Introduction
Hypertension is defined as a sustained blood pressure higher than 140/90 mmHg and may be attributable to any of the conditions summarized in Box 35.1. It affects 20–30% of American adults and complicates as many as 5–8% of all pregnancies. Approximately 15% of maternal deaths are attributable to hypertension, making it the second leading cause of maternal mortality in the United States. The classification system of hypertension in pregnancy proposed by the National High Blood Pressure Education Program Working Group is summarized in Box 35.2.
Chronic hypertension complicates as many as 5% of pregnancies and is characterized by a history of high blood pressure before pregnancy, elevated blood pressure during the first half of pregnancy, or elevated blood pressure that persists beyond 12 weeks post partum. Blood pressure is measured in a sitting position with the arm at the level of the heart and multiple measurements are obtained. Other physical findings may include a renal artery bruit, funduscopic abnormalities, an enlarged thyroid gland, diminished peripheral pulses, skin and joint abnormalities.
Laboratory tests include a complete blood count, glucose screen, electrolyte panel, serum creatinine, urinalysis and urine culture. In some cases, additional tests may be needed. In patients with possible renal disease (serum creatinine ≥ 0.8 mg/dL, urine protein > 1 + on dipstick), a 24-h urine collection for creatinine clearance and total protein will provide baseline information that may be helpful in diagnosing the onset of pre-eclampsia later in pregnancy. Additional tests may include antinuclear antibody, thyroid-stimulating hormone, urinary catecholamines, electrocardiogram and chest x-ray.
Box 35.1 Causes of chronic hypertension
Idiopathic
Essential hypertension
Vascular disorders
Renovascular hypertension
Aortic coarctation
Endocrine disorders
Diabetes mellitus
Hyperthyroidism
Pheochromocytoma
Primary hyperaldosteronism
Hyperparathyroidism
Cushing’s syndrome
Renal disorders
Diabetic nephropathy
Chronic renal failure
Acute Renal Failure
Tubular necrosis
Cortical necrosis
Pyelonephritis
Chronic glomerulonephritis
Nephrotic Syndrome
Polycystic kidney
Connective tissue disorders
Systemic lupus erythematosus
Fetal assessment in chronic hypertension
Chronic hypertension, regardless of the cause, increases the risk of poor fetal growth. An initial ultrasound examination should be performed as early as possible to confirm the dates and exclude fetal anomalies. Thereafter, fetal growth usually is assessed every 2–4 weeks. Antepartum fetal monitoring is initiated by 32–34 weeks. Doppler velocimetry of the umbilical, uterine and middle cerebral arteries is helpful in optimizing the timing of delivery, particularly in cases of fetal growth restriction.
Box 35.2 Classification of hypertension in pregnancy
Definition of Hypertension
Mild: Systolic blood pressure ≥140 mmHg
Diastolic blood pressure ≥90 mmHg
Severe: Systolic blood pressure ≥180 mmHg
Diastolic blood pressure ≥110 mmHg
Chronic Hypertension
Hypertension with onset before pregnancy or before 20th week of gestation
Use of antihypertensive medications before pregnancy
Persistence of hypertension beyond 12 weeks postpartum
Pre-eclampsia
Hypertension that occurs after 20 weeks of gestation in a woman with previously normal blood pressure. SBP ≥ 140 mmHg or DBP ≥ 90 mmHg on two occasions at least 6 hours apart
Proteinuria, defined as urinary excretion of 0.3 g protein or higher in a 24-hour urine specimen. This finding usually correlates with a finding of 1 + or greater on dipstick
Note edema is no longer a diagnostic criterion
Note a systolic rise of 30 mm Hg or a diastolic rise of 15 mm Hg no longer diagnostic criteria
Eclampsia
New-onset grand mal seizures in a woman with pre-eclampsia that cannot be attributed to other causes
Superimposed Pre-eclampsia – Eclampsia
Pre-eclampsia or eclampsia that occur in a woman with preexisting chronic hypertension
Gestational Hypertension
Hypertension detected for the first time after midpregnancy
Distinguished from pre-eclampsia by the absence of proteinuria
Working diagnosis only during pregnancy
Transient hypertension of pregnancy
Gestational hypertension that resolves by 12 weeks postpartum
If proteinuria develops in a patient with gestational hypertension, the diagnosis is pre-eclampsia.
If gestational hypertension does not resolve by 12 weeks postpartum, the diagnosis is chronic hypertension
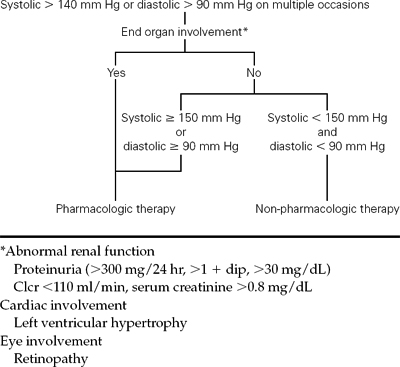
Management of mild chronic hypertension
In pregnant women with mild hypertension and no evidence of renal disease, serious complications are rare and antihypertensive medication usually is not necessary. Nonpharmacologic therapy includes a healthy diet, moderate exercise and avoidance of alcohol, tobacco and medications that increase blood pressure. A practical management algorithm is summarized in Figure 35.1. Prenatal visits are scheduled every 2–4 weeks until 34–36 weeks, and weekly thereafter. At each visit, blood pressure, urine protein and fundal height are evaluated. Patients are questioned regarding signs and symptoms of pre-eclampsia, including headache, abdominal pain, blurred vision, scotomata, rapid weight gain or marked swelling of the hands and/or face. Antepartum fetal monitoring usually is started around 32–34 weeks and in most cases, delivery is no later than 40 weeks.
Management of severe chronic hypertension
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree