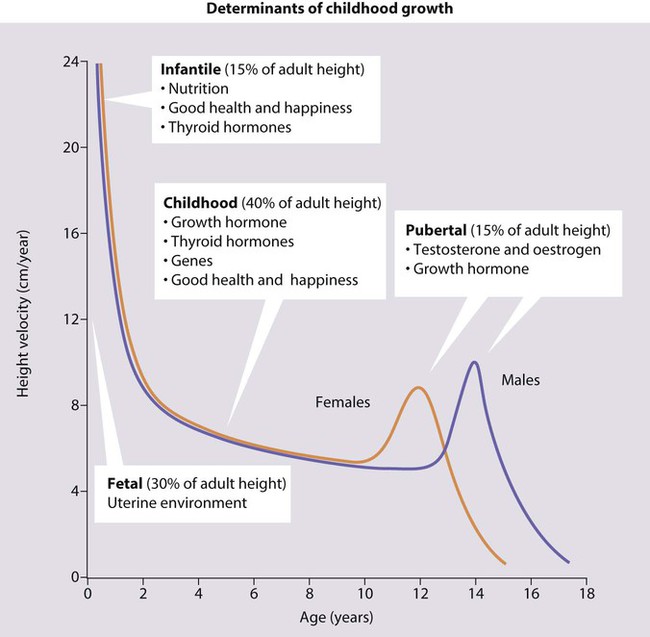
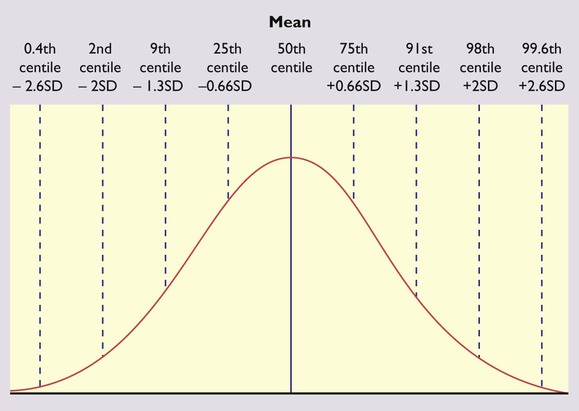
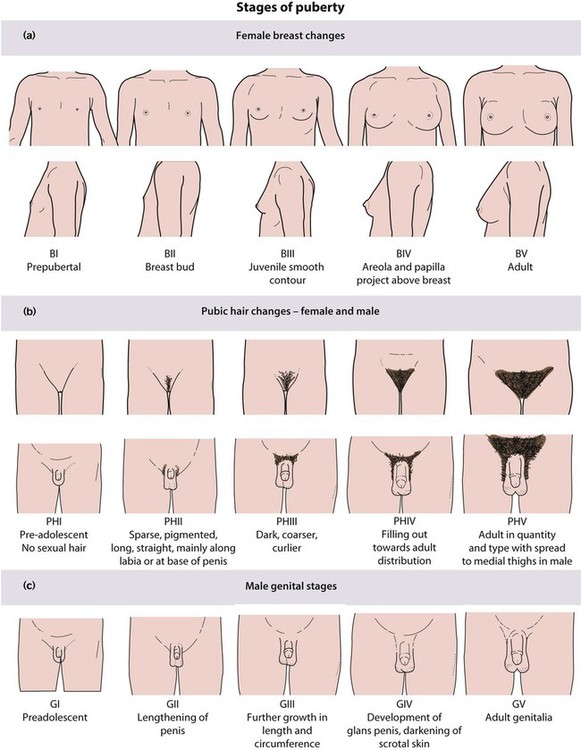
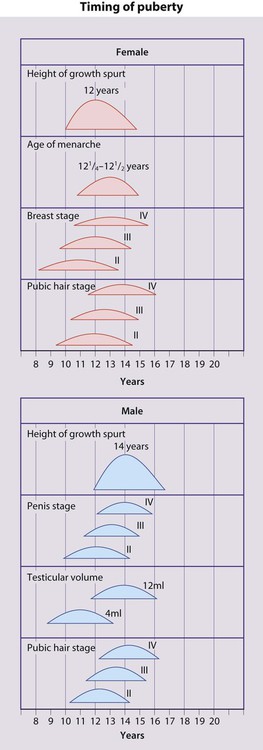
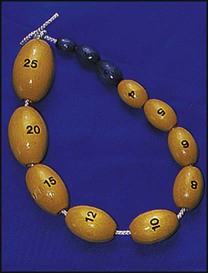
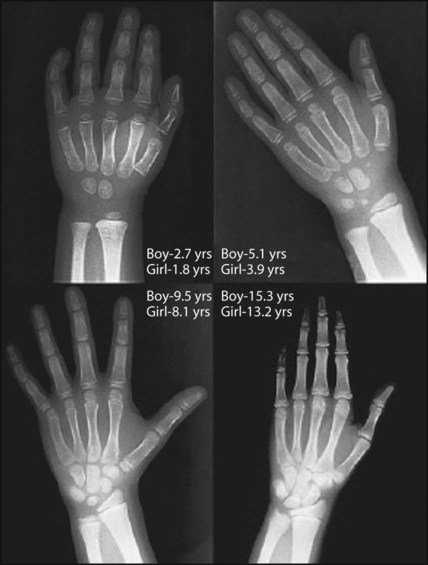
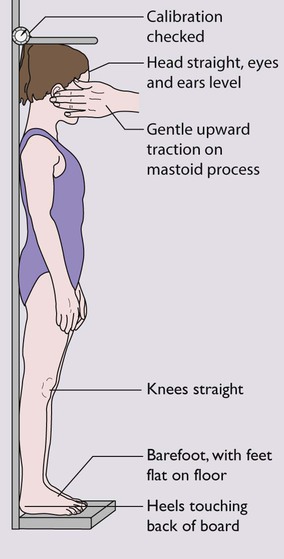
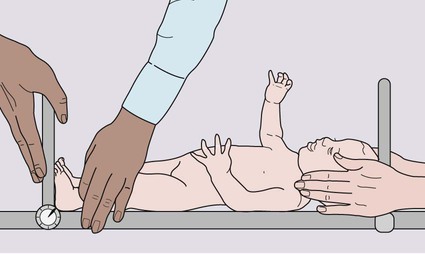
There are four phases of normal human growth (Fig. 11.1). Growth during infancy to around 18 months of age is also largely dependent on adequate nutrition. Good health and normal thyroid function are also necessary. This phase is characterised by a rapid but decelerating growth rate, and accounts for about 15% of eventual height. By the end of this phase, children have changed from their fetal length, largely determined by the uterine environment, to their genetically determined height. An inadequate rate of weight gain during this period is called ‘failure to thrive’ (see Ch. 12). • Weight – readily and accurately determined with electronic scales but must be performed on a naked infant or a child dressed only in underclothing as an entire month’s or year’s weight gain can be represented by a wet nappy or heavy jeans, respectively. • Height – the equipment must be regularly calibrated and maintained. In children over 2 years of age, the standing height is measured as illustrated in Figure 11.2. In children under 2 years, length is measured lying horizontally (Fig. 11.3), using the mother to assist. Accurate length measurement in infants can be difficult to obtain, as the legs need to be held straight and infants often dislike being held still. For this reason, routine measurement of length in infancy is often omitted from child surveillance, but it should always be performed whenever there is doubt about an infant’s growth. • Head circumference – the occipitofrontal circumference is a measure of head and hence brain growth. The maximum of three measurements is used. It is of particular importance in developmental delay or suspected hydrocephalus These measurements should be plotted as a simple dot on an appropriate growth centile chart. Standards for a population should be constructed and updated every generation to allow for the trend towards earlier puberty and taller adult stature from improved childhood nutrition. In 2009, the UK adopted the World Health Organization (WHO) new global Child Growth Standards for infants and children 0–4 years old (See Appendix Fig. A1). The new charts are based on the optimal growth of healthy children totally breast-fed up to the age of 6 months. These charts allow for the lower weight of totally breast-fed infants and are therefore less likely to identify some breast-fed babies as underweight and may also allow early identification of bottle-fed babies gaining weight too rapidly. Height in a population is normally distributed and the deviation from the mean can be measured as a centile or standard deviation (Fig. 11.4). The bands on the growth reference charts have been chosen to be two-thirds of a standard deviation apart and correspond approximately to the 25th, 9th, 2nd and 0.4th centiles below the mean, and the 75th, 91st, 98th and 99.6th centiles above the mean. The further these centiles lie from the mean, the more likely it is that a child has a pathological cause for his short or tall stature. For instance, values below the 0.4th or above the 99.6th centile will occur by chance in only 4 per 1000 children and can be used as a criterion for referral from primary to specialist care. A single growth parameter should not be assessed in isolation from the other growth parameters: e.g. a child’s low weight may be in proportion to the height if short, but abnormal if tall. Serial measurements are used to show the pattern and determine the rate of growth. This is helpful in diagnosing or monitoring many paediatric conditions. The WHO charts include an adult height predictor and a BMI centile ready-reckoner. Puberty follows a well-defined sequence of changes that may be assigned stages, as shown in Figures 11.5 and 11.6. Over the last 20 years, the mean age at which puberty starts in girls has lowered. However, the age at which menarche occurs has remained stable. Therefore, females now remain in puberty for longer. In females the features of puberty are: • Breast development – the first sign, usually starting between 8.5 and 12.5 years • Pubic hair growth and a rapid height spurt – occur almost immediately after breast development • Menarche – occurs on average 2.5 years after the start of puberty and signals that growth is coming to an end, with only around 5 cm height gain remaining. • Testicular enlargement to >4 ml volume measured using an orchidometer (Fig. 11.7) – the first sign of puberty • Pubic hair growth – follows testicular enlargement, usually between 10 and 14 years of age • Height spurt – when the testicular volume is 12–15 ml, after a delay of around 18 months. In both sexes, there will be development of acne, axillary hair, body odour and mood changes. If puberty is abnormally early or late, it can be further assessed: • Bone age measurement from a hand and wrist X-ray to determine skeletal maturation (Fig. 11.8) • In females, pelvic ultrasound can be used to assess uterine size and endometrial thickness. Short stature is usually defined as a height below the second centile (i.e. two standard deviations (SD) below the mean) or 0.4th centile (−2.6 SD). Only 1 in 50 children will be shorter than the 2nd centile and 1 in 250 (4 in 1000) shorter than the 0.4th centile. Most of these children will be normal, though short, with short parents, but the further the child is below these centiles, the more likely it is that there will be a pathological cause. However, the rate of growth (measured as height velocity; Fig. 11.1) may be abnormal long before a child’s height falls below these values. This growth failure can be identified from the child’s height falling across centile lines plotted on a height velocity chart (Fig. 11.1). This allows growth failure to be identified earlier, even though the child’s height is still above the 2nd centile. Measuring height velocity is a sensitive indicator of growth failure. Two accurate measurements at least 6 months but preferably a year apart allow calculation of height velocity in cm/year (Fig. 11.1). This is plotted at the midpoint in time on a height/velocity chart. A height velocity persistently below the 25th centile is abnormal and that child will eventually become short. A disadvantage of using height velocity calculations is that they are highly dependent on the accuracy of the height measurements and so tend not to be used outside specialist growth units. The height centile of a child must be compared with the weight centile and an estimate of their genetic target centile and range calculated from the height of their parents. This is calculated as the mean of the father’s and mother’s height with 7 cm added for the mid-parental target height of a boy, and 7 cm subtracted for a girl. The 9th–91st centile range of this estimate is given by ±10 cm in a boy and ±8.5 cm in a girl (see examples in Fig. 11.9). This is usually caused by autoimmune thyroiditis during childhood (see Ch. 25). This produces growth failure, usually with excess weight gain. It may go undiagnosed for many years and lead to short stature. When treated, catch-up growth rapidly occurs but often with a rapid entry into puberty that can limit final height. Congenital hypothyroidism is diagnosed soon after birth by screening and so does not result in any abnormality of growth. This is usually iatrogenic, as corticosteroid therapy is a potent growth suppressor. This effect is greatly reduced by alternate day therapy, but some growth suppression may be seen even with relatively low doses of inhaled or topical steroids in susceptible individuals. Non-iatrogenic Cushing syndrome is very unusual in childhood and may be caused by pituitary or adrenal pathology. Growth failure may be very severe, usually with excess weight gain, although normalisation of body shape and height occurs on withdrawal of treatment or treatment of the underlying steroid excess. Cushing syndrome during puberty can result in permanent loss of height (see Ch. 25).
Growth and puberty
The infantile phase
Measurement
Puberty
Short stature
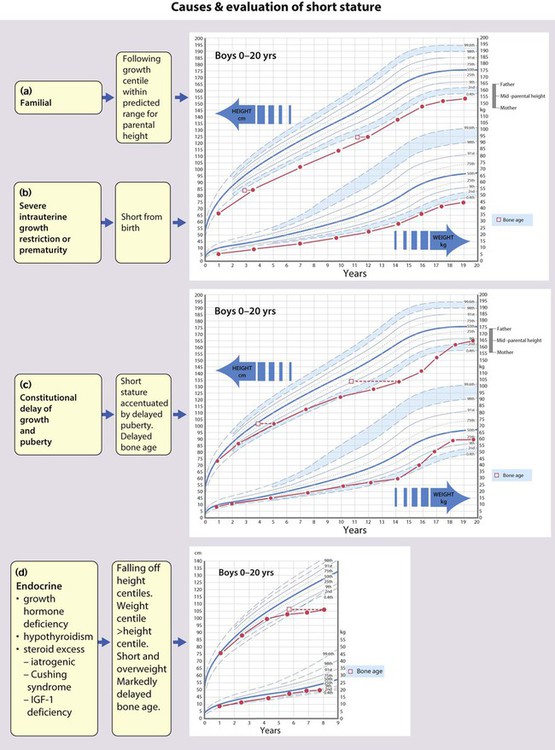
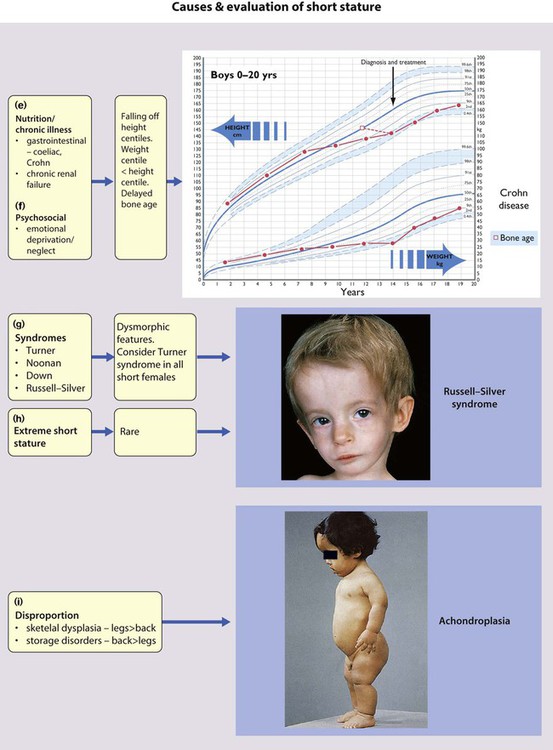
Endocrine
Hypothyroidism
Corticosteroid excess, Cushing syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Growth and puberty