11 Interdisciplinary Education and Training
Principles of Adult Education
These attributes lead to highly pragmatic learners who are likely to be motivated when the material is relevant. They are able to be critical about the value of what they learn. When adult learners feel respected by the teachers, they can actively test what they learn in the real world, integrating new learning into their professional roles1 (Box 11-1).
Principles of Interdisciplinary Education
The World Health Organization (WHO) says “Interaction is the important goal, to collaborate in providing preventive, curative, rehabilitative, and other health-related services”2 regarding interdisciplinary education. Other goals include “enhancing” or “improving” both collaboration and quality of care3 (Table 11-1).
TABLE 11-1 Core Competencies for Every Clinician
| Institute of Medicine—IOM11 | Interprofessional Education Consortium—IPEC12 |
|---|---|
| Provide patient-centered care | Family-centered practice |
| Work in interdisciplinary teams Employ evidence-based practice Apply quality improvement Use informatics | Integrated services through collaboration and/or group process |
| Assessment and outcome | |
| Social policy issues | |
| Communication | |
| Leadership |
There is a mantra in palliative care circles that interdisciplinary teamwork and learning are beneficial. However, the supporting research and literature is limited, and where available, remains controversial. A review of the general and academic literature on interdisciplinary education identifies some of the salient qualities, benefits, and challenges4 (Table 11-2).
TABLE 11-2 Interdisciplinary Education: Benefits and Challenges
| Benefits | Challenges and/or disadvantages |
|---|---|
The Pedagogy of Pediatric Palliative Care
Unique dynamics of pediatric palliative care
Core Curriculum
Although communication is listed equally among the components below, enhanced communication with patients, families, and colleagues is a priority and an intrinsic part of all the topics. Pediatric residents wished for “aspects of communication” as 4/5 of their top choices for additional education.5 Core educational components include:
Team interdisciplinary education and training
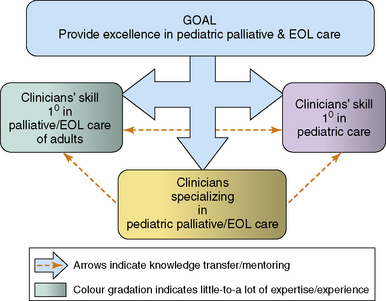
A dynamic mix of clinicians, from different disciplines and with varied skills, requires training in pediatric palliative care (Fig. 11-1).
Interdisciplinary groups provide an opportunity to share information from each individual and discipline’s perspective. Because each discipline has unique educational preparation, philosophy, and standard of practice, a common forum lends a richness and diversity to the group’s knowledge. Furthermore, it fosters respect and appreciation for each individual’s contribution. Research suggests that the earlier students from different disciplines are paired, the better their perceived understanding of roles.16 Medical student participants shared what they perceived as institutional support or the lack thereof in interprofessional interventions.17 Both within and outside the formal teaching session, the frequent and ongoing modeling of interdisciplinary practice must be considered in curricula implementation.18,19 The evaluation of these initiatives is also crucial because trainees’ perceptions of the importance of educational material is strongly linked to such data.20
Emerging research identifies the educational needs of the support staff on the pediatric palliative care team. A recent study pointed out that professional, educational, and emotional needs were notably unmet in this heterogeneous community of care providers. Although they had significant and direct contact with dying children and their families, none of them had received training in coping strategies and grief.21
Informal focus groups of trainees in pediatric palliative care rated respect of one another’s disciplines as the most important outcome of an interdisciplinary educational initiative.13 An integral component described by Health Canada is the development of mutual understanding for the contributions of various disciplines.18 In this emotionally difficult field, such respect may help prevent and reduce staff distress, communication obstacles, and conflict. Furthermore, the sharing of experiences and perceptions across disciplines leads to the recognition of universal reactions and emotions. An Australian interdisciplinary education palliative care model involved 537 participants, whose feedback requested more group sharing.22 Pediatric hematology-oncology and critical-care physicians noted that observing senior physicians in difficult conversations with families was the most helpful aspect of their palliative care training.14 It bodes well for interdisciplinary education that respondents also requested that team members from disciplines other than medicine be involved in teaching of communication skills.
Setting the stage for a level playing field within the group is essential within interdisiplinary education. For example, although nurses are often the most numerous of the participants, their input may be dismissed if there is a real or imagined power differential between them and the physicians present. On the other hand, the number of nurses may intimidate individuals from less well-represented disciplines. A study evaluating interdisciplinary workshops found that male participants and physicians tended to take over in role play and discussion formats.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree