CHAPTER 5 Imaging techniques in gynaecology
Introduction
Since the discovery of X-rays by Roentgen in 1895, there has been an explosion in technology for imaging the human body; in addition to ionizing radiation, high-frequency sound (Wade 1999), radiolabelled pharmaceuticals and non-ionizing radiation in strong magnetic fields are used. The parallel expansion in computer technology has enabled the development of cross-sectional imaging using computed tomographic (CT) techniques, and three-dimensional imaging using magnetic resonance imaging (MRI) data.
Methodology
Ultrasound
In Glasgow in 1950, Ian Donald used an industrial flaw detector, designed for testing the integrity of steel boilers, to demonstrate that the massive abdominal swelling of one of his patients was fluid and not solid (Kurjak 2000). A large ovarian cyst that proved to be benign was subsequently removed. Since then, the rapid and continuing evolution of ultrasound technology has led to a proliferation of applications in almost all aspects of medicine and surgery.
The choice of frequency is a compromise between the spatial resolution and the depth of penetration required. The higher the frequency, the better the resolution, but the greater the attenuation of the beam within the tissues. Hence, for abdominal scanning, frequencies of between 3.5 and 5 MHz are commonly employed. Probes designed for intracavitary and intraoperative use employ higher frequencies (8–15 MHz) because the organs of interest are closer to the transducer. This enables higher resolution images to be obtained, and also allows study of the movement of structures when pressure is applied to the probe, which gives important diagnostic clues on their relative mobility. The drawbacks of transvaginal scanning are practical (intolerance of the probe by the very young and old, and in the presence of scarring) and diagnostic (the depth of view is limited to approximately 70 mm) (Bennett and Richards 2000). By sweeping an array through the tissues, a three-dimensional scan can be created; while most useful in obstetrics to visualize complex structures such as the fetal face, it also displays uterine anatomy well (Alcazar and Galvan 2009).
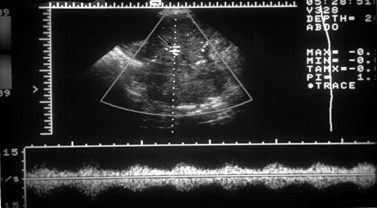
Doppler operates by detecting the change in frequency of ultrasound echoes caused by movement of the target. In the simplest system, this is done continuously with only minimal control of the beam direction. Continuous wave Doppler is well suited to fetal heart monitoring, especially because movements of the fetus do not interrupt the signal. In gynaecology, the vessels of interest are small so precise placement of the Doppler sample is a prerequisite. This can be achieved with pulsed Doppler. The Doppler gate is superimposed on a real-time image that allows the target to be pinpointed (Figure 5.1). The Doppler signal depicts a range of blood velocities occurring in the selected vessel over time. Output can be audio or as a strip chart on which intensity indicates the strength of the signal at each velocity in the spectrum. A variety of measurements can be made from these tracings, the most useful of which are systolic/diastolic velocity ratios. These are measures of the arteriolar resistance to flow, with a low value indicating low vasomotor tone, typical of the placenta and the corpus luteum. This pattern also occurs in inflammation and malignancy. High indices are typical of inactive tissue, such as the resting uterus. Doppler can be used to measure fetal and uteroplacental blood flow, thereby producing physiological information (Brinkman and Wladimiroff 2000).
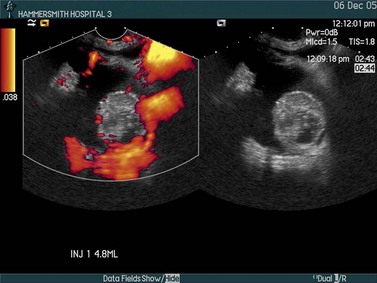
In colour Doppler scanning, the same process is applied across an area of interest. The velocity signals are presented as a colour-coded overlay, superimposed on the real-time scan (Figure 5.2). Although the Doppler information is less rich than with spectral Doppler (only the mean velocity or the amount of flow is depicted), the angiogram-like map provides information on the morphological arrangement of the vascular tree, and its sensitivity allows vessels as small as approximately 1 mm in diameter to be detected. Colour Doppler is often used to locate a vessel to guide placement of the spectral Doppler gate for haemodynamic analysis.
Magnetic resonance imaging
The female pelvis is suitable for MRI examination because of the minimal effect of respiratory motion on the pelvic organs. By placing the receiver coil adjacent to the tissue of interest (e.g. endovaginally to maximize signal from the cervix), very-high-resolution images of an area of interest may be obtained. However, as the data to produce a set of images are accumulated over 5–10 min, patients are required to remain still during this time. If multiple sequences and multiple planes are employed, the total imaging time may exceed 30 min which reduces patient tolerance. However, newer faster pulse sequences with breath-hold techniques and improved computer software are greatly reducing scan times. Recently, open design MR scanners and production of MR-compatible equipment has produced an explosion in the field of ‘interventional MRI’. This has expanded the applications of MRI from being purely diagnostic to its use during treatment, such as for placing brachytherapy implants (Popowski et al 2000) or monitoring thermal ablative therapy.
Radionuclide imaging
The purity and specificity of monoclonal antibodies gives them an important role in tumour detection and possibly in the targeting of antitumour agents. Different anticytokeratin antibodies may help in distinguishing a primary ovarian adenocarcinoma from a metastatic adenocarcinoma, especially of colorectal origin (McCluggage 2000). These antibodies have also helped to clarify the origin of the peritoneal disease in most cases of pseudomyxoma peritonei. In recent years, several studies have also investigated the value of a variety of monoclonal antibodies in the diagnosis of ovarian sex cord stromal tumours, and in the distinction between these neoplasms and their histological mimics. Of these, anti-alpha-inhibin and CD99 appear to be of most diagnostic value (Choi et al 2000). Antibodies should always be used as part of a larger panel and not in isolation.
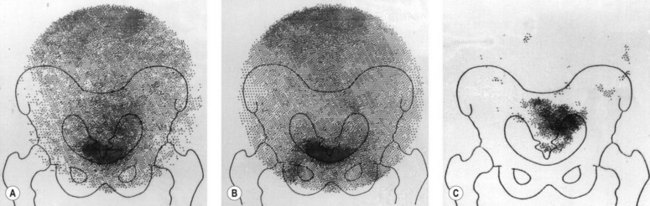
Following injection of the antibody, a gamma camera provides serial images of the distribution and uptake of radiolabelled antibody between 18 and 72 h after the antibody has been administered. The radionuclide 111In is ideally suited for tomographic studies using images produced by a gamma camera mounted on a gantry which rotates through 360°. The images are reconstructed by computer in the same manner as X-ray CT. 111In-labelled antibody is taken up into the liver, spleen, bone marrow and, occasionally, adrenal glands but is a more suitable radiolabel than 131I. Excretion of 111In into the bladder has not been a problem, although non-specific bowel uptake may account for false-positive results. An example of an 111In study is shown in Figure 5.3. A central area of increased uptake is apparent at the site of a primary ovarian cancer.
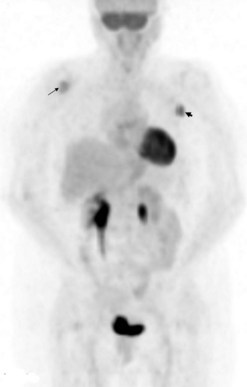
18FDG (18fluorodeoxyglucose) is a non-specific positron-emitting tracer. It is an analogue of glucose, thereby reflecting metabolism and detecting the increased glycolysis associated with several tumour types. It gains entry into cells by membrane transporter proteins, such as Glut-1, which are expressed in many tumours. It is phosphorylated intracellularly to FDG-6-phosphate and retained within malignant cells. Tumour hypoxia may also increase 18FDG accumulation via activation of glycolysis. The quantitative parameter used is typically a standardized uptake value (SUV), which represents the tissue activity within a region of interest corrected for the injected activity and the patient’s body weight. A new lesion (Figure 5.4) or a rise in SUV within a lesion indicates disease progression. Whether this can be used as a marker for early therapy remains to be proven.
Clinical Applications
Normal anatomy and variations
Uterus
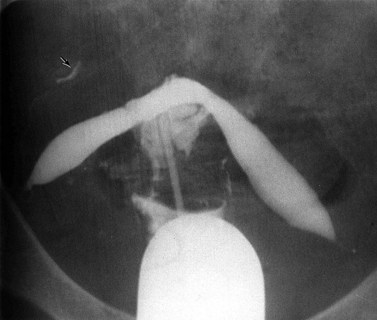
The normal uterine cavity is delineated as a triangular structure on hysterosalpingography, with the cornua and the internal cervical os as the corners. Intracavitary abnormalities, both congenital and acquired, such as internal septations and divisions may be defined using this technique (Figure 5.5). Similar information can be acquired with ultrasound following instillation of saline into the uterine cavity (hysterosonography) (van den Brule et al 1998).
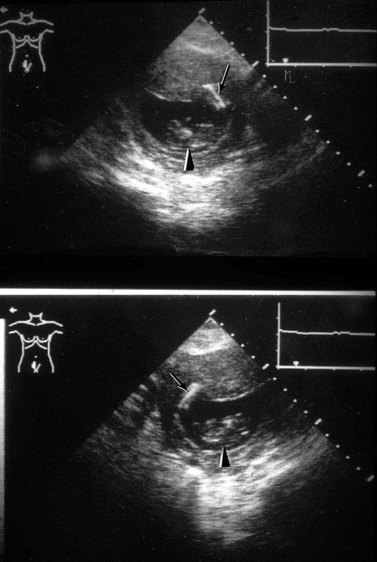
On ultrasound, the uterine cavity is normally represented by a bright line of apposition of the endometrial layers, although occasionally a trace of fluid can be seen at menstruation. Persistent fluid or fluid in a non-menstruating woman is abnormal. In adolescence, it may be caused by vaginal atresia, where the upper vagina dilates more than the uterus so that haematocolpos dominates the picture, while in postmenopausal women, cervical stenosis, either fibrotic or malignant, must be considered. Ultrasound is also useful in detecting the position of an intrauterine device; provided the coil lies in the uterus, it is easy to locate, but a coil that has penetrated through the myometrium is obscured by echoes from bowel gas (Figure 5.6).
The entire uterus can be imaged using ultrasound (Figure 5.7) and its size measured accurately. This is useful in precocious or delayed puberty and in planning brachytherapy. The endometrium is seen as an echogenic layer of uniform texture, often with a fine echo-poor margin. Its thickness varies through the menstrual cycle from 12 mm premenstrually (double-layer thickness) to a thin line after menstruation. The endometrium gradually thins after menopause unless supported by hormones.
The morphology of the normal uterus, however, is best defined on MRI where its zonal architecture may be recognized (Hricak et al 1983). On T2-weighted images, the endometrium is seen as a central high-signal stripe which increases in thickness in the secretory phase of the menstrual cycle. The inner myometrium (junctional zone) is of lower signal intensity than the outer myometrium on T2 weighting, and correlates histologically with a layer of more densely packed smooth muscle.
Fallopian tubes
The patency of the fallopian tubes may be demonstrated on hysterosalpingography where filling and free spill into the peritoneal cavity may be seen (Figure 5.5). Ultrasound contrast salpingography is currently being evaluated to reduce the radiation dose to the ovaries in patients trying to conceive. Normal uterine tubes cannot be demonstrated on ultrasound, but instillation of microbubble contrast agents into the uterus and tubes permits their visualization and can be used as an initial screening test for tubal patency. Although the anatomical detail is less than that offered by conventional X-ray salpingography and false-positive results occur, this technique of ultrasound salpingography seems likely to find an important role as an initial screen; if the tubes are demonstrated to be patent, no further investigation is necessary and this should result in a reduction of radiation exposure (Van Voorhis 2008).
Ovaries
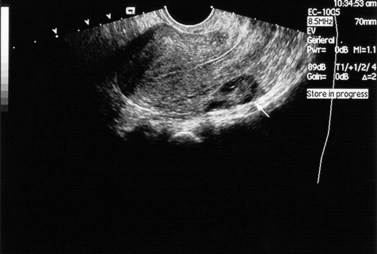
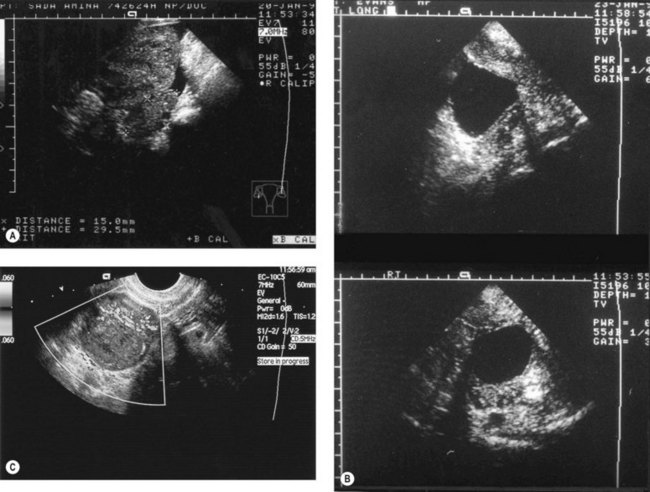
The ovaries are best imaged with ultrasound (either transabdominal or, preferably, transvaginal). Changes in their appearance can be correlated with their functional status. Infantile ovaries are small (except in the neonate when hypertrophy and follicles stimulated by maternal hormones may be a surprising finding) and they enlarge before puberty. Follicular development begins before menstruation, but these cycles and those at the menopause are often imperfect so that follicles may persist and continue enlarging for several months. Normally, ovulation occurs at a follicle size of 20–25 mm diameter and the echo-free follicle is replaced by a corpus luteum which can be cystic or solid. Corpora lutea produce a confusing variety of appearances, whose only consistent feature is their transience (Figure 5.8A–C). In doubtful cases, a rescan at 6 weeks to image them at a different phase of the cycle may be needed to resolve their identity. The postmenopausal ovary is usually too small to identify with ultrasound.
Ovarian varices
The pelvic congestion syndrome is one of many causes of chronic pelvic pain, and is associated with the presence of large varices within the broad ligaments (Liddle and Davies 2007). When pelvic symptoms are severe, there may be gross dilatation of the ovarian veins, with reflux down into the pelvis and often into the legs. These vessels are best demonstrated by selective ovarian venography, although they may also be imaged with Doppler ultrasound (Haag and Manhes 1999). Venography is performed via a femoral or internal jugular venous approach, and the ovarian veins are selectively catheterized with an appropriately shaped angiographic catheter. Satisfactory retrograde opacification of pelvic varices is achieved by injecting contrast medium through the selectively placed catheter with the patient almost upright on a tilting table, while the Valsalva manoeuvre is performed.
Treatment of this condition is primarily surgical and consists of venous ligation. Symptomatic relief has been reported following transcatheter ovarian vein embolization (Ganeshan et al 2007).
Investigation of female infertility
Transvaginal sonography has largely replaced the transabdominal approach in infertility practice because of the superior anatomical display and because it allows precisely guided aspiration of follicles and fluid in the pouch of Douglas. More precise measurement of follicles is possible, and the corpus luteum is easily recognized. In the midluteal phase, it appears as an oval structure 30–35 mm long and 20–25 mm wide with a wide variety of sonographic appearances (Baerwald et al 2005). Endometrial reflectivity patterns have been proposed as another way to assess ovulation (Randall et al 1989). Ultrasound can only provide presumptive evidence of ovulation/pregnancy. The collection of secondary oocytes constitutes definitive evidence of ovulation. The appearance of internal echoes before the follicle reaches 18 mm or continuous enlargement to 30–40 mm indicates follicular failure.
The waveforms of blood flow in vessels supplying the ovaries of women undergoing IVF have been studied using transvaginal power Doppler ultrasound (Palomba et al 2008). The observation of blood flow patterns did not improve any reproductive outcomes and is currently not advocated in IVF programmes.
MRI is valuable in the investigation of infertility where uterine pathology is suspected, and provides a particularly high diagnostic yield in patients with dysmenorrhoea and menorrhagia (deSouza et al 1995). It should be part of the investigation of patients with persistent unexplained infertility awaiting costly procedures such as gamete intrafallopian transfer and IVF. MRI should also be used before myomectomy in order to differentiate between leiomyoma and adenomyoma, as attempts to perform a myomectomy on a localized adenomyoma often result in extensive uterine damage.
Adenomyosis and endometriosis
The diagnosis of adenomyosis is often suggested by symptoms of hypermenorrhoea and dysmenorrhoea, but similar symptoms are also produced by leiomyomas. Hysterosalpingography may show multiple small tracks of contrast extending into the myometrium but is now obsolete. Ultrasound in skilled hands may be useful (Dueholm and Lundorf 2007).
Adenomyosis is best demonstrated on T2-weighted MRI, with which two patterns (focal and diffuse) can be recognized (Hricak et al 1992, Byun et al 1999). In focal adenomyosis, there is a localized ill-defined mixed-signal-intensity mass (adenomyoma) within the myometrium (Figure 5.9). Diffuse adenomyosis presents with diffuse or irregular thickening of the junctional zone, often with underlying high-signal foci (Figure 5.10). Pathologically, this represents smooth muscle hypertrophy and hyperplasia surrounding a focus of basal endometrium. It is the smooth muscle changes that are easily recognized by MRI rather than the foci of heterotopic glandular epithelium. Values for junctional zone thickness from >5 to >12 mm have been suggested for the diagnosis of adenomyosis. In the authors’ experience, however, the thickening of the junctional zone that is described in adenomyosis (Reinhold et al 1999) is not diagnostic of adenomyosis on its own; it may be seen in hypermenorrhoea where no pathological evidence for adenomyosis has subsequently been shown. In these instances, absolute values for junctional zone widths are unhelpful (Hauth et al 2007), and ratios to the width of the outer myometrium or the cervical stroma may be more meaningful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree