FIGURE 20-1 Complete hydatidiform mole. A. Gross specimen with characteristic vesicles of variable size. (Image contributed by Dr. Brian Levenson.) B. Low-magnification photomicrograph shows generalized edema and cistern formation (black asterisks) within avascular villi. Haphazard trophoblastic hyperplasia is marked by a yellow asterisk on the right. (Image contributed by Dr. Erika Fong.)
A complete mole has abnormal chorionic villi that grossly appear as a mass of clear vesicles. These vary in size and often hang in clusters from thin pedicles. In contrast, a partial molar pregnancy has focal and less advanced hydatidiform changes and contains some fetal tissue. Although both forms of moles usually fill the uterine cavity, they rarely may be tubal or other forms of ectopic pregnancy (Sebire, 2005).
 Epidemiology and Risk Factors
Epidemiology and Risk Factors
There is an ethnic predisposition to hydatidiform mole, which has increased prevalence in Asians, Hispanics, and American Indians (Drake, 2006; Lee, 2011; Smith, 2006). The incidence in the United States and Europe has been relatively constant at 1 to 2 per 1000 deliveries (Lee, 2011; Lybol, 2011; Salehi, 2011).
The strongest risk factors are age and a history of prior hydatidiform mole. Women at both extremes of reproductive age are most vulnerable. Specifically, adolescents and women aged 36 to 40 years have a twofold risk, but those older than 40 have an almost tenfold risk (Altman, 2008; Sebire, 2002a). For those with a prior complete mole, the risk of another mole is 1.5 percent. With a previous partial mole, the rate is 2.7 percent (Garrett, 2008). After two prior molar pregnancies, Berkowitz and associates (1998) reported that 23 percent of women had a third mole.
 Pathogenesis
Pathogenesis
With rare exceptions, molar pregnancies arise from chromosomally abnormal fertilizations. Complete moles most often have a diploid chromosomal composition (Table 20-1). These usually are 46,XX and result from androgenesis, meaning both sets of chromosomes are paternal in origin. As shown in Figure 20-2A, an ovum is fertilized by a haploid sperm, which then duplicates its own chromosomes after meiosis. The chromosomes of the ovum are either absent or inactivated. Less commonly, the chromosomal pattern may be 46,XY or 46,XX and due to fertilization by two sperm, that is, dispermic fertilization or dispermy (Lawler, 1991; Lipata, 2010).
TABLE 20-1. Features of Partial and Complete Hydatidiform Moles
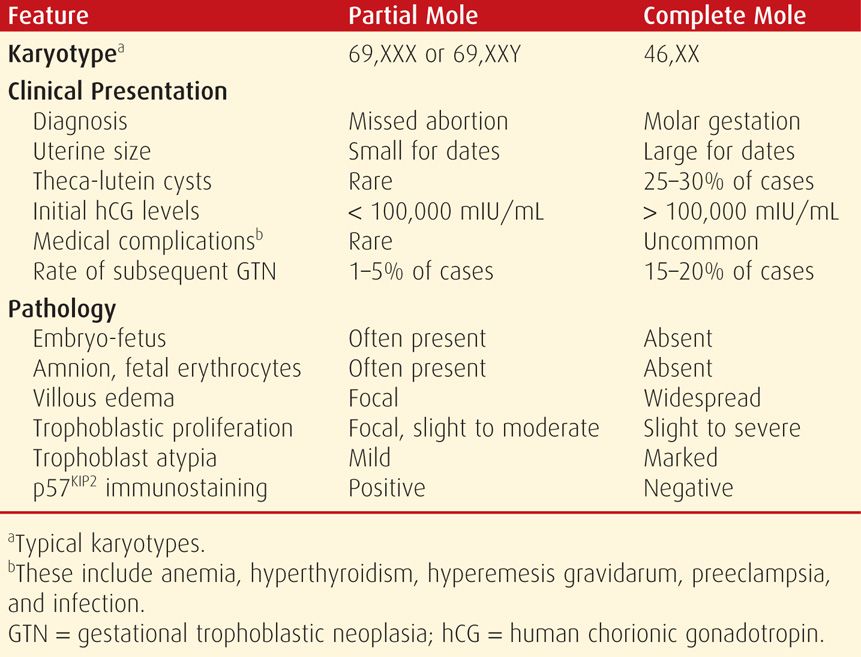
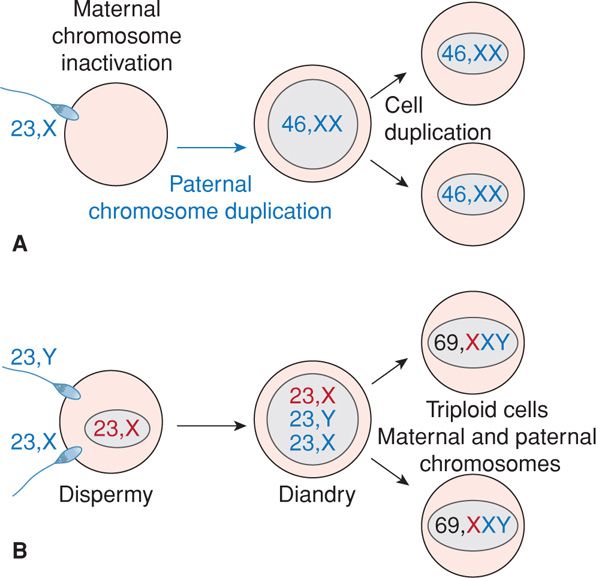
FIGURE 20-2 Typical pathogenesis of complete and partial moles. A. A 46,XX complete mole may be formed if a 23,X-bearing haploid sperm penetrates a 23,X-containing haploid egg whose genes have been “inactivated.” Paternal chromosomes then duplicate to create a 46,XX diploid complement solely of paternal origin. B. A partial mole may be formed if two sperm—either 23,X- or 23,Y-bearing—both fertilize (dispermy) a 23,X-containing haploid egg whose genes have not been inactivated. The resulting fertilized egg is triploid with two chromosome sets being donated by the father (diandry).
Partial moles usually have a triploid karyotype—69,XXX, 69,XXY—or much less commonly, 69,XYY. These are each composed of two paternal haploid sets of chromosomes contributed by dispermy and one maternal haploid set (see Fig. 20-2B). Less frequently, a similar haploid egg may be fertilized by an unreduced diploid 46,XY sperm. These triploid zygotes result in some embryonic development, however, it ultimately is a lethal fetal condition. Fetuses that reach advanced ages have severe growth restriction, multiple congenital anomalies, or both.
Twin Pregnancy Comprised of a Normal Fetus and Coexistent Complete Mole
Rarely, in some twin pregnancies, one chromosomally normal fetus is paired with a complete diploid molar pregnancy. These are recognized in only 1 in 22,000 to 100,000 pregnancies (Steller, 1994). It is important that these cases be distinguished from a single partial molar pregnancy with its abnormal associated fetus. Amniocentesis done for fetal karyotyping is used to confirm the diagnosis.
There are a number of unique pregnancy complications with this twin pregnancy. And, many women may choose to terminate the pregnancy, if diagnosed early. In those with continuing pregnancy, survival of the normal fetus is variable and dependent on complications that commonly develop from the molar component. The most worrisome are preeclampsia or hemorrhage, which frequently necessitate preterm delivery. Wee and Jauniaux (2005) reviewed outcomes in 174 women of whom 82 chose termination. Of the remaining 92 pregnancies, 42 percent either miscarried or had a perinatal death; approximately 60 percent delivered preterm; and only 40 percent delivered at term.
Another concern for those continuing their pregnancy is the possible risk for developing subsequent GTN. Sebire and colleagues (2002b) reviewed such twin pregnancies and reported that in those not terminated, 21 percent of mothers subsequently required chemotherapy. But, this was not significantly different from a rate of 16 percent among women who chose termination. Others have reported rates up to 50 percent following continuation (Massardier, 2009). At this time, most data indicate that women with these twin pregnancies are not at greater risk for subsequent neoplasia than those with a singleton complete mole (Niemann, 2007b). Postdelivery surveillance is conducted as for any molar pregnancy and is discussed on page 401.
 Clinical Findings
Clinical Findings
The clinical presentation of women with a molar pregnancy has changed remarkably over the past several decades because prenatal care is sought much earlier and because sonography is virtually universal. As a result, most molar pregnancies are detected when they are small and before complications ensue (Kerkmeijer, 2009; Mangili, 2008).
Typically, there are usually 1 to 2 months of amenorrhea before discovery. In 41 women with a complete mole diagnosed at a mean of 10 weeks, Gemer and colleagues (2000) reported that 41 percent were asymptomatic and 58 percent had vaginal bleeding. Moreover, only 2 percent had anemia or hyperemesis, and none had other manifestations that in the past were common in these women.
As gestation advances, symptoms generally tend to be more pronounced with complete compared with partial moles (Niemann, 2007a). Untreated molar pregnancies will almost always cause uterine bleeding that varies from spotting to profuse hemorrhage. Bleeding may presage spontaneous molar abortion, but more often, it follows an intermittent course for weeks to months. In more advanced moles with considerable concealed uterine hemorrhage, moderate iron-deficiency anemia develops. Many women have uterine growth that is more rapid than expected. The enlarged uterus has a soft consistency, but typically no fetal heart motion is detected. Nausea and vomiting may become significant. The ovaries contain multiple theca-lutein cysts in 25 to 60 percent of women with a complete mole (Fig. 20-3). These likely result from overstimulation of lutein elements by sometimes massive amounts of hCG. Because theca-lutein cysts regress following pregnancy evacuation, expectant management is preferred. Occasionally a larger cyst may undergo torsion, infarction, and hemorrhage. However, oophorectomy is not performed unless there is extensive infarction that persists after untwisting.
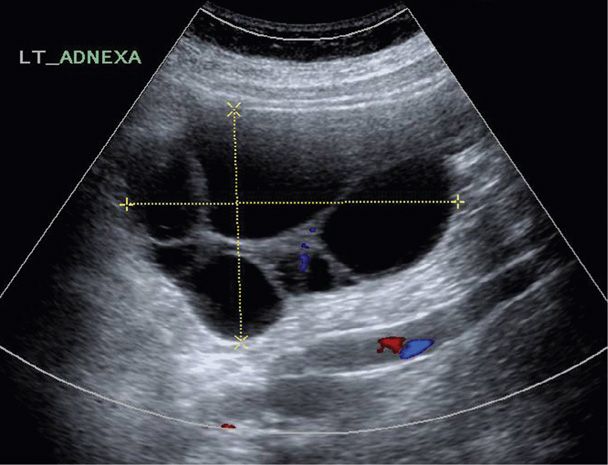
FIGURE 20-3 Sonographic image of an ovary with theca-lutein cysts in a woman with a hydatidiform mole.
The thyrotropin-like effects of hCG frequently cause serum free thyroxine (fT4) levels to be elevated and thyroid-stimulating hormone (TSH) levels to be decreased. Despite this, clinically apparent thyrotoxicosis is unusual and, in our experience, can be mimicked by bleeding and sepsis from infected products. Moreover, the serum free T4 levels rapidly normalize after uterine evacuation. Despite this, a case of presumed “thyroid storm” has been reported (Moskovitz, 2010).
Severe preeclampsia and eclampsia are relatively common with large molar pregnancies. However, these are seldom seen today because of early diagnosis and evacuation. An exception is in the case of a normal fetus coexisting with a complete mole, described earlier. In those cases in which pregnancy is not terminated, severe preeclampsia frequently mandates preterm delivery. The predilection for preeclampsia is explained by the hypoxic trophoblastic mass, which releases antiangiogenic factors that activate endothelial damage (Chap. 40, p. 733).
 Diagnosis
Diagnosis
Most women initially have amenorrhea that is followed by irregular bleeding that almost always prompts pregnancy testing and sonography. Some women will present with spontaneous passage of molar tissue.
Serum β-HCG Measurements
With a complete molar pregnancy, serum β-hCG levels are commonly elevated above those expected for gestational age. With more advanced moles, values in the millions are not unusual. Importantly, these high values can lead to erroneous false-negative urine pregnancy test results because of oversaturation of the test assay by excessive β-hCG hormone (Chap. 9, p. 169). In these cases, serum β-hCG determinations with or without sample dilution will clarify the conundrum. With a partial mole, β-hCG levels may also be significantly elevated, but more commonly concentrations fall into ranges expected for gestational age.
Sonography
Although sonographic imaging is the mainstay of trophoblastic disease diagnosis, not all cases are confirmed initially. Sonographically, a complete mole appears as an echogenic uterine mass with numerous anechoic cystic spaces but without a fetus or amnionic sac. The appearance is often described as a “snowstorm” (Figure 20-4). A partial mole has features that include a thickened, multicystic placenta along with a fetus or at least fetal tissue. In early pregnancy, however, these sonographic characteristics are seen in fewer than half of hydatidiform moles (Fowler, 2006). The most common misdiagnosis is incomplete or missed abortion. Occasionally, molar pregnancy may be confused for a multifetal pregnancy or a uterine leiomyoma with cystic degeneration.
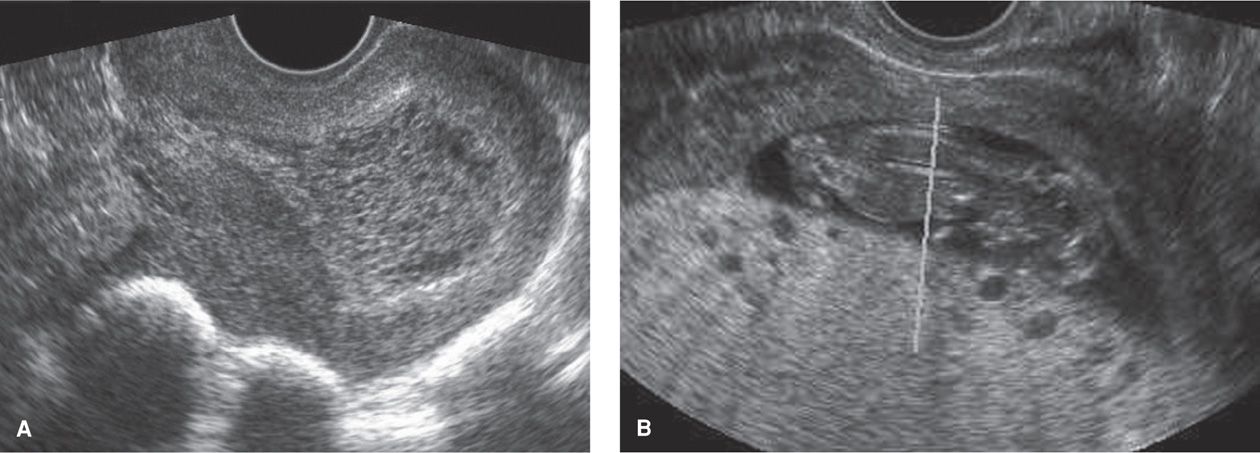
FIGURE 20-4 Sonograms of hydatidiform moles. A. Sagittal view of a uterus with a complete hydatidiform mole. The characteristic “snowstorm” appearance is due to an echogenic uterine mass that has numerous anechoic cystic spaces. Notably, a fetus and amnionic sac are absent. B. In this image of a partial hydatidiform mole, the fetus is seen above a multicystic placenta. (Image contributed by Dr. Elysia Moschos.)
Pathological Diagnosis
Surveillance for subsequent neoplasia following molar pregnancy is crucial. Thus, moles must be histologically distinguished from other types of pregnancy failure that have hydropic placental degeneration, which can mimic molar villous changes. Some distinguishing histological characteristics are shown in Table 20-1.
In pregnancies before 10 weeks, classic molar changes may not be apparent because villi may not be enlarged and molar stroma may not yet be edematous and avascular (Paradinas, 1996). In such situations, other techniques are used to differentiate. One takes advantage of the differing ploidy to distinguish partial (triploid) moles from diploid entities. Complete moles and nonmolar pregnancies with hydropic placental degeneration are both diploid.
Another technique involves histological immunostaining to identify the p57KIP2 nuclear protein. Because the gene that expresses p57KIP2 is paternally imprinted, only maternally donated genes are expressed. Because complete moles contain only paternal genetic material, they cannot express this gene; do not produce p57KIP2; and thus, do not pick up this immunostain. In contrast, this nuclear protein is strongly expressed in partial moles and in nonmolar pregnancies with hydropic change (Castrillon, 2001). As a result, the combined use of ploidy analysis and p57KIP2 immunostaining can be used to differentiate: (1) a complete mole (diploid/p57KIP2-negative), (2) a partial mole (triploid/p57KIP2-positive), and spontaneous abortion with hydropic placental degeneration (diploid/p57KIP2-positive) (Merchant, 2005).
 Management
Management
Maternal deaths from molar pregnancies are rare because of early diagnosis, timely evacuation, and vigilant postevacuation surveillance for GTN. Preoperative evaluation attempts to identify known potential complications such as preeclampsia, hyperthyroidism, anemia, electrolyte depletions from hyperemesis, and metastatic disease (Table 20-2) (Lurain, 2010). Most recommend chest x-ray, whereas computed tomography (CT) and magnetic resonance (MR) imaging are not routinely done unless the chest radiograph shows lung lesions or unless there is evidence of other extrauterine disease such as in the brain or liver.
TABLE 20-2. Some Considerations for Management of Hydatidiform Mole
Preoperative
Laboratory
Hemogram; serum β-hCG, creatinine, and hepatic aminotransferase levels
TSH, free T4 levels
Type and Rh; group and screen or crossmatch
Chest radiograph
Consider hygroscopic dilators
Intraoperative
Large-bore intravenous catheter(s)
Regional or general anesthesia
Oxytocin (Pitocin): 20 units in 1000 mL RL for continuous infusion
One or more other uterotonic agents may be added as needed:
Methylergonovine (Methergine): 0.2 mg = 1 mL = 1 ampule IM every 2 hr prn
Carboprost tromethamine (PGF2α) (Hemabate): 250 μg = 1 mL = 1 ampule IM every 15–90 min prn
Misoprostol (PGE1) (Cytotec): 200 mg tablets for rectal administration, 800–1000 mg once
Karman cannula—size 10 or 12
Consider sonography machine
Postevacuation
Anti-D immune globulin (Rhogam) if Rh D-negative
Initiate effective contraceptiona
Review pathology report
Serum hCG levels: within 48 hours of evacuation, weekly until undetectable, then monthly for 6 months
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


