Indications
Induction is indicated when the benefits to either mother or fetus outweigh those of pregnancy continuation. The more common indications include membrane rupture without labor, gestational hypertension, oligohydramnios, nonreassuring fetal status, postterm pregnancy, and various maternal medical conditions such as chronic hypertension and diabetes (American College of Obstetricians and Gynecologists, 2013b).
 Contraindications
Contraindications
Methods to induce or augment labor are contraindicated by most conditions that preclude spontaneous labor or delivery. The few maternal contraindications are related to prior uterine incision type, contracted or distorted pelvic anatomy, abnormally implanted placentas, and uncommon conditions such as active genital herpes infection or cervical cancer. Fetal factors include appreciable macrosomia, severe hydrocephalus, malpresentation, or nonreassuring fetal status.
 Techniques
Techniques
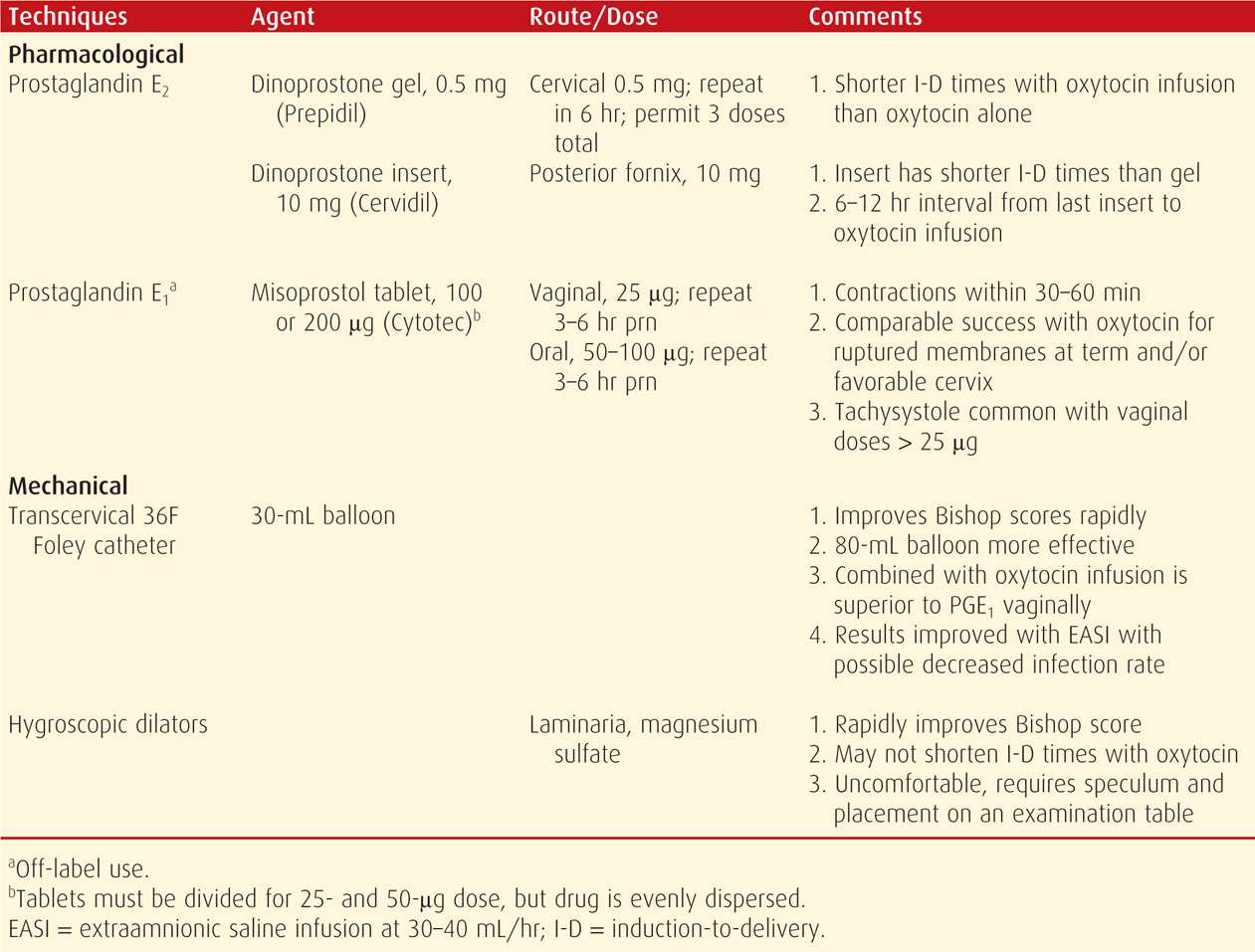
Oxytocin has been used for decades to induce or augment labor. Other effective methods include prostaglandins, such as misoprostol and dinoprostone, and mechanical methods that encompass stripping of membranes, artificial rupture of membranes, extraamnionic saline infusion, transcervical balloons, and hygroscopic cervical dilators. Importantly, and as recommended in Guidelines for Perinatal Care, each obstetrical department should have its own written protocols that describe administration of these methods for labor induction and augmentation (American Academy of Pediatrics and American College of Obstetricians and Gynecologists, 2012).
 Risks
Risks
Maternal complications associated with labor induction consist of cesarean delivery, chorioamnionitis, uterine scar rupture, and postpartum hemorrhage from uterine atony.
Cesarean Delivery Rate
This is especially increased in nulliparas undergoing induction (Luthy, 2004; Yeast, 1999). Indeed, several investigators have reported a two- to threefold increased risk (Hoffman, 2003; Maslow, 2000; Smith, 2003). Moreover, these rates are inversely related with cervical favorability at induction, that is, the Bishop score (Vahratian, 2005; Vrouenraets, 2005). The increased risk for cesarean delivery with labor induction does not appear to be lowered with preinduction cervical ripening in the nullipara with an unfavorable cervix (Mercer, 2005). In fact, the cesarean delivery rate following elective induction was significantly increased even in women with a Bishop score of 7 or greater compared with that in those with spontaneous labor (Hamar, 2001). Station and position of the fetal vertex may also affect success rates. For example, in nulliparas at > 41 weeks’ gestation and with an unengaged vertex, the cesarean delivery rate was increased 12-fold compared with that in women with an engaged fetal vertex (Shin, 2004).
The premise that elective labor induction increases the risk of cesarean delivery has been questioned (Macones, 2009). Many studies have compared women undergoing labor induction to those laboring spontaneously. However, using women undergoing expectant management, Osmundson and colleagues (2010, 2011) reported similar cesarean delivery rates in more than 4000 women undergoing elective induction between 39 and nearly 41 weeks with or without a favorable cervix. Currently, this subject remains unresolved.
Chorioamnionitis
Amniotomy is often selected to augment labor (p. 531). Women whose labor is managed with amniotomy have an increased incidence of chorioamnionitis compared with those in spontaneous labor (American College of Obstetricians and Gynecologists, 2013a).
Rupture of a Prior Uterine Incision
Uterine rupture during labor in women with a history of prior uterine surgery can be catastrophic (Chap. 31, p. 613). Some of these risks were quantified by Lydon-Rochelle and associates (2001), who reported that the uterine rupture risk is increased threefold for women in spontaneous labor with a uterine scar. With oxytocin labor induction without prostaglandins, the risk was fivefold increased, and with prostaglandins, it was strikingly increased 15.6-fold. The Maternal-Fetal Medicine Units Network also reported a threefold increased risk of uterine scar rupture with oxytocin, and this was even higher when prostaglandins were also used (Landon, 2004). The American College of Obstetricians and Gynecologists (2013d) recommends against the use of misoprostol for preinduction cervical ripening or labor induction in women with a prior uterine scar (Chap. 31, p. 615).
Uterine Atony
Postpartum hemorrhage from uterine atony is more common in women undergoing induction or augmentation. And, atony with intractable hemorrhage, especially during cesarean delivery, is a frequent indication for peripartum hysterectomy (Shellhaas, 2009). In a study from Parkland Hospital, labor induction was associated with 17 percent of 553 emergency peripartum hysterectomies (Hernandez, 2013). In the United States, Bateman and coworkers (2012) reported that the postpartum hysterectomy rate increased 15 percent between 1994 and 2007. This was largely attributable to increased rates of atony associated with more medical labor inductions and more primary and repeat cesarean deliveries. Finally, elective induction was associated with more than a threefold increased rate of hysterectomy in the analysis by Bailit and colleagues (2010).
 Elective Labor Induction
Elective Labor Induction
There can be no doubt that elective induction for convenience has become more prevalent. In the United States between 1991 and 2006, rates of early term labor induction increased significantly for all race and ethnicity groups (Murthy, 2011). This was highest for non-Hispanic white women in 2006. In this group, the rate was 20.5 percent if there was either diabetes or hypertension and was 9 percent for women without these indications. Clark and coworkers (2009) reported data from 14,955 deliveries at 37 weeks or greater. They noted that 32 percent were elective deliveries, and 19 percent were elective labor inductions.
The American College of Obstetricians and Gynecologists (2013b) does not endorse this widespread practice. Occasional exceptions might include logistical and other reasons such as a risk of rapid labor, a woman who lives a long distance from the hospital, or psychosocial indications. We are also of the opinion that routine elective induction at term is not justified because of the increased risks for adverse maternal outcomes. Elective delivery before 39 completed weeks is also associated with significant and appreciable adverse neonatal morbidity (Chiossi, 2013; Clark, 2009; Tita, 2009). If elective induction is considered at term, inherent risks must be discussed, informed consent obtained, and guidelines followed as promulgated by the American College of Obstetricians and Gynecologists (2013b), which are detailed in Chapter 31 (p. 610).
Guidelines to discourage elective inductions have been described by Fisch (2009) and Oshiro (2013) and their associates. Both groups reported significant decreases in elective delivery rates following guideline initiation. Tanne (2013) surveyed more than 800 United States hospitals and reported that efforts to reduce early term deliveries are succeeding.
 Factors Affecting Successful Induction
Factors Affecting Successful Induction
Several factors increase or decrease the ability of labor induction to achieve vaginal delivery. Favorable factors include multiparity, body mass index (BMI) < 30, favorable cervix, and birthweight < 3500 g (Peregrine, 2006; Pevzner, 2009). For both nulliparas and multiparas, Kominiarek and colleagues (2011) found that labor duration to reach the active phase and to complete dilatation was adversely affected by a higher BMI.
In many cases, the uterus is simply poorly prepared for labor. One example is an “unripe cervix.” Indeed, investigators with the Consortium on Safe Labor reported that elective induction resulted in vaginal delivery in 97 percent of multiparas and 76 percent of nulliparas, but that induction was more often successful with a ripe cervix (Laughon, 2012a). The increased cesarean delivery risk associated with induction is likely also strongly influenced by the induction attempt duration, especially with an unfavorable cervix (Spong, 2012). Simon and Grobman (2005) concluded that a latent phase as long as 18 hours during induction allowed most of these women to achieve a vaginal delivery without a significantly increased risk of maternal or neonatal morbidity. Rouse and associates (2000) recommend a minimum of 12 hours of uterine stimulation with oxytocin after membrane rupture.
PREINDUCTION CERVICAL RIPENING
As noted, the condition of the cervix—described as cervical “ripeness” or “favorability”—is important to successful labor induction. That said, at least some estimates of favorability are highly subjective. In either case, there are pharmacological and mechanical methods that can enhance cervical favorability—also termed preinduction cervical ripening.
Some of the techniques described may have benefits when compared with oxytocin induction alone (Table 26-1). Some are also quite successful for initiating labor. That said, few data support the premise that any of these techniques results in a reduced cesarean delivery rate or in less maternal or neonatal morbidity compared with that in women in whom these methods are not used.
TABLE 26-1. Some Commonly Used Regimens for Preinduction Cervical Ripening and/or Labor Induction
 Cervical “Favorability”
Cervical “Favorability”
One quantifiable method used to predict labor induction outcomes is the score described by Bishop (1964) and presented in Table 26-2. As favorability or Bishop score decreases, the rate of induction to effect vaginal delivery also declines. A Bishop score of 9 conveys a high likelihood for a successful induction. Put another way, most practitioners would consider that a woman whose cervix is 2-cm dilated, 80-percent effaced, soft, and midposition and with the fetal occiput at –1 station would have a successful labor induction. For research purposes, a Bishop score of 4 or less identifies an unfavorable cervix and may be an indication for cervical ripening.
TABLE 26-2. Bishop Scoring System Used for Assessment of Inducibility
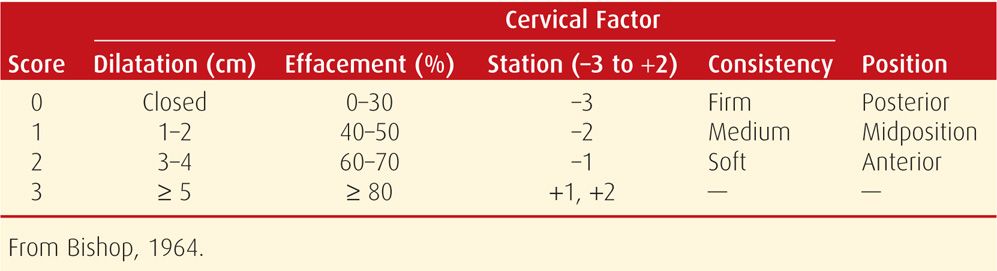
Laughon and coworkers (2011) attempted to simplify the Bishop score by performing a regression analysis on 5610 singleton, uncomplicated deliveries by nulliparas between 370/7 and 416/7 weeks. Only cervical dilation, station, and effacement were significantly associated with successful vaginal delivery. Thus, a simplified Bishop score, which incorporated only these three parameters, had a similar or improved positive- or negative- predictive value compared with that of the original Bishop score.
Transvaginal sonographic measurement of cervical length has been evaluated as a Bishop score alternative. Hatfield and associates (2007) performed a metaanalysis of 20 trials in which cervical length was used to predict successful induction. Because of study criteria heterogeneity—including the definition of “successful induction”—the authors concluded that the question remains unanswered. Both this study and the one by Uzun and colleagues (2013) found that sonographically determined cervical length was not superior to the Bishop score for predicting induction success.
 Pharmacological Techniques
Pharmacological Techniques
Unfortunately, women frequently have an indication for induction but also have an unfavorable cervix. Thus, considerable research has been directed toward techniques to “ripen” the cervix before uterine contraction stimulation. Importantly, more often than not, techniques used to improve cervical favorability also stimulate contractions and thereby aid subsequent labor induction or augmentation. Techniques most commonly used for preinduction cervical ripening and induction include several prostaglandin analogues.
Prostaglandin E2
Dinoprostone is a synthetic analogue of prostaglandin E2. It is commercially available in three forms: a gel, a time-release vaginal insert, and a 10-mg suppository. The gel and time-release vaginal insert formulations are indicated only for cervical ripening before labor induction. However, the 10-mg suppository is indicated for pregnancy termination between 12 and 20 weeks and for evacuation of the uterus after fetal demise up to 28 weeks.
Local application of dinoprostone is commonly used for cervical ripening (American College of Obstetricians and Gynecologists, 2013b). Its gel form—Prepidil—is available in a 2.5-mL syringe for an intracervical application of 0.5 mg of dinoprostone. With the woman supine, the tip of a prefilled syringe is placed intracervically, and the gel is deposited just below the internal cervical os. After application, the woman remains reclined for at least 30 minutes. Doses may be repeated every 6 hours, with a maximum of three doses recommended in 24 hours.
A 10-mg dinoprostone vaginal insert—Cervidil—is also approved for cervical ripening. This is a thin, flat, rectangular polymeric wafer held within a small, white, mesh polyester sac (Fig. 26-1). The sac has a long attached tail to allow easy removal from the vagina. The insert provides slower release of medication—0.3 mg/hr—than the gel form. Cervidil is used as a single dose placed transversely in the posterior vaginal fornix. Lubricant should be used sparingly, if at all, because it can coat the device and hinder dinoprostone release. Following insertion, the woman should remain recumbent for at least 2 hours. The insert is removed after 12 hours or with labor onset and at least 30 minutes before the administration of oxytocin.
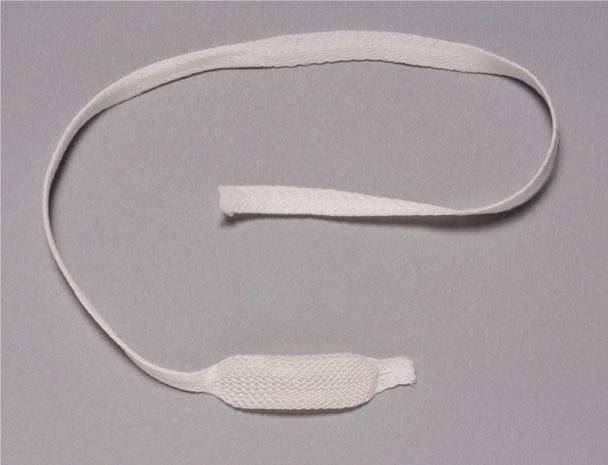
FIGURE 26-1 Cervidil vaginal insert contains 10 mg of dinoprostone designed to release approximately 0.3 mg/hr during a 10-hour period.
Most metaanalyses of dinoprostone efficacy report a reduced time to delivery within 24 hours. However, they do not consistently show a reduction in the cesarean delivery rate. Kelly and coworkers (2009) provided a Cochrane review of 63 trials and 10,441 women given vaginal prostaglandins or either placebo or no treatment. These investigators reported a higher vaginal delivery rate within 24 hours when prostaglandins were used. They also found that cesarean delivery rates were unchanged. Similar results were reported after another Cochrane review of intracervical dinoprostone gel by Boulvain and associates (2008). Compared with placebo or no treatment, a reduced risk of cesarean delivery was found only in a subgroup of women with an unfavorable cervix and intact membranes. Finally, the Foley catheter versus vaginal prostaglandin E2 gel for induction of labor at term (PROBAAT trials) were unblinded, randomized trials comparing these two options (Jozwiak, 2011, 2013a, 2014). There was no difference in cesarean delivery rate, a finding consistent with accompanying metaanalyses.
Side Effects. Uterine tachysystole has been reported to follow vaginally administered prostaglandin E2 in 1 to 5 percent of women (Hawkins, 2012). Although definitions of uterine activity vary among studies, most use the definition recommended by the American College of Obstetricians and Gynecologists (2013c):
1. Uterine tachysystole is defined as > 5 contractions in a 10-minute period. It should always be qualified by the presence or absence of fetal heart rate abnormalities.
2. Uterine hypertonus, hyperstimulation, and hypercontractility are terms no longer defined, and their use is not recommended.
Because uterine tachysystole associated with fetal compromise may develop when prostaglandins are used with preexisting spontaneous labor, such use is not recommended. If tachysystole follows the 10-mg insert, its removal by pulling on the tail of the surrounding net sac will usually reverse this effect. Irrigation to remove the gel preparation has not been shown to be helpful.
The manufacturers recommend caution when these preparations are used in women with ruptured membranes. Caution is also recommended when they are used in women with glaucoma or asthma. In a review of 189 women with asthma, however, dinoprostone was not associated with asthma worsening or exacerbation (Towers, 2004). Other contraindications listed by the manufacturers include a history of dinoprostone hypersensitivity, suspicion of fetal compromise or cephalopelvic disproportion, unexplained vaginal bleeding, women already receiving oxytocin, those with six or more previous term pregnancies, those with a contraindication to vaginal delivery, or women with a contraindication to oxytocin or who may be endangered by prolonged uterine contractions, for example, those with a history of cesarean delivery or uterine surgery.
Administration. Prostaglandin E2 preparations should only be administered in or near the delivery suite. Moreover, uterine activity and fetal heart rate should be monitored (American College of Obstetricians and Gynecologists, 2013b). These guidelines stem from the risk of uterine tachysystole. When contractions begin, they are usually apparent in the first hour and show peak activity in the first 4 hours. According to manufacturer guidelines, oxytocin induction that follows prostaglandin use for cervical ripening should be delayed for 6 to 12 hours following prostaglandin E2 gel administration or for at least 30 minutes after removal of the vaginal insert.
Prostaglandin E1
Misoprostol—Cytotec—is a synthetic prostaglandin E1 that is approved as a 100- or 200-μg tablet for peptic ulcer prevention. It has been used “off label” for preinduction cervical ripening and may be administered orally or vaginally. The tablets are stable at room temperature. Although widespread, the off-label use of misoprostol has been controversial (Wagner, 2005; Weeks, 2005). Specifically, G. D. Searle & Company (Cullen, 2000) notified physicians that misoprostol is not approved for labor induction or abortion. At the same time, however, the American College of Obstetricians and Gynecologists (2013b) reaffirmed its recommendation for use of the drug because of proven safety and efficacy. It currently is the preferred prostaglandin for cervical ripening at Parkland Hospital.
Vaginal Administration. Numerous studies have reported equivalent or superior efficacy for cervical ripening or labor induction with vaginally administered misoprostol tablets compared with intracervical or intravaginal prostaglandin E2. A metaanalysis of 121 trials also confirmed these findings (Hofmeyr, 2010). Compared with oxytocin or with intravaginal or intracervical dinoprostone, misoprostol increased the vaginal delivery rate within 24 hours. Moreover, although the uterine tachysystole rate increased, this did not affect cesarean delivery rates. Compared with dinoprostone, misoprostol decreased the need for oxytocin induction, but it increased the frequency of meconium-stained amnionic fluid. Higher doses of misoprostol are associated with a decreased need for oxytocin but more uterine tachysystole with and without fetal heart rate changes. The American College of Obstetricians and Gynecologists (2013b) recommends the 25-μg vaginal dose—a fourth of a 100-μg tablet. The drug is evenly distributed among these quartered tablets.
Wing and colleagues (2013) recently described use of a vaginal polymer insert containing 200 μg of PGE1. They compared its efficacy with 10-mg dinoprostone inserts, and preliminary observations are favorable.
Oral Administration. Prostaglandin E1 tablets are also effective when given orally. Ho and coworkers (2010) performed a randomized controlled trial comparing titrated oral misoprostol with oxytocin. They found similar rates of vaginal delivery and side effects. In a metaanalysis of nine trials including nearly 3000 women, however, there were reported improvements in various outcomes with oral misoprostol (Kundodyiwa, 2009). In particular, there was a significantly lower cesarean delivery rate for the five trials comparing oral misoprostol with dinoprostone—relative risk 0.82. For the two trials comparing oral with vaginal misoprostol, oral misoprostol was associated with a lower rate of uterine tachysystole with fetal heart rate changes, but there were no significant differences with respect to rates of cesarean delivery or other outcomes.
Nitric Oxide Donors
Several findings have led to a search for clinical agents that stimulate nitric oxide (NO) production locally (Chanrachakul, 2000a). This is because nitric oxide is likely a mediator of cervical ripening (Chap. 21, p. 423). Also, cervical nitric oxide metabolite concentrations are increased at the beginning of uterine contractions. Last, cervical nitric oxide production is very low in postterm pregnancy (Väisänen-Tommiska, 2003, 2004).
Bullarbo and colleagues (2007) reviewed rationale and use of two nitric oxide donors, isosorbide mononitrate and glyceryl trinitrate. Isosorbide mononitrate induces cervical cyclooxygenase 2 (COX-2), and it also brings about cervical ultrastructure rearrangement similar to that seen with spontaneous cervical ripening (Ekerhovd, 2002, 2003). Despite this, clinical trials have not shown nitric oxide donors to be as effective as prostaglandin E2 for cervical ripening (Chanrachakul, 2000b; Osman, 2006). Moreover, the addition of isosorbide mononitrate to either dinoprostone or misoprostol did not enhance cervical ripening either in early or term pregnancy nor did it shorten time to vaginal delivery (Collingham, 2010; Ledingham, 2001; Wölfler, 2006). A metaanalysis of 10 trials including 1889 women concluded that nitric oxide donors do not appear to be useful for cervical ripening during labor induction (Kelly, 2011).
 Mechanical Techniques
Mechanical Techniques
These include transcervical placement of a Foley catheter with or without extraamnionic saline infusion, hygroscopic cervical dilators, and membrane stripping. In a recent metaanalysis of 71 randomized trials including 9722 women, Jozwiak and associates (2012) reported that mechanical techniques reduced the risk of uterine tachysystole compared with prostaglandins, although cesarean delivery rates were unchanged. Trials comparing mechanical techniques with oxytocin found a lower rate of cesarean delivery with mechanical methods. Trials comparing mechanical techniques with dinoprostone found a higher rate of multiparous women undelivered at 24 hours with mechanical techniques. Another metaanalysis done to compare Foley catheter placement with intravaginal dinoprostone inserts also found similar rates of cesarean delivery and less frequent uterine tachysystole (Jozwiak, 2013a).
Transcervical Catheter
Generally, these techniques are only used when the cervix is unfavorable because the catheter tends to come out as the cervix opens. In most cases, a Foley catheter is placed through the internal cervical os, and downward tension is created by taping the catheter to the thigh (Mei-Dan, 2014). A modification of this—extraamnionic saline infusion (EASI)—consists of a constant saline infusion through the catheter into the space between the internal os and placental membranes (Fig. 26-2). Karjane and coworkers (2006) reported that chorioamnionitis was significantly less frequent when infusion was done compared with no infusion—6 versus 16 percent. A systematic review and metaanalysis of 30 trials found that Foley catheter induction alone compared with prostaglandins resulted in higher infection rates unless saline was infused (Heinemann, 2008).
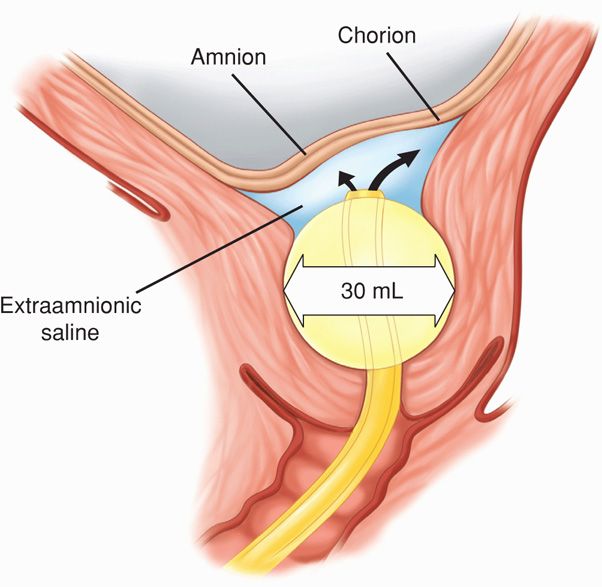
FIGURE 26-2 Extraamnionic saline infusion (EASI) through a 26F Foley catheter that is placed through the cervix. The 30-mL balloon is inflated with saline and pulled snugly against the internal os, and the catheter is taped to the thigh. Room-temperature normal saline is infused through the catheter port of the Foley at 30 or 40 mL/hour by intravenous infusion pump.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


