46 Heart Failure
Etiology And Presentation
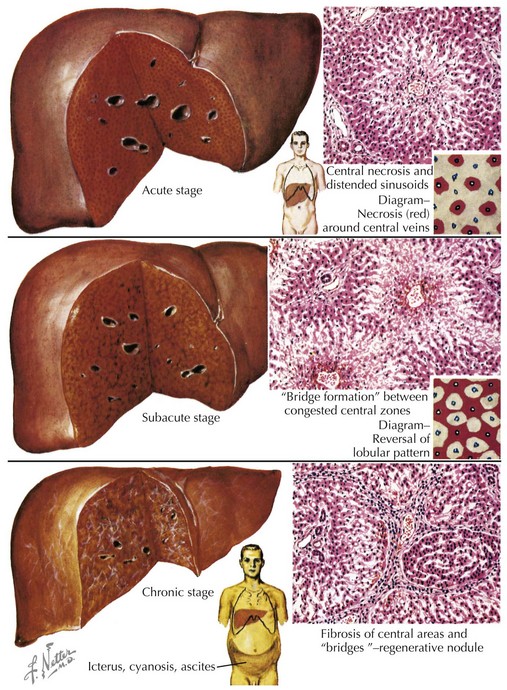
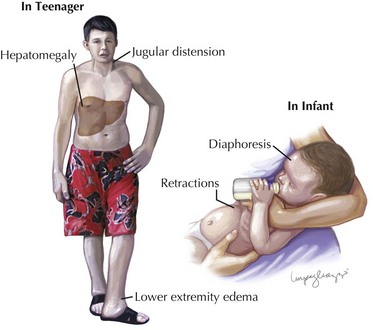
When the heart fails to adequately pump blood forward for any reason, venous congestion occurs. On the right side, the liver in particular becomes distended and engorged with blood. This leads to abdominal discomfort or vomiting initially, but in certain prolonged cases, it may lead to liver dysfunction and distension of venous collaterals, some of which may be visible under the skin (Figure 46-1). The signs of peripheral edema and jugular venous distension (Figure 46-2, left), classically seen in adults are not typically seen in infants or young children. On the left side, pulmonary venous congestion leads to fluid extravasation within the lungs, typically interstitial in infants and intraalveolar in older children and adults (Figure 46-2, right). This leads to shortness of breath, tachypnea, and dyspnea and can present on chest radiography similar to pneumonia. Indeed, in some cases, a secondary infection may develop superimposed on these wet and stiff lungs.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree