25
Haematology
Chapter map
Anaemia is quite common in childhood, and you should know the main differentials and be able to sensibly assess a patient. Coagulation disorders are less common, and sometimes present as purpura: know the important differential diagnoses.
25.1 The normal blood picture (Table 25.1)
25.2.1 Impaired production of red cells
25.3.1 Haemophilia (Table 25.2)
25.3.3 Disseminated intravascular coagulation (DIC, consumption coagulopathy)
25.1 The normal blood picture (Table 25.1)
Table 25.1 Normal blood picture
| Age | Haemoglobin (g/dL) | Type |
| Birth | 17 | HbF > HbA |
| 1 year | 12 | HbA |
| 12 years | 14 | HbA |
Newborn infants at term have a haemoglobin of 17 g/dL (range 14–20) and a high mean cell volume (MCV). This falls until 3 months because of limited erythropoiesis and red cell survival.
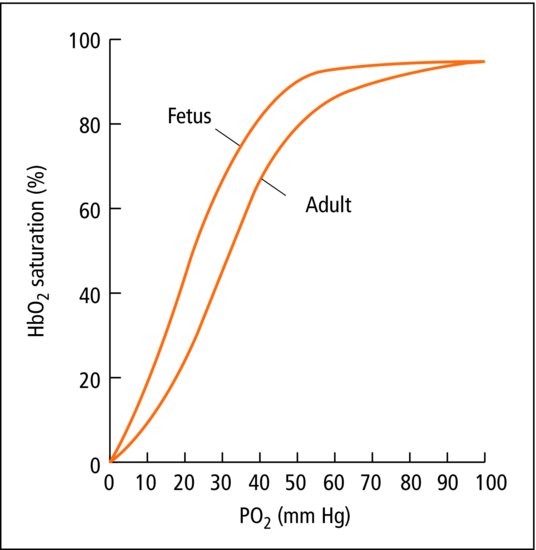
The fetus and newborn have fetal haemoglobin – HbF. HbF is gradually replaced by HbA (adult) (Figure 25.1). Children have a high white cell count and lymphocyte count, particularly in the first year. Infection often provokes a marked neutrophil leukocytosis with immature white cells pouring out of the marrow. In infants, bacterial infection may produce a lymphocytic response. The platelet count is slightly reduced in the first months.
Figure 25.1 Fetal and adult oxyhaemoglobin dissociation curves. The fetus achieves a higher oxygen saturation at lower Pao2. A small drop in Pao2 will result in release of a large amount of oxygen to the tissues.
25.2 Anaemia
Anaemia is common in childhood, but does not usually lead to symptoms. Pallor is common and often not related to anaemia. Anaemia may cause tiredness and even breathlessness, but most tired children are not anaemic.
- Impaired production of red cells
- Excessive breakdown of red cells
- Blood loss.
 PRACTICE POINT Clinical approach to anaemia
PRACTICE POINT Clinical approach to anaemia- Dietary iron (consider dietetic assessment)
- Blood loss (e.g. periods)
- Malabsorption/diarrhoea
- Chronic illness
- Family history and ethnicity (inherited red cell disorders)
- Growth/failure to thrive
- Signs associated with anaemia (angular cheilosis, koilonychia)
- Jaundice (haemolysis)
- Lymphadenopathy, hepatosplenomegaly, bruising (leukaemia)
- Abdominal distension (malabsorption, coeliac)
- Signs of chronic illness e.g. clubbing
- FBC with red cell indices and film (cells small, pale in iron deficiency, large in B12/folate deficiency)
- Reticulocytes (low in iron deficiency, rise within a few days of iron treatment; raised in haemolysis)
- Markers of iron deficiency (e.g. % hypochromic cells increased, low ferritin)
- Depending on clinical findings and results, consider haemoglobin electrophoresis, tests for haemolysis, other haematinics (folate, B12) and coeliac screen
- Depends on cause; for iron deficiency anaemia treat with iron medication, attend to diet.
25.2.1 Impaired production of red cells
25.2.1.1 Deficiency anaemias
Iron-deficiency anaemia is by far the most common, with a hypochromic microcytic blood picture. MCV is low. It is usually dietary, but may occur because losses of iron or blood exceed intake. Iron-deficiency anaemia is more common in the following:
- Preterm babies and twins (Section 8.2.8).
- Infants fed mainly cow’s milk who are late changing to iron-containing weaning foods – sometimes because the infant is late learning to chew solids, or simply prefers milk.
- Homes where poverty, ignorance or dietary restrictions prevent the child from receiving red meat, green vegetables, eggs and bread (which are the main sources of iron). Older infants and toddlers are most at risk.
- Chronic malabsorption such as coeliac disease (Section 21.2.5).
- Adolescent girls with rapid growth and menstrual losses.
 PRACTICE POINT
PRACTICE POINTPica, when children eat almost anything including soil or dirt, is associated with iron deficiency. Pica is the Latin name for magpie, a bird notorious for stealing and consuming almost anything. Other deficiency anaemias are uncommon. Folic acid deficiency is rare even in coeliac disease. Pernicious anaemia is extremely rare in children.
25.2.1.2 Bone marrow disturbance
Infiltration. Leukaemia (Section 26.1) is the most important. Secondary deposits from malignant tumours are less common. Aplastic anaemia may be drug related, post-viral (e.g. Epstein–Barr) or more commonly idiopathic.
25.2.1.3 Systemic disease
Chronic infection (e.g. cystic fibrosis), inflammatory disease (e.g. Crohn diease) and renal insufficiency depress haemopoiesis.
25.2.2 Excessive breakdown
Haemolytic anaemias are not common except in the newborn infant (Section 8.4.2.1). In paediatrics, haemolysis may have a cause specific to children or present mainly in childhood. Chronic or recurrent anaemia occurs with slight jaundice during periods of haemolysis. There is usually a reticulocytosis. If severe and sudden, it is called a ‘haemolytic crisis’: acute anaemia with jaundice, dark urine and dark stools seen. Splenomegaly is a feature of chronic cases.
25.2.2.1 Cellular abnormalities
These comprise abnormalities of red cell shape, red cell enzymes or haemoglobin structure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


