS) is present, the musculature becomes enlarged, measuring up to 4 cm in length and 3 cm in diameter.
♦ As its name implies, in the presence of HPS, the pyloric musculature is hypertrophied without accompanying hyperplasia. There is an obvious demarcation between the distal aspect of the abnormal pylorus musculature and the normal thin-walled duodenum. The hypertrophied pylorus leads to protrusion of the muscle and mucosa into the distal duodenum, and care must be taken to not injure the duodenal mucosa at its transition at the time of pyloromyotomy.
Step 2: Preoperative Considerations
Presentation and Metabolic Abnormalities
♦ Infants with HPS are a remarkably homogeneous population. They are usually between 3 weeks and 3 months of age with a history of at least 2 weeks of nonbilious emesis. The emesis pattern associated with HPS is unique and is an important part of the history. Vomiting is postprandial and projectile, often described as “shooting across the room.” This forceful vomiting is due to the aggressive contractions of the gastric musculature in an attempt to push the gastric contents through the obstructed pylorus. Despite the vomiting, the infant remains hungry and will feed again almost immediately if allowed, only to vomit again. Often the family will have undertaken several changes in formula feeds at the recommendation of the pediatrician or primary care physician after a diagnosis of milk allergy or formula intolerance.
♦ At presentation, the infant can be below his or her birth weight as a result of progressive malnutrition and dehydration. Prolonged emesis results in loss of gastric secretions and severe dehydration, leading to the development of hypokalemic, hypochloremic metabolic alkalosis that can progress to paradoxical aciduria as a result of the renal response to volume contraction and increasing alkalosis. The kidneys attempt to expand intravascular volume, rather than correct the abnormal pH, by absorbing sodium and excreting a hydrogen ion from the hypokalemia. This proton excretion is what leads to the paradoxical aciduria.
Diagnosis
♦ Palpation of the abdomen in an infant with HPS reveals an enlarged pylorus classically described as an “olive” deformity located over the epigastrium. The pylorus is mobile in its superior-inferior direction and is more easily palpated with the stomach empty (after emesis).
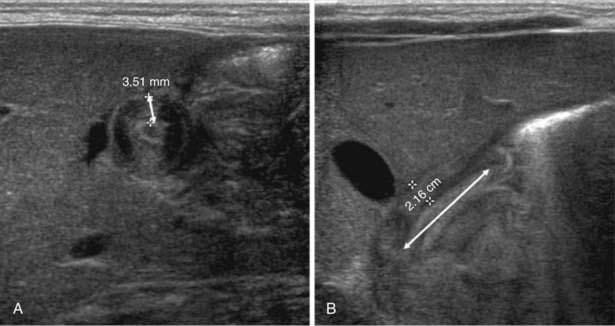
♦ A small amount of sugar water on a pacifier or bottle nipple will usually allow several minutes of diminished agitation, thereby allowing a careful and accurate examination. Although this examination is described in what seems to be a straightforward and efficient manner, it is time consuming and difficult to perform by individuals not experienced in the technique. In our experience, nearly all patients routinely have undergone an abdominal ultrasound before surgical consultation, and we strongly feel that in this setting this is a more efficient diagnostic modality compared with a physical examination alone. Generally accepted guidelines for the diagnosis of HPS by ultrasound include a tumor depth of 4 mm and a pyloric channel length of at least 16 mm (Fig. 26-1).
♦ Although we do not recommend their use as a diagnostic modality today, upper gastrointestinal contrast studies have been utilized in the past. When performed in an infant with HPS, the stomach will appear distended and there will be delay in gastric emptying. Gastroesophageal reflux may be detected during this study, which is the result of the gastric outlet obstruction created by the hypertrophied pylorus. An elongated and narrowed line of contrast, classically described as a “string sign,” will identify the hypertrophied pyloric channel.
Preoperative Resuscitation and Preparation
♦ The preoperative resuscitation and preparation of a patient with HPS are paramount to any surgical procedure. As outlined, infants with HPS are usually dehydrated and malnourished and can have severe electrolyte abnormalities (hypokalemia, hypochloremia, and alkalosis).
♦ All patients should be admitted to the hospital and have an intravenous catheter inserted and a basic chemistry profile obtained. Fluid resuscitation should begin with an initial fluid bolus of 10 to 20 mL/kg of normal saline, after which the bolus resuscitation can be determined by the clinical state of the infant (urine output, skin turgor, mucous membranes, normalization of serum electrolytes). Maintenance fluids should be continued at a volume of 1.5 times the hourly maintenance rate of D5 1/2 normal saline. Then 20 meq KCl/L should be added after urine output has been established. Only after patients have been adequately resuscitated and have normal serum electrolytes can they be considered for operative correction. In our institution, we use a serum chloride of greater than 90 mEq/dL and a serum bicarbonate of less than 30 mEq/dL as safe electrolyte levels for general anesthesia in HPS patients.
♦ Preoperative anesthetic concerns must also be addressed. Before any progression toward anesthetic induction, the stomach is emptied with several passes of an orogastric tube connected to suction in remove any gastric contents that are retained in the obstructed stomach. Anesthesia is induced in a rapid sequence manner with great care taken to protect the airway from aspiration of gastric contents. Gentle cricoid pressure can be applied to assist in occluding the esophagus, thus decreasing the aspiration risk during the induction and intubation portion of the anesthetic.