Chapter 46 Hypertension
ETIOLOGY
What Is Hypertension in a Child?
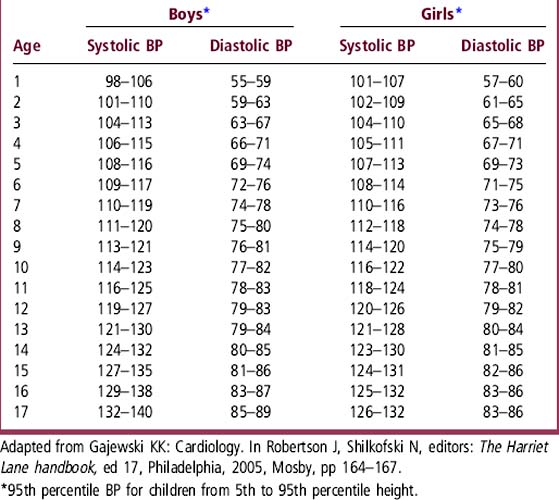
Ideally, blood pressure (BP) should be less than the 90th percentile for age. Hypertension is defined as BP that is above the 95th percentile for the child’s age, gender, and height, measured on at least three separate occasions. For example, a 4-year-old boy with BP 120/80 mm Hg is above this cut-off: Even if his height is at the 95th percentile, his BP should not be above 115/71 mm Hg. (See Table 46-1 for the 95th percentile ranges of BP for children between the 5th and 95th percentiles for height.) For complete tables of BP values in children see www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm or Pediatrics 114:555, 2004.
What Causes Hypertension in a Child?
In some children and in most adults, elevated BP that does not result from identifiable pathology in a single organ system is labeled primary hypertension (formerly called “essential”). Hypertension that results from a pathologic process in one organ or organ system is labeled secondary hypertension. BP elevation also may be caused by medications, such as over-the-counter cold preparations, which often are vasoconstrictors. Acute elevations in BP may be seen with emotional or physical stress, including that associated with a visit to a physician’s office (“white-coat” hypertension). Systolic pressure may be elevated for a period after vigorous exercise, an important fact to consider in sports physical examinations. Transient elevations in BP are also common with smoking, alcohol or caffeine consumption, and the use of illicit drugs such as cocaine and amphetamines. These personal habits should be addressed routinely at health supervision visits for older children and adolescents and should be specifically included in the history designed to identify causes of elevated BP. Obesity is an important cause of hypertension that defies classification into a particular category. Elevated BPs can normalize with weight loss. Table 46-2 lists specific causes of hypertension.
Table 46-2 Causes of Hypertension in Children
| Primary hypertension |
| Secondary hypertension |
| Renal causes (80% of all secondary hypertension) |
| • Renal parenchymal diseases (80% of all renal causes) |
| • Acute and chronic renal failure |
| • Acute and chronic glomerulonephritis |
| • Renal scarring/reflux nephropathy |
| • Structural malformations: renal hypodysplasia, polycystic kidneys |
| • Tumors (rare as a cause of hypertension) |
| • Renovascular hypertension |
| • Fibromuscular dysplasia |
| • Neurofibromatosis |
| • Williams syndrome |
| Cardiac causes (10% of all secondary hypertension) |
| • Coarctation of the aorta |
| • Aortoarteritis (rare in North America) |
| Endocrine causes (2% of all secondary hypertension) |
| • Cushing disease |
| • Mineralocorticoid excess |
| • Conn syndrome, licorice ingestion, glucocorticoid use |
| • Congenital adrenal hyperplasia (certain subtypes) |
| • Syndrome of apparent mineralocorticoid excess |
| • Glucocorticoid-remediable aldosteronism |
| • Hypothyroidism and hyperthyroidism |
| • Pheochromocytoma (rare as a cause of hypertension in children) |
| Miscellaneous causes |
| • Central nervous system tumors or other space-occupying lesions |
| • Liddle syndrome |
| • Autonomic neuropathy (Guillain-Barré syndrome) |
| • Acute intermittent porphyria |
| • Stimulant use such as Ritalin |
EVALUATION
How Do I Start the Evaluation of Hypertension?
If the patient’s BP is persistently above the 95th percentile for age, gender, and height, the history and physical examination should search for possible causes of hypertension, evidence of end-organ damage, and comorbid conditions such as dyslipidemia, diabetes, and obesity. The laboratory workup should be based on the data obtained by history and physical examination (Table 46-3).
Table 46-3 Diagnostic Evaluation for Secondary Hypertension
| Causes of Hypertension | Clues from History, Physical Examination, and Screening Laboratory Tests | Imaging and Second-Line Tests |
|---|---|---|
| Renal parenchymal | ||
| Renal failure/GN | H/o oliguria, hematuria, proteinuria, edema, elevated serum creatinine | Renal ultrasound C3 and C4 complement |
| Renal scarring | H/o UTIs/unexplained fevers | DMSA renal scan/VCUG |
| Anatomic (polycystic kidneys) | Palpable kidneys Family history of renal disease | Renal ultrasound or CT |
| Renovascular | ||
| Renal artery thrombosis | H/o umbilical catheterization as neonate | Renal arteriogram (gold standard) |
| Fibromuscular dysplasia | Dysmorphic facies (Williams syndrome) Neurofibromas, axillary freckling, café au lait spots Abdominal bruits Hypokalemia Elevated plasma renin level | Alternative imaging (not standardized in children) Captopril renal scans MRA and Duplex ultrasound of renal arteries |
| Cardiac (coarctation) | Cardiac murmur BP elevated in arms | Chest radiograph and echocardiogram |
| Endocrine | ||
| Cushing disease | H/o exogenous steroid use, weight gain, acne, moon facies, abdominal striae Hyperglycemia | Elevated urine and serum cortisol |
| Conn syndrome | H/o muscle weakness Hypokalemia | Increased serum aldosterone |
| Congenital adrenal hyperplasia | H/o amenorrhea, hirsutism Ambiguous genitalia | Abnormal urinary corticosteroid profile |
| Pheochromocytoma | Episodes of flushing, palpitation, tremors, panic attacks, palpable abdominal mass | Urinary catecholamines |
| Thyroid abnormalities | Change in bowel habits, heat or cold intolerance, tremors Tachycardia, myxedema, exophthalmos | Thyroid function tests (T3, T4, and TSH) |
| GRA/AME | Family history of hypertension, hypokalemia Low plasma renin level | Abnormal urinary steroid profile: 18 oxo-cortisol (GRA), cortisol/cortisone metabolites (AME) |
AME, Apparent mineralocorticoid excess; BP, blood pressure; CT, computed tomography; DMSA, dimercaptosuccinic acid; GN, glomerulonephritis; GRA, glucocorticoid-remediable aldosteronism; H/o, history of; MRA, magnetic resonance angiography; T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone; UTI, urinary tract infection; VCUG, voiding cystourethrogram.
Further investigation will depend on factors unique to you and your patient:
• How significantly elevated is the BP? Is it life threatening?
 How difficult is it to control your patient’s BP medically?
How difficult is it to control your patient’s BP medically?
 What evidence do you have that your patient has a treatable cause of hypertension?
What evidence do you have that your patient has a treatable cause of hypertension?
 How aggressive do you and the family want to be in the workup?
How aggressive do you and the family want to be in the workup?
• What do you plan to do if you identify a specific cause for the hypertension?
 Do the benefits of investigation or treatment outweigh the risks?
Do the benefits of investigation or treatment outweigh the risks?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree