30 Granulomatous Disease
Noninfectious granulomatous disease is rare in children, with the exception of Crohn disease (see Chapter 110). This group of diseases includes sarcoidosis, granulomatous vasculitides (Wegener granulomatosis [WG] and Churg-Strauss syndrome [CSS]), and familial juvenile systemic granulomatosis (Blau syndrome).
Sarcoidosis
Etiology and Pathogenesis
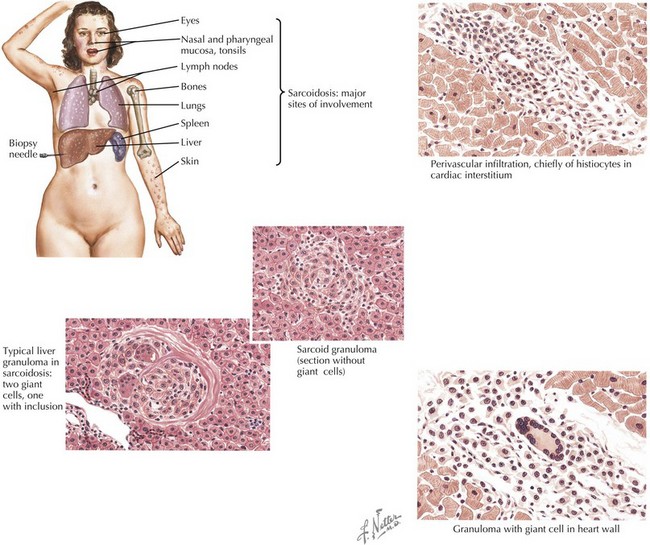
Sarcoidosis is characterized by granulomas consisting of tightly packed epithelioid cells and macrophages surrounded by lymphocytes (Figure 30-1). In the lung, CD4+ T cell-mediated alveolitis occurs early followed by granuloma formation. Granulomas may resolve without sequelae or may heal with residual fibrosis.
Clinical Presentation
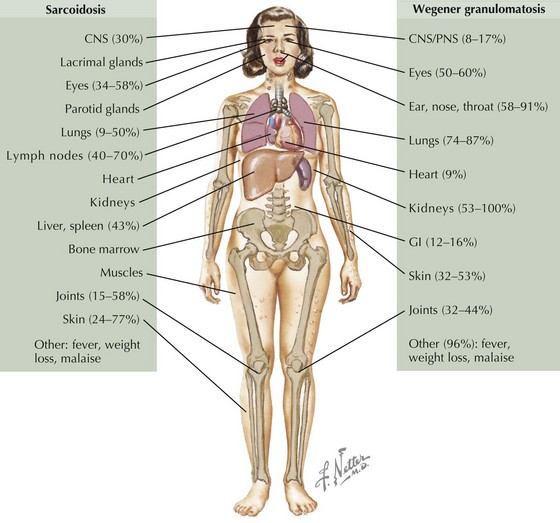
Sarcoidosis in children occurs in two distinct forms. Older children (age 8-15 years) typically present with symptoms resembling the adult form of disease, including lymphadenopathy, lung involvement (often asymptomatic), systemic signs (fever, weight loss), and hypercalcemia, but rarely with joint involvement. In children younger than 5 years, the onset typically consists of the triad of rash, arthritis, and uveitis. Sarcoidosis commonly presents with lymphadenopathy and may affect a wide range of organs (Figure 30-2).
Differential Diagnosis
Sarcoidosis should be considered in any child presenting with nonspecific findings, including fever, weight loss, and lymphadenopathy, especially if accompanied by rash, arthritis, or hilar adenopathy, or in any child with fever of unknown origin (see Chapter 86, Figure 86-1). Other conditions that must be considered in a child suspected of having sarcoidosis include infections, malignancies, and other rheumatic illnesses (vasculitides, systemic lupus erythematosus [SLE], mixed connective tissue disease [MCTD], Sjögren syndrome, juvenile idiopathic arthritis [JIA]). Hilar adenopathy with constitutional symptoms may mimic lymphoma. After granulomatous inflammation has been established, infections must be ruled out before initiation of immunosuppressive medications (Box 30-1).