CHAPTER 26 Hirsutism and virilization
Introduction
Hair follicles are stimulated by androgens to either enlarge on the face and body or to shrink on the vertex of the scalp. These changes occur in the female after puberty and probably develop to a small extent in all women. A small number of women develop excessive changes in hair, prompting advice from beauty therapists or physicians. The heaviness of facial or body hair growth that is necessary for a woman to consider herself to be hirsute is dependent on racial, cultural, social and economic factors. Although the pattern of hair growth is similar in all races, there is a variation in the heaviness of growth between ethnic groups. Furthermore, Shah (1957) in India and Lunde and Grottum (1984) in Norway have both stressed that women are more likely to consider themselves to be hirsute if they have significant growth on the upper lip, chin, chest and upper back.
The problem with defining hirsutism is that all measurements are subjective (Barth 1997). Large studies of unselected women in the USA (DeUgarte et al 2006) and Scandinavia (Lunde and Grottum 1984) have shown that it is impossible to separate hirsute from non-hirsute women on the basis of hair scoring scales, as women with similar hair scores may or may not consider that they have excessive hair growth. The problem with physician scales is that they do not consider the effect of hair localization. Is a women with facial hair but no body and limb hair more or less hirsute than a woman with a hairless face but a hairy trunk and limbs?
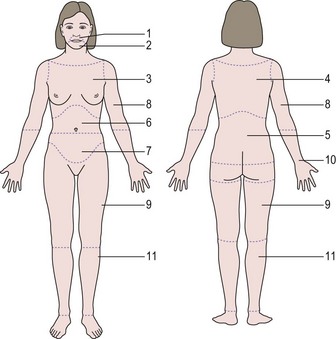
The standard scoring scale designed by Ferriman and Gallwey (1961) (Figure 26.1) defined 1.2% of females as hirsute, but this was based purely on mathematical grounds (i.e. 2 standard deviations from the mean). This contrasts with women’s perspectives. A study of 400 unselected students, 60% of whom were Welsh, showed that 9% considered themselves to be disfigured by their facial hair growth (McKnight 1964). A study of unselected women in the USA found that approximately 20% of women had modified Ferriman and Gallwey scores greater than 3, and of these women, 70% considered themselves to have excessive facial and body hair. Furthermore, women with hirsutism give their hair growth a higher score than their physicians (Kozloviene et al 2005).
Hirsuties or hypertrichosis?
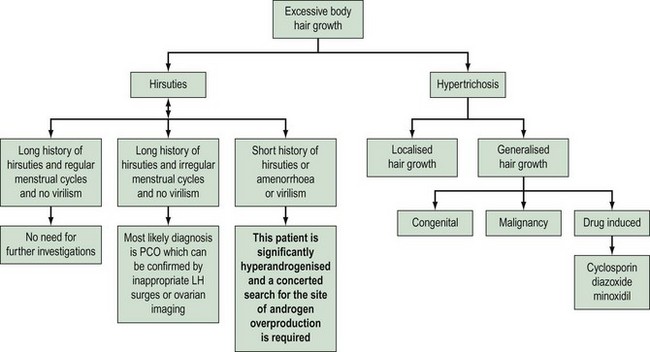
Hypertrichosis needs to be differentiated as it is not androgen mediated and therefore does not respond to antiandrogen therapy. The onset of hair growth is not related to puberty; there is no hair growth pattern but there is a uniform diffuse growth of hair over the body. The individual hair shafts tend to be finer and lie flat against the skin, rather than being coarse, curly and rising above the skin surface. Hypertrichosis may be congenital or acquired due to drug therapy and some metabolic disorders (Table 26.1).
Table 26.1 Aetiology of hirsuties and hypertrichosis
| Causes of hirsutism | Causes of hypertrichosis |
|---|---|
Congenital disorders, e.g. hypertrichosis lanuginosa and other syndromes often associated with mental retardation |
PCO, polycystic ovaries.
Investigation
Diagnostic approach to the hirsute woman
What is the evidence for this approach?
Moran et al (1994) reported on 250 premenopausal (<38 years) women presenting with various symptoms who were noted to be hirsute. Ninety-six percent were diagnosed with polycystic ovaries, idiopathic hirsuties or obesity; 2% were diagnosed with congenital adrenal hyperplasia (CAH); and 1.6% were either iatrogenic (one case) or due to an ovarian tumour (two cases) or Cushing’s syndrome (one case).
