Chapter 42 Gestational Trophoblastic Neoplasia
 Genetics of Gestational Trophoblastic Disease
Genetics of Gestational Trophoblastic Disease
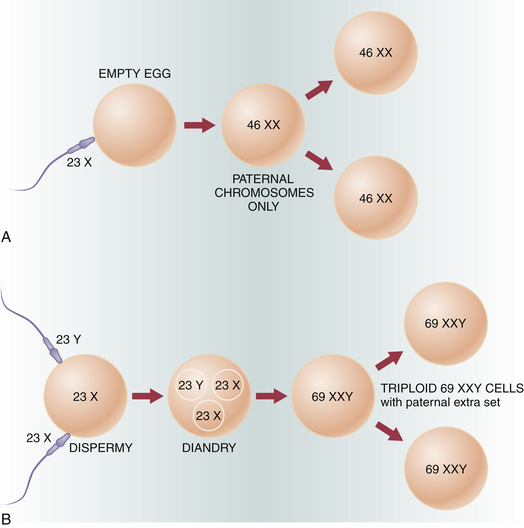
The cytogenetic analysis of tissue obtained from molar pregnancies offers some clue to the genesis of these lesions. Figure 42-1 illustrates the genetic composition of molar pregnancies.
 Classification
Classification
The term gestational trophoblastic neoplasia is of clinical value because often the diagnosis is made and therapy instituted without definitive knowledge of the precise histologic pattern. GTN may be benign or malignant and nonmetastatic or metastatic (Box 42-1).
Metastatic GTN can be subdivided into good prognosis and poor prognosis groups, depending on the sites of metastases and other clinical variables (Box 42-2).
 Pathologic Features
Pathologic Features
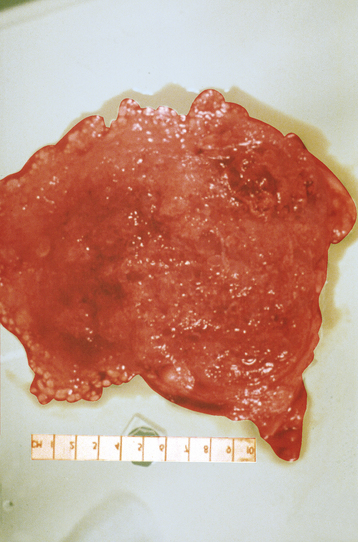
Grossly, a hydatidiform mole appears as multiple vesicles that have been classically described as a “bunch of grapes” (Figure 42-2). The characteristic histopathologic findings associated with a complete molar pregnancy are (1) hydropic villi, (2) absence of fetal blood vessels, and (3) hyperplasia of trophoblastic tissue (Figure 42-3). Invasive mole differs from hydatidiform mole only in its propensity to invade locally and to metastasize.
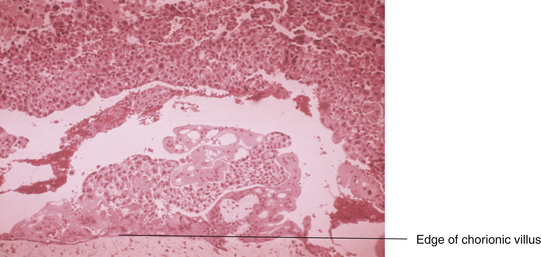
FIGURE 42-3 Histologic appearance of a complete hydatidiform mole. Note the marked trophoblastic proliferation.
 Hydatidiform Mole
Hydatidiform Mole
SYMPTOMS
Most patients with hydatidiform mole present with irregular or heavy vaginal bleeding during the first or early second trimester of pregnancy (Box 42-3). The bleeding is usually painless, although it can be associated with uterine contractions. In addition, the patient may expel molar “vesicles” from the vagina and occasionally may have excessive nausea, even hyperemesis gravidarum. Irritability, dizziness, and photophobia may occur because some patients experience preeclampsia. Patients may occasionally exhibit symptoms relating to hyperthyroidism, such as nervousness, anorexia, and tremors.
 Epidemiology and Etiology
Epidemiology and Etiology