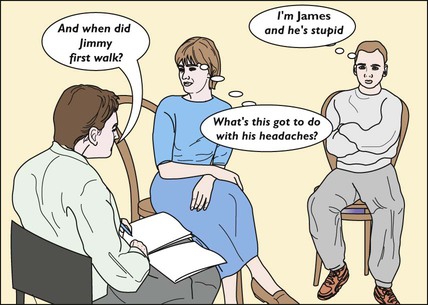
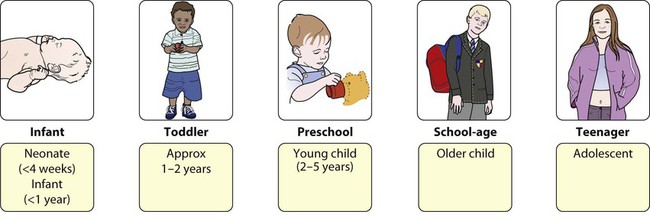
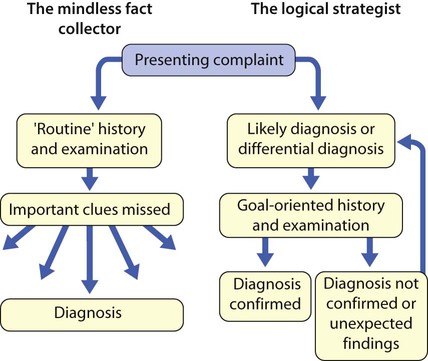
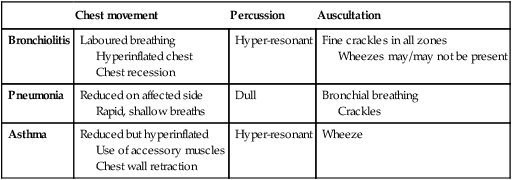
• An acute illness, e.g. respiratory tract infection, meningitis, appendicitis • A chronic problem, e.g. failure to thrive, chronic cough • A newborn infant with a congenital malformation or abnormality, e.g. developmental dysplasia of the hip, Down syndrome • Suspected delay in development, e.g. slow to walk, talk or acquire skills • Behaviour problems, e.g. temper tantrums, hyperactivity, eating disorders. The aims and objectives are to: • establish the relevant facts of the history; this is always the most fruitful source of diagnostic information • elicit all relevant clinical findings • collate the findings from the history and examination • formulate a working diagnosis or differential diagnosis on the basis of logical deduction The above can be summarised by the acronym HELP: Key points in paediatric history and examination are: • the child’s age – a key feature in the history and examination (Fig. 2.1) as it determines: – the nature and presentation of illnesses, developmental or behaviour problems – the way in which the history-taking (Fig. 2.2) and examination are conducted • the parents, who are astute observers of their children. Never ignore or dismiss what they say. • Make sure you have read any referral letter and scanned the notes before the start of the interview. • Observe the child at play in the waiting area and observe their appearance, behaviour and gait as they come into the clinic room. The continued observation of the child during the whole interview may provide important clues to the diagnosis and management. • When you welcome the child, parents and siblings, check that you know the child’s first name and gender. Ask how the child prefers to be addressed. • Determine the relationship of the adults to the child. • Establish eye contact and rapport with the family. Infants and some toddlers are most secure in parents’ arms or laps. Young children may need some time to get to know you. • Ensure that the interview environment is as welcoming and unthreatening as possible. Avoid having desks or beds between you and the family, but keep a comfortable distance. • Have toys available. Observe how the child separates, plays and interacts with any siblings present. • Do not forget to address questions to the child, when appropriate. • There will be occasions when the parents will not want the child present or when the child should be seen alone. This is usually to avoid embarrassing older children or teenagers or to impart sensitive information. This must be handled tactfully, often by negotiating to talk separately to each in turn. The scope and detail of further history-taking are determined by the nature and severity of the presenting complaint and the child’s age. While the comprehensive assessment listed here is sometimes required, usually a selective approach is more appropriate (Fig. 2.3). This is not an excuse for a short, slipshod history, but instead allows one to focus on the areas where a thorough, detailed history is required. • General rashes, fever (if measured) • Respiratory – cough, wheeze, breathing problems • ENT – throat infections, snoring, noisy breathing (stridor) • Cardiovascular – heart murmur, cyanosis, exercise tolerance • Gastrointestinal – vomiting, diarrhoea/constipation, abdominal pain • Genitourinary – dysuria, frequency, wetting, toilet-trained • Neurological – seizures, headaches, abnormal movements • Musculoskeletal – disturbance of gait, limb pain or swelling, other functional abnormalities. Make sure that you and the parent or child mean the same thing when describing a problem. • Maternal obstetric problems, delivery, prolonged rupture of membranes, group B streptococcus status, maternal pyrexia (pertinent if neonate) • Perinatal problems, whether admitted to special care baby unit, jaundice, etc. • Immunisations (ideally from the personal child health record) • Past illnesses, hospital admissions and operations, accidents and injuries. • Relevant information about the family and its community – parental occupation, economic status, housing, relationships, parental smoking, marital stresses. • Is the child happy at home? What are the child’s preferred play or leisure activities? • Is the child happy at nursery/school? • Parental worries about vision, hearing, development • Key developmental milestones (Fig. 2.4) • Previous child health surveillance developmental checks • Child’s temperament, behaviour • Make friends with the child. • Short mock examinations, e.g. auscultating a teddy or the mother’s hand, may allay a young child’s fears. • When first examining a young child, start at a non-threatening area, such as a hand or knee. • Explain what you are about to do and what you want the child to do, in language he can understand. As the examination is essential, not optional, it is best not to ask his permission, as it may well be refused! • A smiling, talking doctor appears less threatening, but this should not be overdone as it can interfere with one’s relationship with the parents. • Babies in the first few months are best examined on an examination couch with a parent next to them. • A toddler is best initially examined on his mother’s lap or occasionally over a parent’s shoulder. • Parents are reassuring for the child and helpful in facilitating the examination if guided as to what to do (Fig. 2.5). • Preschool children may initially be examined while they are playing. • Older children and teenagers are often concerned about privacy. Teenage girls should normally be examined in the presence of their mother, or a nurse or suitable chaperone. Be aware of cultural sensitivities in different ethnic groups. A good overview of developmental skills can be obtained by watching the child play. A few simple toys, such as some bricks, a car, doll, ball, pencil and paper, pegboard, miniature toys and a picture book, are all that is required, as they can be adapted for any age. If developmental assessment (see Ch. 3) is the focus of the examination, it is advisable to assess this before the physical examination, as cooperation may then be lost.
History and examination
Taking a history
Introduction
Presenting symptoms
Systems review
Past medical history
Social history
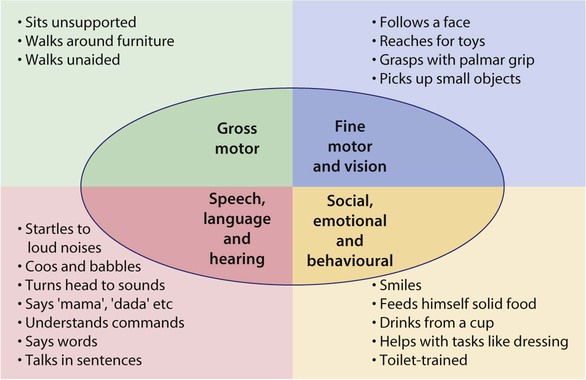
Development
An approach to examining children
Obtaining the child’s cooperation
Adapting to the child’s age
Developmental skills
Examination
Initial observations