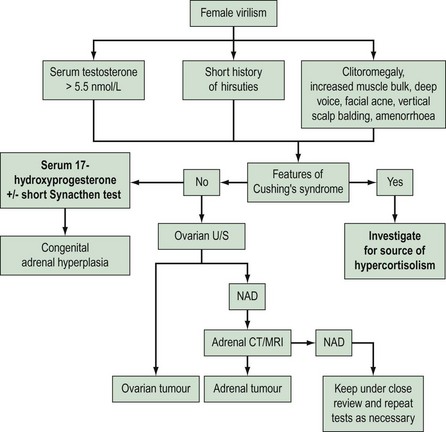
O’Driscoll et al (1994) reported a series of 350 consecutive patients who had presented with either hirsuties or androgenic alopecia. They identified eight women from this series with clear endocrine diseases; two had pituitary tumours (prolactinoma and acromegaly). The others were identified by a grossly elevated serum testosterone (>5 nmol/l). In total, 13 women had elevated testosterone; six had polycystic ovaries, two had late-onset CAH, one had virilizing CAH that had been ignored in childhood, one had an adrenal carcinoma, one had a postmenopausal Leydig cell tumour, one had corticosteroid 11-reductase deficiency, and the diagnosis in one hyperandrogenized postmenopausal woman was not elucidated. On the basis of the clinical details given in the report, only two diagnoses of late-onset CAH would have been missed by clinical evaluation alone (one had regular cycles and two children, the other had a long history of oligomenorrhoea; both had polycystic ovaries on ultrasound examination).
Arguably, the most important purpose for investigation is to identify those women with androgen-secreting tumours, since they require different therapy. Derksen et al (1994) reported a series of two adrenal adenomas and 12 carcinomas in which hirsutism was the presenting symptom. The women with adenomas were described as being severely virilized. Six of the women with carcinoma had clinical signs of Cushing’s syndrome; of the remaining six cases, four were severely virilized and the other two women presented with abdominal pain.
Functioning ovarian tumours which secrete androgens and therefore cause virilization are rare and represent only 1% of all ovarian tumours. In these cases, hirsuties is a nearly universal feature. Amenorrhoea develops rapidly in all premenopausal patients, and systemic virilization with alopecia, cliteromegaly, deepening of the voice and a male habitus develops in approximately half of patients. Meldrum and Abraham (1979) reviewed the literature of 43 women with virilizing ovarian tumours; seven had a serum testosterone level below 7.0 nmol/l but all were clinically virilized, and one 65-year-old woman was reported as not virilized but her serum testosterone level was more than 12 nmol/l.
In conclusion, the vast majority of hirsute women have polycystic ovaries, and those women with androgen-secreting tumours can be identified by clinical evaluation and a single serum testosterone estimation (Figure 26.3).
How Useful Are Endocrine Tests?
The laboratory findings in reports of hirsute women demonstrate considerable heterogeneity. This may be due to differences in diagnostic criteria for the studies; for example, hyperandrogenaemia, acne and/or hirsutism, or women with polycystic ovaries/menstrual disturbances. A further factor may be the degree of hair growth necessary to define whether a woman is considered to be hirsute (Barth et al 2007). A third point has been proposed by Toscano et al (1983) who suggested that the endocrine abnormalities are dependent on the length of the history of hirsutism. They posed the question ‘is hirsutism an evolving syndrome?’, and whilst their interpretation of the findings may be argued, it is clear that (i) a degree of hirsutism and/or oligomenorrhoea is necessary before hormonal abnormalities may be present, and (ii) not all hirsute women have abnormal circulating hormones.
Investigations to diagnose polycystic ovaries
Ovarian imaging compares extremely favourably with anatomical appearance in those subjects who have had abdominal laparoscopy, whereas the use of gonadotrophins is less well established as a diagnostic tool. Approximately 50% of women with polycystic ovaries have an elevated concentration of luteinizing hormone (LH), and 40% of women with elevated LH have polycystic ovaries. The use of gonadotrophins is further complicated by assay methodology. In view of these factors, the latest guidelines to diagnose polycystic ovaries have abandoned their use (Rotterdam ESHRE/ASRM-sponsored PCOS Consensus Workshop Group 2004). The over-riding problem is that approximately 10% of women with ultrasound-diagnosed polycystic ovaries will have normal endocrine tests, however many are performed. This may be due to the relationship between body weight and the dynamics of testosterone production (Figure 26.4).
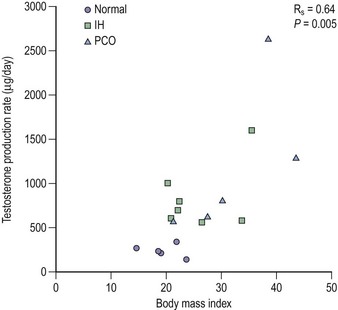
Figure 26.4 Although serum testosterone is usually reported as slightly elevated in women with polycystic ovaries (PCO) or hirsuties, it can be seen from this redrawing of the original data of Bardin and Lipsett (1967) that testosterone production rates are closely related to body mass irrespective of the patient’s phenotype. IH, idiopathic hirsuties.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree