Testing Modalities (Obstet Gynecol 2009;113:687)
• Fetal mvmt count (“kick count”) (Cochrane Database Syst Rev 2007:CD004909)
Variable protocols, usually 2 h, 3–7× per week
10 mvmts → reassuring; insuff evid to recommend this method of surveillance
• Nonstress test
Continuous fetal heart monitoring × 20–40 min
At least 2 15 bpm × 15 s accelerations (or 10 × 10 at <32 w) → reassuring
Occasional, brief variable decelerations do not affect negative predictive value
Performance for prediction of stillbirth w/i 1 w: Sens 99.7%, spec 45%
• Biophysical profile (From US exam of fetus up to 30 min)
Elements (2 points each if nml/reassuring):
Continuous fetal breathing, 1 episode >30 s
3+ fetal limb or body mvmt
1+ episodes of flexion/extension of a limb or hand
2 × 2 cm or greater pocket of amniotic fluid (or amniotic fluid index >5 cm)
Reactive nonstress test
<6/10 = abn (consider deliv); 6/10 = equivocal (rpt in 6–24 h); >6/10 = reassuring. Prediction of stillbirth w/i 1 w: Sens 99.92%, spec 50%.
• Contraction stress test (oxytocin or nipple stimulation to produce 3 contractions in 10 min of >40 s, w/ continuous FHR monitoring)
Negative = No late or signif variable decelerations
Positive = Late decelerations w/ >50% of contractions
Equivocal = Anything btw “negative” & “positive”
Unsatisfactory = Uninterpretable fetal heart tracing or insuff contraction frequency
Prediction of stillbirth w/i 1 w: Sens 99.96%, PPV 70%
• Umbilical artery Doppler velocimetry (US measurement, only indicated in fetuses w/ growth restriction)
Low resistance system should allow forward flow throughout cardiac cycle
Absent or reverse end-diastolic flow is a/w increased perinatal mortality (5× greater w/ reversed flow) (Lancet 1994;344:1664)
• Middle cerebral artery Doppler velocimetry
US measurement of peak systolic velocity, indicated if concern for fetal anemia
Velocity >1.5 MoM has sens for mod/sev anemia 100%, spec 88% (N Engl J Med 2000;342:9). Optimal screening interval likely 1–2 w
FETAL LUNG MATURITY TESTING BY AMNIOCENTESIS
General Considerations
• Consider testing for planned deliv btw 32 & 39 w
• Before 32 w low likelihood of maturity
• Test performance worsens at earlier GAs
• All tests more accurately predict absence of respiratory distress (w/ mature result) than predict respiratory distress (w/ immature result) (Obstet Gynecol 2001;97:305)
Specific Assays
• Lamellar body count (direct assessment) or optical density at 650 nm (indirect assessment)
>50000/μL or optical density (OD) >0.15 sugg maturity. May vary by institution.
• L/S ratio (L/S about equal till ∼35 w, then lecithin increases)
Threshold value for “mature” varies by institution. Generally mature at >2 (2–3.5)
• PG measurement (appears ∼35 w & rapidly increases)
Quantitative or qualitative measurement. Not affected by mec or bld.
• Foam stability index. Measures functional surfactant. >47 signifies maturity.
• Surfactant/albumin ratio, TDx-FLM II (phased out by manufacturer in 2011)
NEWBORN RESPIRATORY DISTRESS
Epidemiology (Am Fam Physician 2007;76:987)
• 7% of infants. Most common causes: Transient tachypnea of the newborn, respiratory distress syn, mec aspiration syn.
• Less common causes: Delayed transition, infxn, persistent pHTN, PTX, nonpulmonary causes (anemia, CHD)
Signs and Symptoms
• Tachypnea (>60 breaths/min), nasal flaring, poor feeding, grunting, sub- or intracostal retractions, insp stridor, apnea, cyanosis
Transient Tachypnea of the Newborn
• >40% of cases of respiratory distress
• Inadeq fluid clearance from lung → decreased pulm compliance → tachypnea
• Onset w/i 2 h of birth; usually resolves in <72 h
• CXR: Diffuse parenchymal infiltrates
Respiratory Distress Syndrome (Hyaline Membrane Disease)
• Affects 24000 infants in US annually
Most common before 28 w gest
1/3 of infants 28–34 w gest
<5% of infants after 34 w gest
• Surfactant deficiency causing atelectasis & V/Q mismatching → hypoxemia
• Incid ↑ for newborns of diabetic moms
• CXR: Homogenous, opaque infiltrates, & air bronchograms
Meconium Aspiration Syndrome
• Mec-stained amniotic fluid = 15% of deliveries → 10–15% of those get mec aspiration syn; mec = irritative, obstructive, medium for bact culture
• Usually term or postterm infants; signif respiratory distress immediately after deliv
• CXR: Patchy atelectasis or consolidation
General Management
• Diagnostic CXR; CBC, bld gas, bld cx
• Supplemental oxygen therapy, w/ assisted ventilation if necessary
• Supportive care w/ fluid/electrolyte mgmt & neutral thermal environment
Oral feeding often withheld w/ respiratory rate >80 breaths/min
• Empiric ampicillin & gentamicin if risk factors for sepsis or refrac/persistent sx
• Surfactant administration may be req
GROUP B STREPTOCOCCAL DISEASE
Definition and Epidemiology (MMWR 59(RR10):1)
• Intrapartum vertical transmission of GBS is the leading cause of infectious morbidity/mortality in neonates; incid is ∼0.35/1000 births
• Caused by GBS infxn of fetal mucosal surfaces by GBS in amniotic fluid or birth canal
• 10–30% of pregnant women are colonized w/ GBS in GI tract or vagina
• Risk factors for invasive perinatal dz include:
<37 w at deliv
Ruptured amniotic membranes for >12 h
Intra-amniotic infxn
Young mat age
Black race
Low levels of anti-GBS Ab
Clinical Manifestations
• Sepsis, PNA, & meningitis in the 1st w of life
• Fatal in 2–3% full-term infants & 20–30% of preterm newborns <33 w GA
Screening and Diagnosis
• Pregnant women should routinely be screened by rectovaginal swab at 35–37 w. Culture results are valid for up to 5 w, then should be repeated at >5 w.
• NAAT for GBS is currently only indicated in women w/ (1) culture data unk, (2) at term, & (3) w/o prolonged rupture of membranes or fever
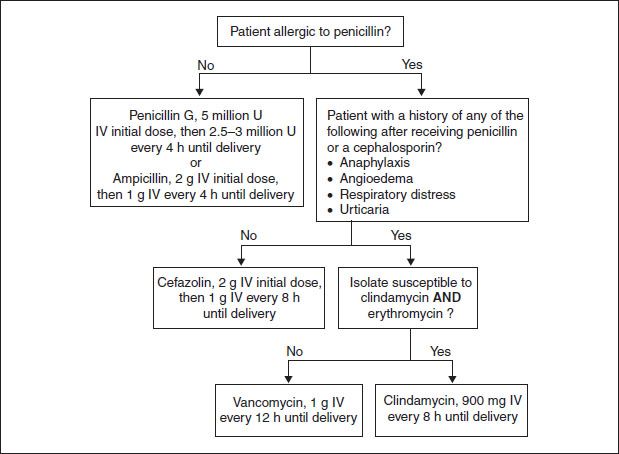
Treatment
• Intrapartum Abx indicated for:
Positive rectovaginal culture during this Preg
GBS bacteriuria at any time during this Preg (exempt from routine screening)
H/o perinatal GBS dz in a prior Preg (exempt from routine screening)
Culture data unavailable & <37 w OR term w/ rupture of membranes >18 h or temperature >100.4°F
• Intrapartum ppx NOT indicated at the time of cesarean deliv at any GA for women delivered prior to labor w/ intact membranes
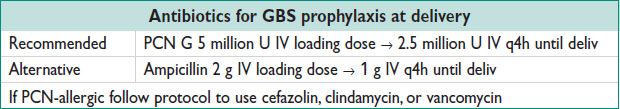
Figure 10.1 Intrapartum prophylaxis for GBS disease
SPONTANEOUS LABOR AND DELIVERY
Definitions
• Labor: Regular uterine contractions & cervical change
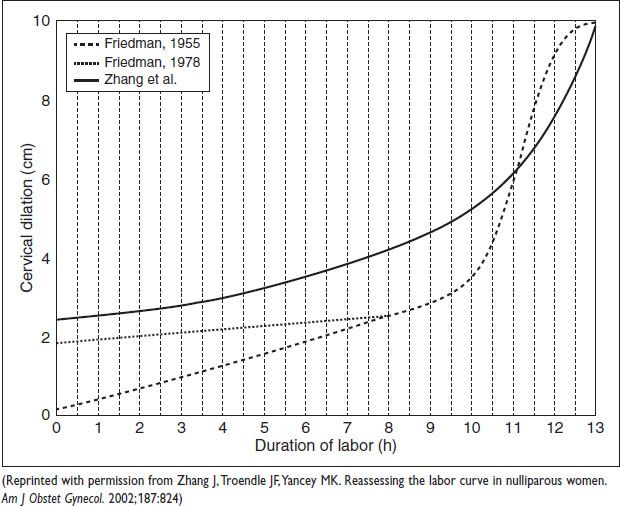
• 1st stage of labor: Onset of labor → full cervical dilation
Latent phase: Early labor until acceleration of rate of cervical change
Active phase: Period of accelerated cervical change until full dilation
Historically, minimum rate of cervical change: Nulliparas ∼1.2 cm/h, multiparas, ∼1.5 cm/h (N Y Acad Med 1972;48:842)
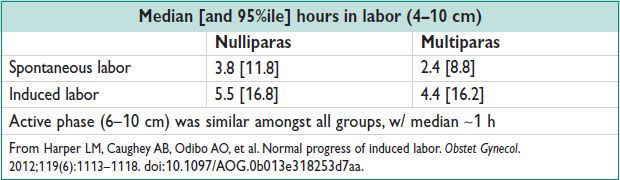
Labor curve: Friedman (1955) described ideal labor progress at term; Zhang (2002) showed women enter active phase at 3–5 cm, w/ variable labor course & no deceleration phase
• 2nd stage of labor: Full cervical dilation → deliv of the infant
Consider 2nd stage arrest in nulliparas after 2 h (no epidural) or 3 h (w/ epidural), or in multiparas after 1 h (no epidural) or 2 h (w/ epidural)
• 3rd stage of labor: Deliv of the infant → deliv of the placenta
• 4th stage of labor: 1–2 h immediately following deliv of the placenta
• Cervical assessment: Cervical dilation is measured in cm. Cervical effacement is documented as percentage of full length (4 cm) cervix lost (0% is full length & 100% is paper thin), or as cm of length. Fetal station is descent of the bony fetal presenting part in centimeters above or below the mat ischial spine (−5–+5 cm scale).
• Fetal position: Orientation of the presenting part relative to the mat pelvis
Cephalic presentation w/ occiput documented on mat left/right, rotated post/anter/transverse (eg, ROA). The sacrum may be used for fetuses in breech presentation, the acromion for transverse lie, the mentum for face presentations
Figure 10.2 Labor curves
Cardinal Movements of Labor
• Engagement: Passage of widest diameter of presenting part below pelvic brim
• Descent: Passage of presenting part downward into pelvis
• Flexion: Allows optimal descent by presenting smallest cranial diameter
• Internal rotation: Mvmt of the fetal head from transverse to anteroposterior
• Extension: Mvmt of the fetal head under the pubic symphysis & out the introitus
• External rotation (“restitution”): Mvmt of the head to align w/ torso
• Expulsion: Deliv of the fetal body
Management of Labor
• Physical exam on presentation: Mat VS; cervical dilation, effacement, fetal station, rupture of membranes (± mec), presence of vaginal bleeding, & estimated fetal weight (by Leopold’s)
Fetal heart assessment (intermittent in low-risk, or continuous in high-risk pts) & uterine tocometry to assess fetal status & contractions
• Consider CBC, bld type & screen, urinalysis
• IV access, avoid solid foods (Obstet Gynecol 2009;114:714)
• Walking & upright positioning in early labor may ↓ the 1st stage by 1 h (Cochrane Database Syst Rev 2009,2:CD003934)
• Assess desire for pain control, w/ or w/o regional anesthesia
• GBS ppx if indicated
Management of Delivery
• Pushing may begin w/ full cervical dilation or be delayed until presenting part descends (“laboring down”); pushing generally accompanies contractions. Delayed pushing ↑ length of the 2nd stage by ∼1 h, but ↓ the need for instrumented deliveries (but not cesarean deliveries) (J Obstet Gynecol Neonatal Nurs 2008;37:4). Pushing should not be delayed if there is an indication to expedite deliv (eg, infxn).
• No indication for routine episiotomy. If necessary, midline a/w ↓ bld loss & ↑ anal sphincter injury compared to mediolateral.
• Warm compresses to the perineum may ↓ incid of 3rd/4th-degree lacerations (Cochrane Database Syst Rev 2011;12:CD006672)
• In women w/o epidural anesthesia, pushing while upright was a/w ↑ risk of EBL >500 cc & ↓ abn FHTs w/o signif impact on length of 2nd stage (Cochrane Database Syst Rev 2012;5:CD002006)
• Deliv of the fetal head:
Care should be taken to control speed of deliv & to protect the anter vaginal wall, urethra, & clitoris
The perineum should be eased over the fetal head
The head should be allowed to restitute
Gentle downward traction of the head to deliver the anter shoulder (difficulty w/ this maneuver should prompt consideration of shoulder dystocia)
The body should be delivered w/ gentle upward traction, supporting the perineum as poss
• The cord should be clamped & cut → delayed cord clamping ↓ risk of fetal/neonat anemia, but ↑ need for phototherapy (Cochrane Database Syst Rev 2008:CD004074; BMJ 2011;343:d7157). Delaying cord clamping by 45 s in premature infants <37 w may ↓ risk of IVH & neonat xfusion (Cochrane Database Syst Rev 2004;4:CD003248)
• Active mgmt of 3rd stage w/ suprapubic pres & controlled cord traction may ↓ mat hemorrhage (Cochrane Database Syst Rev 2011;11:CD007412)
• Consider deliv onto mat abd to promote immediate breastfeeding & bonding (Cochrane Database Syst Rev 2012;5:CD003519)
• Give oxytocin in the 3rd stage to ↓ postpartum hemorrhage (Cochrane Database Syst Rev 2001;(4):CD001808)
• Inspect the placenta to identify anomalies & to ensure intact disc
• Fetal cord bld gas analysis & postpartum hemorrhage (see sections below)
INDUCTION OF LABOR (IOL)
Definition and Epidemiology
• Stimulation of uterine contractions w/ intent to cause vaginal deliv prior to spontaneous onset of labor
• 23.2% of births in 2009 were after IOL (National Vital Statistics Report, 2011)
• “CR” is the softening, thinning, & dilating to facilitate successful IOL
Indications
• Risks (to mother or fetus) of continuing Preg outweigh the risks a/w effecting deliv, & no contraindication to vaginal birth
• Labor should not be electively induced prior to 39 w gest due to significantly elevated neonat morbidity
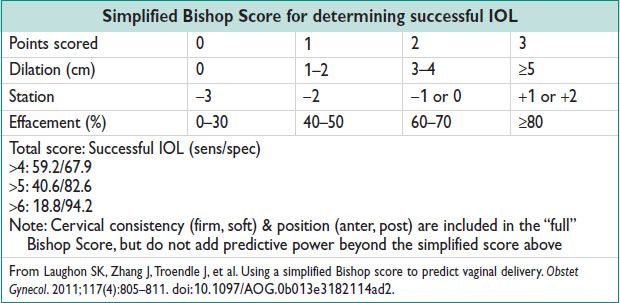
• Overall, multiparas are less likely than primiparas to fail induction or require cesarean deliv at a given Bishop Score
Methods of Cervical Ripening & Induction of Labor
• Oxytocin – most commonly used induction agent
Various dosing regimens; titrate to contractions q2–3min
Low-dose regimen (start 0.5–2 mU/min w/ 1–2 mU/min ↑ q15–40min)
High-dose regimen (start 6 mU/min w/ 3–6 mU/min ↑ q15–40min)
Note: High-dose regimen decreases time to deliv, but increases rate of tachysystole w/ FHR changes (Cochrane Database Syst Rev 2012;3:CD001233)
• Misoprostol (PGE1) – for CR or IOL
Oral misoprostol superior to vaginal misoprostol for CR/IOL (fewer 5-min Apgars <7)
Dosage 25 mcg PO q2h or 50 mcg PO q4h (Cochrane Database Syst Rev 2006;(2):CD001338)
Vaginal misoprostol may be used for CR/IOL at dose of 25 mcg PV q3–6h
Contraindicated if h/o uterine Surg (including prior cesarean) given elevated risk of uterine rupture
• Dinoprostone (PGE2) – for CR or IOL
Each insert contains 10 mg of dinoprostone → releases mean dose of 0.3 mg/h
Dosed q12h
Upon removal of insert, quickly eliminated from mat circulation
• Amniotomy alone (Cochrane Database Syst Rev 2000;(4):CD002862)
Insuff evid regarding efficacy
↑ need for oxytocin augmentation vs. vaginal prostaglandin
• Balloon catheter (Cochrane Database Syst Rev 2012;3:CD001233) – for CR or IOL
Placement of balloon catheter w/ 30–60 cc of saline through internal os into extra-amniotic space
↓ efficacy for multiparous women & ↓ risk of tachysystole compared w/ prostaglandin
• Membrane stripping (Cochrane Database Syst Rev 2005;(1):CD000451)
Manual detachment of inferior pole of fetal membranes during vaginal exam
• Sexual intercourse: Insuff evid. Likely ineffective (Obstet Gynecol 2007;110(4):820–826; Cochrane Database Syst Rev 2001;(2):CD003093).
• Breast stimulation: Decreased postpartum hemorrhage compared to no intervention. No difference in rates of cesarean when compared to no intervention or oxytocin. Not effective in women w/ unfavorable cervix (Cochrane Database Syst Rev 2005;(3):CD003392).
Complications of Induction
• Tachysystole (greater than 5 contractions in 10 min). Rx: Stop/↓ uterine stimulation, consider tocolysis
• Uterine tetany (contraction lasting greater than 2 min). Rx: Stop/↓ uterine stimulation, consider tocolysis
• Cord prolapse (w/ amniotomy). Rx: Cesarean deliv.
• HoNa (w/ extended infusion of oxytocin). Rx: Stop oxytocin infusion, consider free water restriction, recheck, & resume.
• Cesarean deliv ↑ compared to spontaneous labor, but elective IOL at 41+ w, compared w/ expectant mgmt may ↓ c-section (Cochrane Database Syst Rev 2012;6:CD004945)
INTRAPARTUM FETAL MONITORING
Background
• Justification for intrapartum FHR monitoring based on expert opinion & medicolegal precedent
• Continuous FHR monitoring a/w (1) reduction in neonat seizures, w/o significant differences in cerebral palsy, infant mortality or other std measures of neonat well-being; & (2) ↑ in cesarean deliv & instrumental vaginal births when compared to intermittent auscultation or no monitoring (Cochrane Database Syst Rev 2006;3:CD006066)
Methods of Monitoring
• FHR: External via Doppler US -or- internal via fetal scalp electrode
• Contractions:
External pres transducer (qualitative)
Intrauterine pres catheter (quantitative). Measurement in MVU: Add up peak minus baseline uterine pres for each contraction over 10 min; >200 MVU considered adequate for labor (Obstet Gynecol 1986;68:305).
Definitions (Obstet Gynecol 2008;112:661)
• Baseline: Avg FHR, exclusive of accelerations, decelerations, & marked variability, taken over a 10-min interval, rounded to nearest 5 bpm
Tachy: Baseline > 160 bpm
Brady: Baseline < 110 bpm
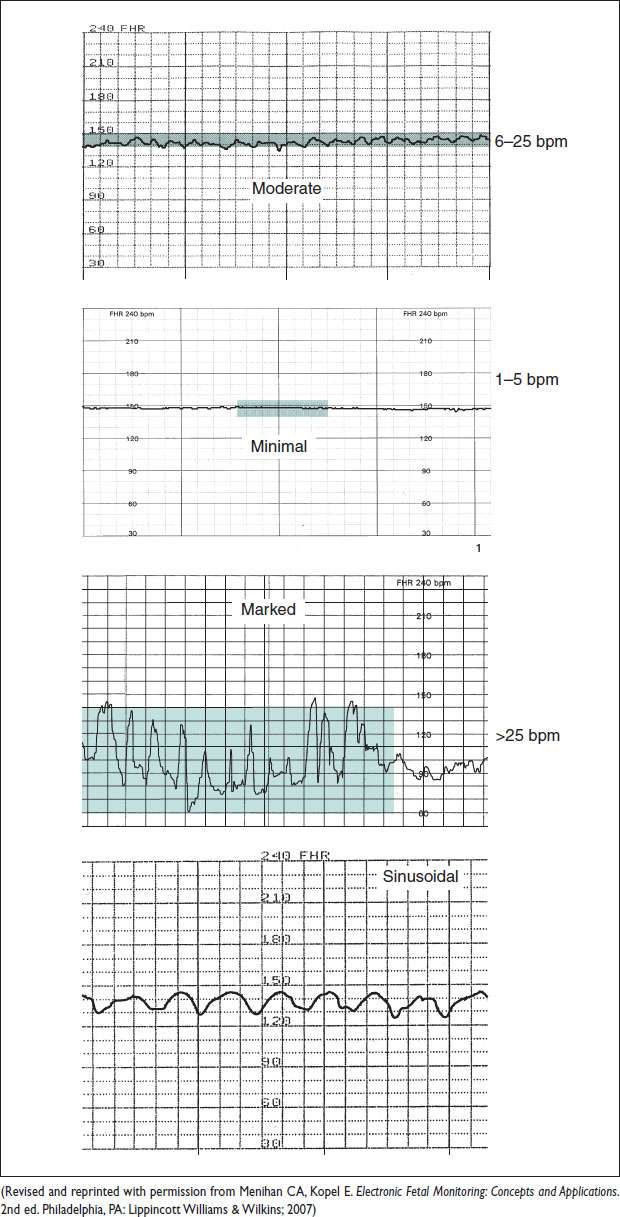
• Variability: Beat-to-beat fluctuations in the baseline FHR, exclusive of accelerations & decelerations. Measured from peak to trough of rapid fluctuations.
Absent: Amplitude undetectable
Minimal: Amplitude btw 1 & 5 bpm
Mod: Amplitude btw 6 & 25 bpm
Marked: Amplitude > 25 bpm
• Accelerations: Increased FHR ≥15 bpm for ≥15 s (before 32 w, use ≥10 bpm & ≥10 s). Time from baseline to peak HR is <30 s. Prolonged acceleration lasts 2–10 min.
• Decelerations: ↓ in FHR
Early deceleration: Nadir w/ peak of contraction. Baseline to nadir takes >30 s.
Late deceleration: Nadir after peak of contraction. Baseline to nadir >30 s.
Variable deceleration: ↓ ≥15 bpm from baseline lasting at least 15 s. Baseline to nadir <30 s.
Prolonged deceleration lasts 2–10 min
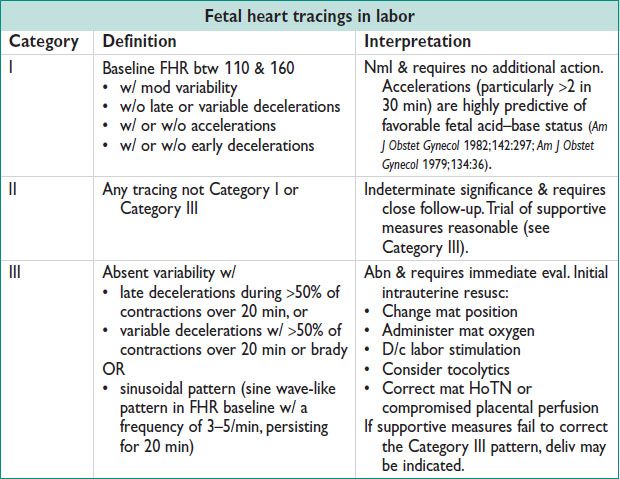
Sample Fetal Heart Tracings
Figure 10.3 Fetal heart rate variability