Chapter 17 Infertility
Infertility
Causes of female factor infertility
With increasing age, women become less fertile.
| Unexplained infertility | 28% |
| Male factor infertility | 21% |
| Ovulatory disorders | 18% |
| Tubal disease | 14% |
| Endometriosis | 6% |
| Coital problems | 5% |
| Cervical factors | 3% |
Investigations
Investigations in the primary setting
| Female partner | Cervical smear test. |
| Urine test for Chlamydia (this can cause blockages of the fallopian tube). | |
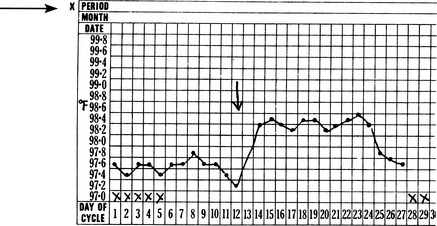
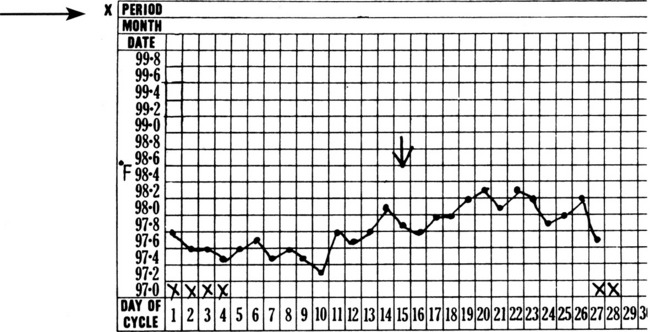
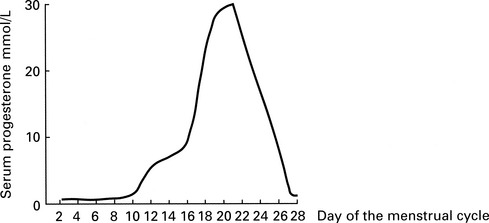
| Serum progesterone level to check ovulation. This is taken 1 week prior to menstruation, hence day 21 for a 28-day cycle or day 28 for a 35-day cycle (see below). | |
| Rubella immunity – if rubella is contracted during the first 3 months of pregnancy it can seriously harm the developing fetus Women who are not immune to rubella should be vaccinated, and advised to avoid pregnancy for 3 months. | |
| Measuring serum FSH (follicle stimulating hormone), LH (luteinising hormone) and oestradiol to identify hormone imbalances or possible early menopause. | |
| Male partner | Semenalysis to check for abnormalities of the sperm such as number, motility, and morphology (see below). |
| Urine test for Chlamydia, which, in addition to being a known cause of infertility in women, can also affect sperm function and male fertility. |
Investigations in the secondary setting
| Female partner | Measuring serum FSH, LH and oestradiol to identify hormone imbalances or possible early menopause. |
| Serum progesterone level to check ovulation. This is taken 1 week prior to menstruation, hence day 21 for a 28-day cycle or day 28 for a 35-day cycle. | |
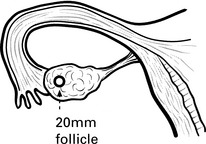
| A pelvic ultrasound scan to look at uterine and ovarian anatomy. | |
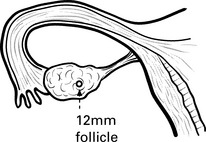
| Serial ultrasound tracking of the ovaries for looking at developing follicles (see below). | |
| Checking of tubal patency – either by hysterosalpingogram, hysteron-contrast sonography or laparoscopic hydrotubation. | |
| Diagnostic laparoscopy – to check for problems with tubal and uterine anatomy. | |
| Hysteroscopy – to check for uterine conditions such as fibroids or polyps | |
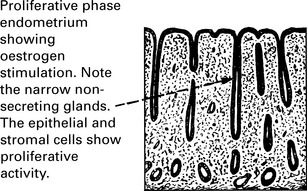
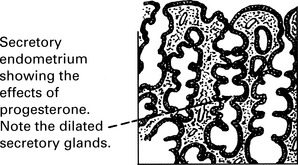
| Endometrial biopsy (in rare cases) see below. | |
| Male partner | Semenalysis to check for abnormalities of the sperm such as number, motility and morphology (see below). |
| Sperm antibody test to check for protein molecules that may prevent sperm from fertilising an egg. |