27 Juvenile Dermatomyositis
Clinical Presentation
Cutaneous Features
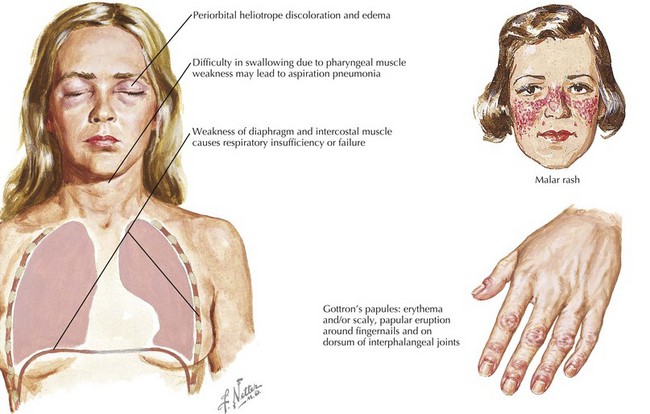
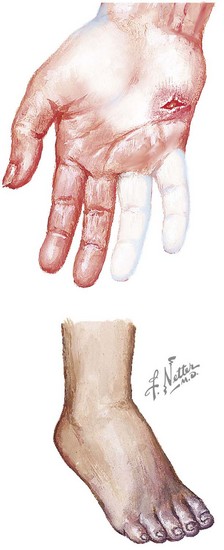
Dermatomyositis has several classic cutaneous findings (Figure 27-1). Gottron’s papules are erythematous, raised, scaling plaques on the dorsal surface of the knuckles, elbows, and knees that are present in more than 90% of children at the time of diagnosis. Gottron’s papules are frequently confused with severe eczema if JDMS is not suspected. The classic heliotrope rash is a violaceous discoloration of the eyelids with associated eyelid edema; this is present in approximately 80% of children at diagnosis. About 40% of children also have a prominent erythematous malar rash. This rash can be ulcerative, cross the nasolabial folds, and extend onto the forehead. Raynaud’s phenomenon (Figure 27-2) and associated nailfold capillary changes are seen in up to 80% of patients. Nailfold changes are characterized by proximal nailfold erythema, capillary dilatation, tortuosity, or dropout. The measured density of capillaries per millimeter may be a useful tool for monitoring clinical activity. Skin ulcerations reflect significant vasculopathy of the skin and may be a sign of internal organ vasculopathy. Ulcerative skin lesions are associated with more severe disease and worse prognosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree