Chapter 27 HYPERTENSION
General Discussion
The most commonly used definitions of normal and abnormal BP in childhood come from the National High Blood Pressure Education Program Working Group. These definitions are endorsed in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Normal BP is defined as systolic and diastolic BP less than the 90th percentile for age and sex. High-normal BP is defined as average systolic or diastolic BP greater than or equal to the 90th percentile but less than the 95th percentile. Hypertension is defined as average systolic or diastolic readings greater than the 95th percentile based on age, gender, and height percentile (Tables 27-1 and 27-2). At least three abnormal readings, obtained on separate occasions over a period of several weeks, should be obtained before entertaining a diagnosis of hypertension in an individual patient. A separate set of BP percentile curves has been established for infants aged 0 to 12 months (Figures 27-1 and 27-2).
Table 27-1 90th and 95th Percentile Blood Pressures for Boys Aged 1 to 17 Years by Height Percentile
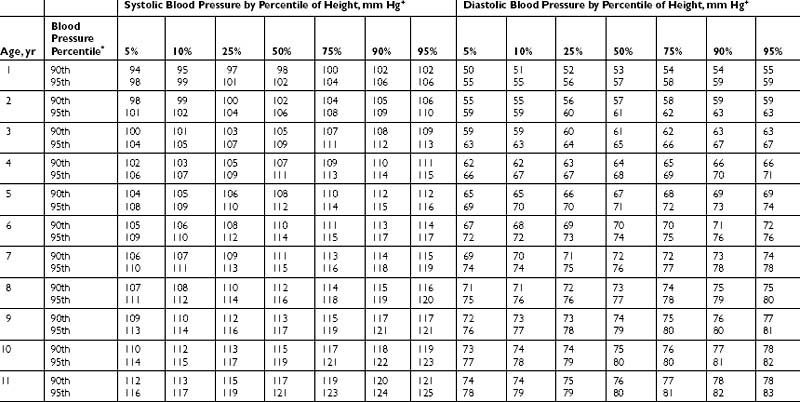
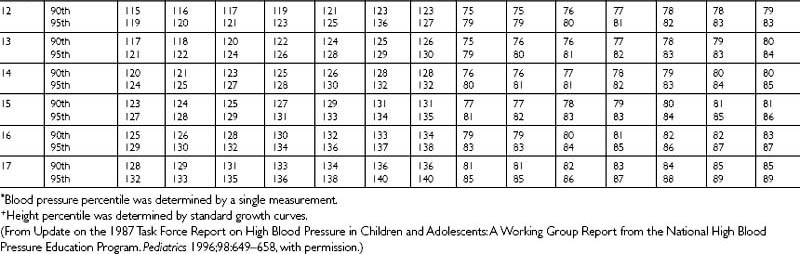
Table 27-2 90th and 95th Percentile Blood Pressures for Girls Aged 1 to 17 Years by Height Percentile.
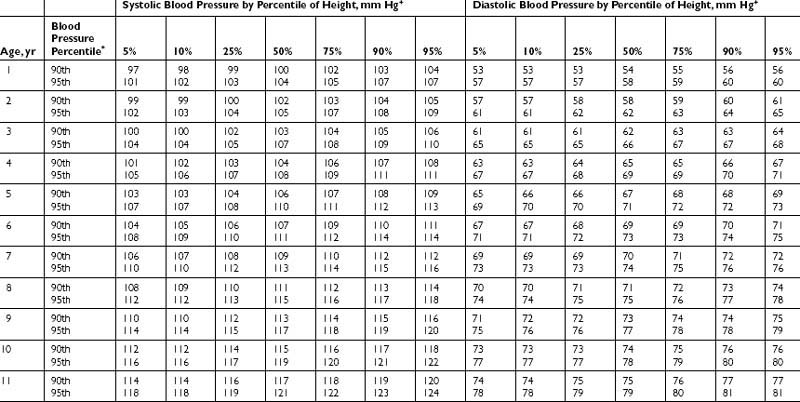
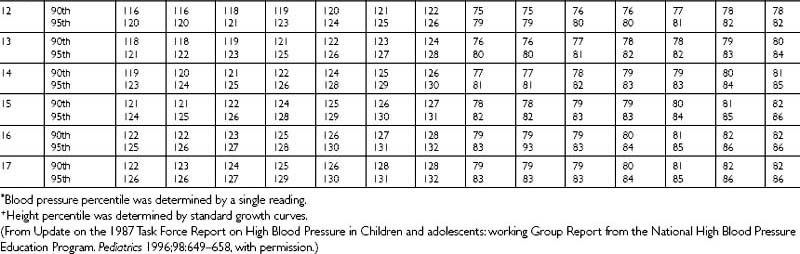
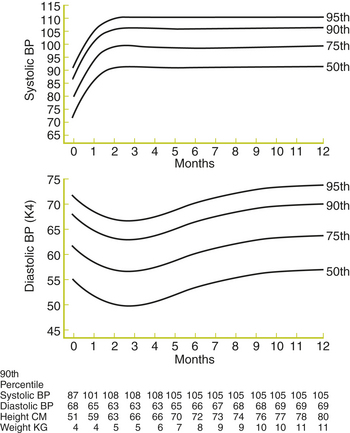
Figure 27-1 Age-specific percentiles of blood pressure measurements in boys—birth to 12 months of age.
(From Task Force on Blood Pressure Control in Children. Report of the second task force on blood pressure control in children—1987. Pediatrics 1987;79:1–25, with permission.)
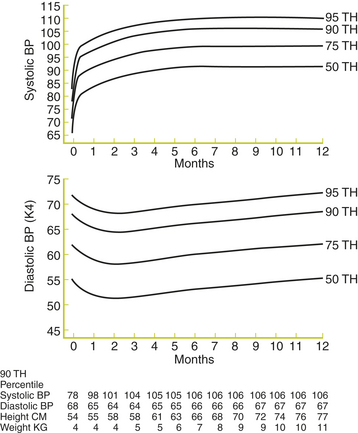
Figure 27-2 Age-specific percentiles of blood pressure measurements in girls—birth to 12 months of age.
(From Task Force on Blood Pressure Control in Children. Report of the second task force on blood pressure control in children—1987. Pediatrics 1987;79:1–25, with permission.)



