Chapter 89 High-Risk Pregnancies
High-risk pregnancies are those that increase the likelihood of abortion, fetal death, premature delivery, intrauterine growth restriction, poor cardiopulmonary or metabolic transitioning at birth, fetal or neonatal disease, congenital malformations, mental retardation, or other handicaps (see Table 89-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ; Chapter 90). Some factors, such as ingestion of a teratogenic drug in the 1st trimester, are causally related to the risk; others, such as hydramnios, are associations that alert a physician to determine the etiology and avoid the inherent risks associated with excessive amniotic fluid. On the basis of their history, 10-20% of pregnant women can be identified as being at high risk; nearly half of all perinatal mortality and morbidity is associated with these high-risk pregnancies. Although assessing antepartum risk is important in reducing perinatal mortality and morbidity, some pregnancies become high risk only during labor and delivery; therefore, careful monitoring is critical throughout the intrapartum course.
; Chapter 90). Some factors, such as ingestion of a teratogenic drug in the 1st trimester, are causally related to the risk; others, such as hydramnios, are associations that alert a physician to determine the etiology and avoid the inherent risks associated with excessive amniotic fluid. On the basis of their history, 10-20% of pregnant women can be identified as being at high risk; nearly half of all perinatal mortality and morbidity is associated with these high-risk pregnancies. Although assessing antepartum risk is important in reducing perinatal mortality and morbidity, some pregnancies become high risk only during labor and delivery; therefore, careful monitoring is critical throughout the intrapartum course.
Table 89-1 FACTORS ASSOCIATED WITH HIGH-RISK PREGNANCY
ECONOMIC
CULTURAL-BEHAVIORAL
BIOLOGIC-GENETIC
REPRODUCTIVE
MEDICAL
Maternal Factors
The lowest neonatal mortality rate occurs in infants of mothers who receive adequate prenatal care and who are 20-30 yr of age. Pregnancies in both teenagers and women older than 40 yr, particularly primiparous women, are at increased risk for intrauterine growth restriction, fetal distress, and intrauterine death. Advanced maternal age increases the risk of both chromosomal and nonchromosomal fetal malformations (Fig. 89-1).
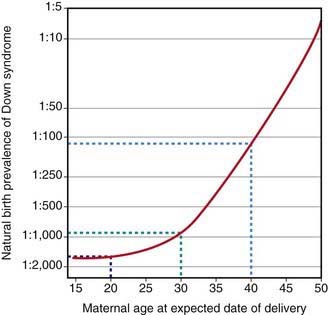
Figure 89-1 Natural birth prevalence of Down syndrome according to maternal age.
(From Wald NJ, Leck I: Antenatal and neonatal screening, ed 2, Oxford, 2000, Oxford University Press.)
Maternal illness (Table 89-2), multiple pregnancies (particularly those involving monochorionic twinning), infections (Table 89-3), and certain drugs (Chapter 90) increase the risk for the fetus. The use of assisted reproductive technology (in vitro fertilization, intracytoplasmic sperm injection) increases the risk of perinatal mortality, infant morbidity, prematurity, low and very low birthweight, and cerebral palsy, largely because of the increase in multiple-fetus pregnancies with such technology; the risks for birth defects are also increased, in part, because of epigenetic effects on gene expression.
Table 89-2 MATERNAL CONDITIONS AFFECTING THE FETUS OR NEONATE
| DISORDER | EFFECT(S) | MECHANISM(S) |
|---|---|---|
| Autoantibody against folate receptors | Neural tube defects | Blockage of cellular uptake of folate |
| Cervical neoplasia | Preterm premature rupture of membranes | Associated with loop electrosurgical excision procedure or cone therapy |
| Cholestasis | Preterm delivery, intrauterine fetal demise | Unknown, possibly hepatitis E |
| Cyanotic heart disease | Intrauterine growth restriction | Low fetal oxygen delivery |
| Diabetes mellitus: | ||
| Mild | Large for gestational age, hypoglycemia | Fetal hyperglycemia—produces hyperinsulinemia; insulin promotes growth |
| Severe | Growth restriction | Vascular disease, placental insufficiency |
| Drug addiction | Intrauterine growth restriction, neonatal withdrawal | Direct drug effect plus poor diet |
| Endemic goiter | Hypothyroidism | Iodine deficiency |
| Graves disease | Transient neonatal thyrotoxicosis | Placental immunoglobulin passage of thyroid-stimulating antibody |
| Herpes gestationis (noninfectious) | Bullous rash, intrauterine fetal demise | Unknown |
| Hyperparathyroidism | Neonatal hypocalcemia | Maternal calcium crosses to fetus and suppresses fetal parathyroid gland |
| Hypertension | Intrauterine growth restriction, intrauterine fetal demise | Placental insufficiency, fetal hypoxia |
| Idiopathic thrombocytopenic purpura | Thrombocytopenia | Nonspecific maternal platelet antibodies cross placenta |
| Isoimmune neutropenia or thrombocytopenia | Neutropenia or thrombocytopenia | Specific antifetus neutrophil or platelet antibody crosses placenta after sensitization of mother |
| Malignant melanoma | Placental or fetal tumor | Metastasis |
| Myasthenia gravis | Transient neonatal myasthenia | Immunoglobulin to acetylcholine receptor crosses placenta |
| Myotonic dystrophy | Neonatal myotonic dystrophy, congenital contractures, respiratory insufficiency | Genetic anticipation |
| Obesity | Macrosomia, hypoglycemia | Unknown |
| Phenylketonuria | Microcephaly, retardation | Elevated fetal phenylalanine values |
| Poor nutrition | ||



