Chapter 23 HEMATURIA, MICROSCOPIC
Asymptomatic isolated microscopic hematuria is common in children. Many experts recommend observation of these children if the examination is normal, with further evaluation only if proteinuria, hypertension, or gross hematuria is present. In the child with asymptomatic isolated microscopic hematuria, the early morning urinalysis should be repeated weekly for 2 weeks with no exercise before the collection of the urine sample. If the hematuria persists, urine culture should be obtained and, if positive, the patient should be treated with antibiotics. If the urine culture is negative, the patient should be followed up every 3 months with a history, physical examination, blood pressure measurement, and urinalysis. If the hematuria persists for 1 year, measurement of the urine calcium-creatinine ratio should be obtained, and the parents and siblings should be tested for hematuria. Hemoglobin electrophoresis should be performed if sickle cell trait is a consideration. Figure 23-1 provides an algorithm for the evaluation of a child with asymptomatic microscopic hematuria.
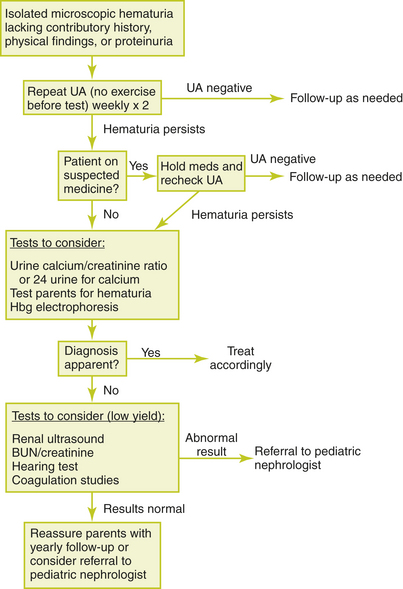
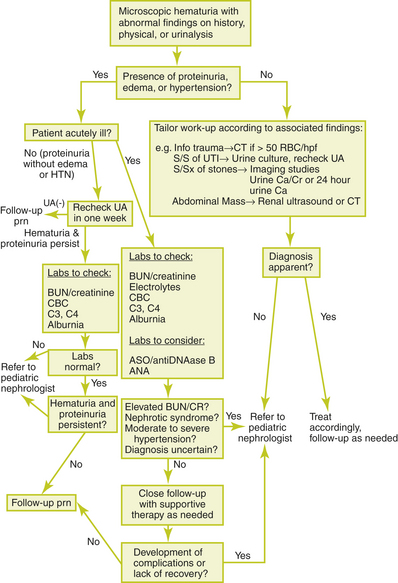
Figure 23-1 Evaluation of a child with asymptomatic microscopic hematuria.
(From Patel HP, Bissler JJ. Hematuria in children. Pediatr Clin North Am 2001;48:1519–1537, with permission.)
Asymptomatic microscopic hematuria with proteinuria is associated with a higher risk for significant renal disease. In this case, urinary protein excretion should be quantified. If protein excretion is greater than 4 mg/m2 per hour or the urine protein-to-creatinine ratio is greater than 0.2 mg protein per milligram of creatinine in children older than 2 years or greater than 0.5 mg of protein per milligram of creatinine in younger children, the patient should be referred to a pediatric nephrologist. If urinary protein excretion is less than these values, the patient should be reevaluated in a few weeks. If the hematuria and proteinuria have resolved, no further evaluation is indicated. If there is only asymptomatic microscopic hematuria, the patient may be monitored as for asymptomatic isolated microscopic hematuria. If the hematuria and proteinuria persist, the patient should be referred to a pediatric nephrologist. Additional testing is outlined below. Figure 23-2 provides an algorithm for the evaluation of a child with microscopic hematuria associated with proteinuria, symptoms, or abnormalities in history or physics examination.