Fig. 5.1
Distribution of methods of sterilization in the Netherlands in 2010 (By courtesy of Michel Vleugels, MD, PhD, personal communication)
Even before the introduction of the hysteroscope in the nineteenth century attempts have been undertaken to ensure a permanent contraception by manipulating the uterus or the fallopian tubes transcervically through a vaginal route in the extent that passage is obstructed (van der Leij 1997). Initially chemical agents or electrothermical instruments were introduced blindly, with tactile feedback only, the effect of which was disappointing. In 1927 for the first time an electrocautery method with hysteroscopic guidance was tested albeit with the same mediocre results. Later attempts with electro-, cryo-, or Nd-YAG laser coagulation were equally unsuccessful in achieving bilateral occlusion (in 15 % up to a maximum of 60 % of cases) (Fig. 5.2a, b; van der Leij 1997; Wamsteker 1977; Cooper 1992; Lindemann and Mohr 1974).
Fig. 5.2
(a) Distal tip of the coagulation probe; (a) insulated tip, (b) coagulation electrode, (c) flexible conduction cable. (b) Thermacoagulator (Wiest KG); (a) Temperature regulator, (b) connection for thermocoagulator probe, (c) timer (a, b Hyst ster Wamsteker: diss Wamsteker)
In developing countries experiments with quinacrine pellets in the uterine cavity have been performed with reasonable success, where the blind insertion has the advantage of low cost (Fig. 5.3). Serious side effects have not been seen, and the mutagen effects however are still under investigation (van der Leij 1997).


Fig. 5.3
Since hysteroscopy found its way as a routine diagnostic and interventional technique in the 1970s and 1980s of the last century even more methods have been tested, among which are several types of intratubal occlusion devices (Fig. 5.4). All of these initial methods have been abandoned, either due to complications or to lack of effectiveness or both (Cooper 1992; Thatcher 1988; Brundin 1991; Hamou et al. 1984).
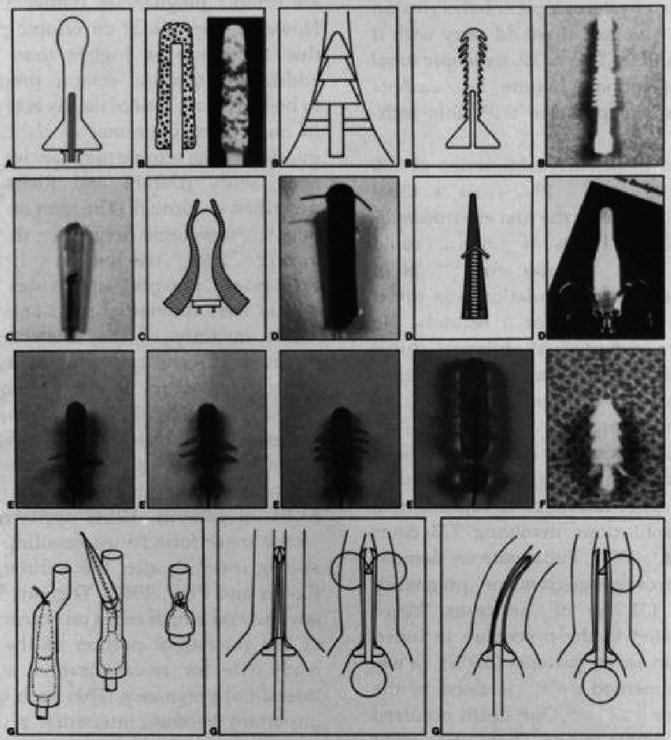
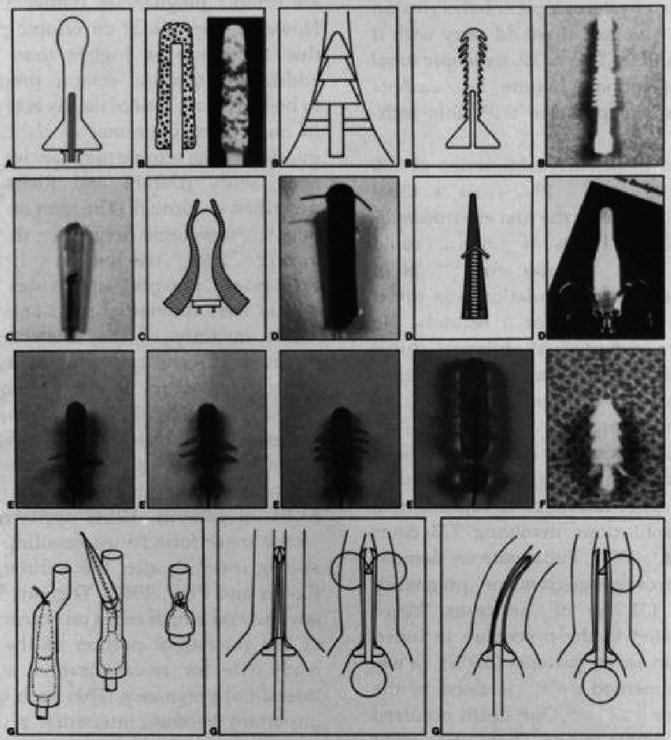
Fig. 5.4
Various experimental intratubal devices (Various devices: http://www.expert-reviews.com/doi/abs/10.1586/17434440.2.5.623)
From 2003 to 2006 Chiroxia Ltd. (Dublin, Ireland) investigated the hysteroscopic application of a cyanoacrylate-based liquid polymer implant, in which the author of this article performed the study on explanted uteri (Figs. 5.5 and 5.6). Although the initial results were promising the investors withdrew their support and the project was discontinued.



Fig. 5.5
Instillation of liquid Chiroxia obstructing material in explanted uterus (Recording of personal explant study)

Fig. 5.6
Extremely firm adhesion of solidified Chiroxia material in intramural tubal lumen of explanted uterus (By courtesy of Chiroxia Ltd.)
5.2 Ovabloc
In 1988 Ovabloc®, a new hysteroscopic sterilization technique was introduced on the Dutch market after preclinical and clinical studies had been performed since 1967 (Loffer 1984; Reed and Erb 1979).
To date it is estimated that around 2,000 procedures have taken place in the Netherlands.
It is a formed-in-place silicone polymer that causes bilateral occlusion in 95 % of cases (Loffer 1984; Ligt-Veneman et al. 1999).
Through a double catheter system the two component fluid siloxane mixture with a high viscosity is injected in the fallopian tubes, which cures within minutes and hereby causes occlusion of the tubal lumen (Fig. 5.7). A specially designed siloxane obturator tip, which is preattached on the inner catheter, forms a complex with the intraluminal plug and causes sealing in the uterotubal junction.
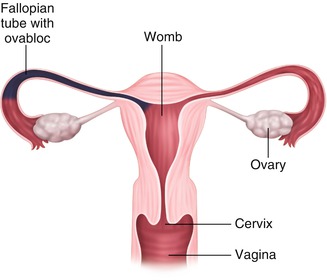
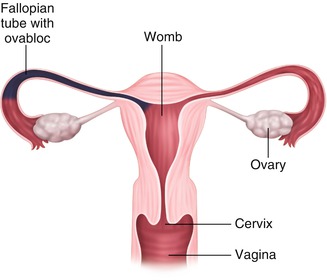
Fig. 5.7
Ovabloc material injected into right tubal lumen (Ovabloc: http://www.ovabloc.nl/ovabloc/the_treatment, Ovabloc cure: http://web.squ.edu.om/med-Lib/MED_CD/E_CDs/Endoscopic%20Surgery%20for%20Gynecologists/Published/Book_Content/Chapters_51-57/Chapter_57/c57p03/c57p03.html)
Failures are caused by (among others) tubal spasm, intracavitary pathology, perforation and inability to position the catheter tip in correct alignment with the tubal lumen.
Especially the latter makes the procedure quite skill dependent.
Although the exact prediction of failure is not possible, some risk factors can be identified, among which are suspicion of intrauterine pathology and nulliparity (van der Leij and Lammes 1996).
After completion of the procedure a pelvic X-ray is made to ensure the integrity and correct position of the plug and the amount of ampullary filling (Fig. 5.8). If the thickness of the plug is insufficient (e.g. due to intracavitary reflux of the material) intrauterine expulsion may occur. The X-ray is then repeated after 3 months to rule out expulsion, which is stated to take place in 3–4 % of cases, usually within the first months after placement (Loffer 1984; van der Leij and Lammes 1996). The use of ultrasound for this second control may well be equivalent since assessment of correct tubal placement is the main goal at this stage and the intramural part of the plug as well as the intrauterine tip is usually easily visualized sonographically.
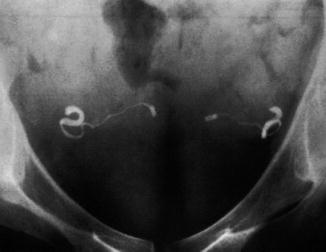
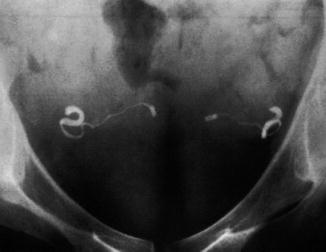
Fig. 5.8
X-ray confirmation test after Ovabloc sterilization showing two adequate plugs (Ovabloc X ray: http://web.squ.edu.om/med-Lib/MED_CD/E_CDs/Endoscopic%20Surgery%20for%20Gynecologists/Published/Book_Content/Chapters_51-57/Chapter_57/c57p03/c57p03.html)
As soon as correct position of both plugs has been established the patient can be allowed to rely on Ovabloc as the sole method of contraception.
According to a multicenter 3 years follow-up study in 398 patients the cumulative pregnancy rate is 0.99 % (Pearl Index 0.13/100 woman-years), which is comparable with the laparoscopic alternative (Ligt-Veneman et al. 1999; Peterson et al. 1996).
The use of Ovabloc declined after the introduction of Essure and has virtually disappeared from the market after the introduction of Adiana.
The system is CE marked, but not FDA approved.
A new version of this device with the same material has recently been developed (Ovalastic). Only scarse clinical data are available yet, the only procedures having been performed either by the author or under his supervision. Basically the procedure has not changed, the ease of use however has made a significant step forward in comparison with the original Ovabloc procedure. A clinical study is in preparation.
5.3 Essure
In November 2001 the European Health Office approved (CE mark) the use of another method of hysteroscopic sterilization which was launched on the Dutch market in 2003: the Essure® system. The FDA PMA approval followed in November 2002.
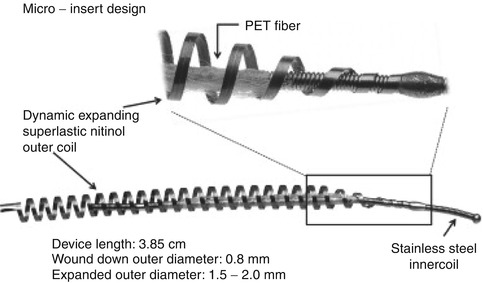
The Essure® micro-insert (Conceptus Inc., sold to Bayer AG. In 2013), initially called STOP, is a dynamically expanding micro-coil with polyethylene terephthalate (PET) fibers wound in and around the inner coil (Fig. 5.9). It is placed through a 5 Fr working channel of a hysteroscope in the intramural section of the fallopian tube, in which it anchors itself by expansion of the coil. The PET fibers subsequently cause a fibrotic reaction, which renders an additional anchoring and obstructing effect (Fig. 5.10a, b).