110 Inflammatory Bowel Disease
Clinical Presentation
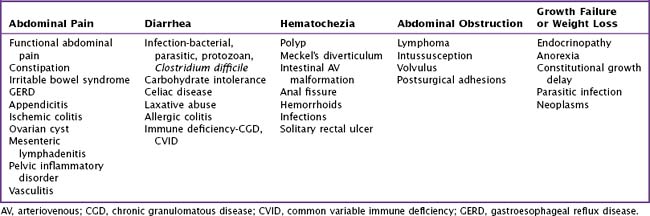
The differential diagnosis for IBD is extensive and largely depends on the presenting symptoms (Table 110-1).
Crohn’s Disease
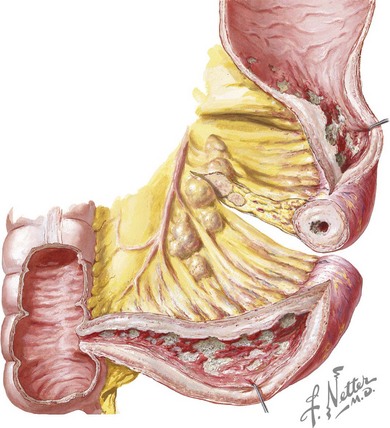
Crohn’s disease is characterized by transmural inflammation that may involve any segment of the intestinal tract from the mouth to the anus. Disease presentation is primarily determined by the location and extent of involvement. In children, the most common presenting distribution is ileocolonic disease (Figure 110-1) followed by small bowel disease alone and then colonic disease alone. Gastroduodenal disease is found in 30% of children with Crohn’s disease. Patients with ileocecal disease often present with right lower quadrant abdominal pain and diarrhea. In such patients, loops of bowel or fullness may be palpable in the right lower quadrant. Bloody stool is more common in colonic disease. Epigastric pain may occur with gastroduodenal disease. Dysphagia can be seen with esophageal involvement. Many children with Crohn’s disease have diarrhea, nocturnal defecation, low-grade intermittent fever, oral ulcers, weight loss, and decelerated growth velocity.
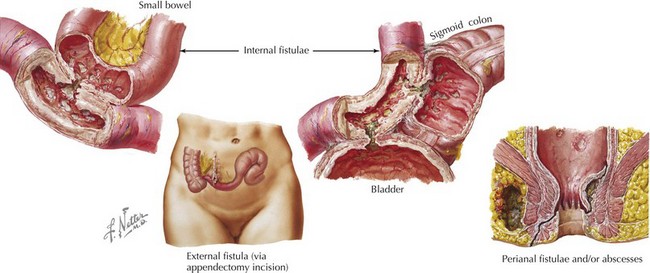
Crohn’s disease is categorized into three subtypes: inflammatory, stricturing, and fistulizing. Inflammatory disease is that described above. Stricturing disease involves luminal narrowing, which may be accompanied by prestenotic dilatation or signs of intestinal obstruction. This most commonly occurs in the small bowel but may involve the colon. Perianal or perirectal fistulae and abscesses or intraabdominal fistulae, phlegmon, or abscesses characterize fistulizing disease (Figure 110-2).
Extraintestinal Manifestations
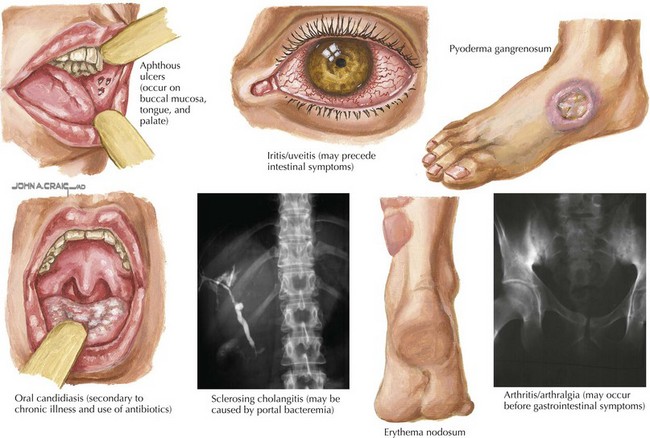
About a third of patients with IBD also have extraintestinal manifestations involving rheumatologic, cutaneous, ocular, vascular, hepatobiliary, renal, and skeletal systems (Figure 110-3). Arthralgia and arthritis are the most common extraintestinal symptoms and may involve both axial and peripheral joints. Joint manifestations may precede GI tract disease, so IBD should be in the differential diagnosis of isolated arthralgia or arthritis. Juvenile rheumatoid arthritis and ankylosing spondylitis are associated with IBD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree