Effect of Surgery and Anesthesia on Pregnancy Outcome
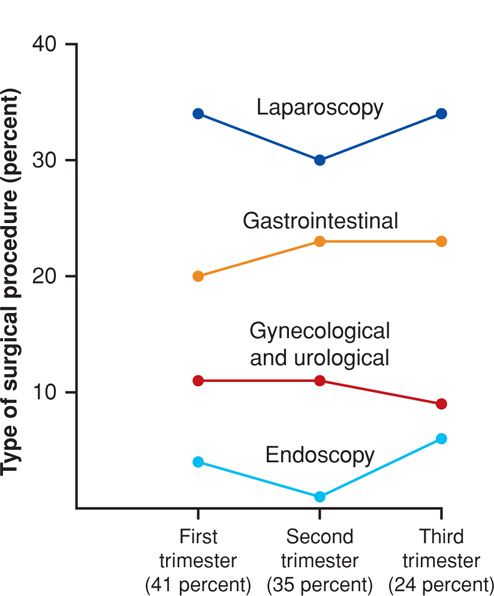
The most extensive data regarding anesthetic and surgical risks to pregnancy are from the Swedish Birth Registry as described by Mazze and Källén (1989). The effects on pregnancy outcomes of 5405 nonobstetrical surgical procedures performed in 720,000 pregnant women from 1973 to 1981 were analyzed. General anesthesia was used for approximately half of these procedures and commonly involved nitrous oxide supplemented by another inhalation agent or intravenous medications. These procedures were performed in 41 percent of women in the first trimester, 35 percent in the second, and 24 percent in the third. The distribution by the type of procedure is shown in Figure 46-1. Overall, 25 percent were abdominal operations and 20 percent were gynecological or urological procedures. Laparoscopy was the most frequently performed operation, and appendectomy was the most common second-trimester procedure.
 Perinatal Outcomes
Perinatal Outcomes
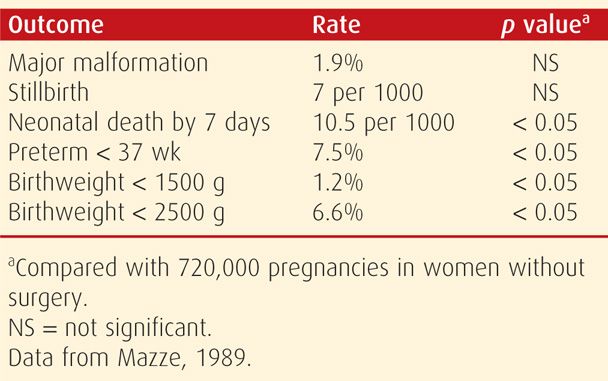
Excessive perinatal morbidity associated with nonobstetrical surgery is attributable in many cases to the disease itself rather than to adverse effects of surgery and anesthesia. The Swedish Birth Registry again provides valuable data as shown in Table 46-1 (Mazze, 1989). The incidence of neonates with congenital malformations or those stillborn was not significantly different from that of nonexposed control newborns. There were, however, significantly increased incidences of low birthweight, preterm birth, and neonatal death in infants born to women who had undergone surgery. Increased neonatal deaths were largely due to preterm birth. These investigators concluded that these adverse outcomes likely were due to a synergistic effect of the illness in concert with the surgical procedures. In another study, there was an increased preterm delivery rate in 235 women undergoing adnexal mass surgery (Hong, 2006).
TABLE 46-1. Birth Outcomes in 5405 Pregnant Women Undergoing Nonobstetrical Surgery
In a follow-up study of the Swedish database, Källén and Mazze (1990) scrutinized 572 operations performed at 4 to 5 weeks’ gestation and reported a nonsignificant relationship with increased neural-tube defect rates. In a similar study from a Hungarian database, Czeizel and colleagues (1998) found no evidence that anesthetic agents were teratogenic. In a review, Kuczkowski (2006) concluded that there is no robust evidence that anesthetic agents are harmful to the fetus.
LAPAROSCOPIC SURGERY DURING PREGNANCY
Laparoscopy has become the most common first-trimester procedure used for diagnosis and management of several surgical disorders (Kuczkowski, 2007). In addition to management of ectopic pregnancy (Chap. 19, p. 385), it is used preferentially during most of pregnancy for exploration and treatment of adnexal masses (Chap. 63, p. 1226), for appendectomy (Chap. 54, p. 1079), and for cholecystectomy (Chap. 55, p. 1096). In 2011, the Guidelines Committee of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) updated its recommendations concerning laparoscopy use in pregnant women. Some of these guidelines are listed in Table 46-2.
TABLE 46-2. Some Guidelines for the Performance of Laparoscopic Surgery in Pregnancy
Indications—same as for nonpregnant women
Adnexal mass excision
Investigation of acute abdominal processes
Appendectomy, cholecystectomy, nephrectomy, adrenalectomy, splenectomy
Timing—all trimesters
Technique
Position: left lateral recumbent
Entry: open technique, careful Veress needle, or optical trocar; fundal height may alter insertion site selection
Trocars: direct visualization for placement; fundal height may alter insertion site selection
CO2 insufflation pressures: 10–15 mm Hg
Monitoring: capnography intraoperatively, FHR assessment pre- and postoperatively
Perioperative pneumatic compression devices and early postoperative ambulation
Information regarding surgical approach selection in pregnant women comes from the American College of Surgeons database (Silvestri, 2011). During the 5-year period ending in 2009, almost 1300 pregnant women who had undergone either appendectomy or cholecystectomy were studied. Open appendectomy was performed in 36 percent of 857 pregnant women compared with only 17 percent of those not pregnant. Of those undergoing cholecystectomy, an open procedure was used in 10 percent of 436 pregnant women compared with 5 percent of nonpregnant women.
There are no randomized trials comparing laparoscopic with open surgery, however, most reviews report equally satisfactory outcomes (Bunyavejchevin, 2013; Fatum, 2001; Lachman, 1999). The most frequently performed procedures were cholecystectomy, adnexal surgery, and appendectomy. Laparoscopic adnexal mass surgery in pregnancy is preferred, and its relative safety is attested to by several investigators (Biscette, 2011; Hoover, 2011; Koo, 2011, 2012). At first, 26 to 28 weeks became the upper gestational-age limit recommended, but as experience has continued to accrue, many now describe laparoscopic surgery performed in the third trimester (Donkervoort, 2011; Kizer, 2011). In one report of 59 pregnant women undergoing laparoscopic cholecystectomy or appendectomy, a third were > 26 weeks pregnant (Rollins, 2004). There were no serious adverse sequelae to these procedures. There are now reports of laparoscopic splenectomy, adrenalectomy, and nephrectomy done in pregnant women (Aubrey-Bassier, 2012; Gernsheimer, 2007; Kosaka, 2006; Miller, 2012; Stroup, 2007).
 Hemodynamic Effects
Hemodynamic Effects
Abdominal insufflation for laparoscopy causes hemodynamic changes that are similar in pregnant and nonpregnant women, and these are summarized in Table 46-3. Reedy and associates (1995) studied baboons at the human equivalent of 22 to 26 weeks’ gestation. There were no substantive physiological changes with 10 mm Hg insufflation pressures, but 20 mm Hg caused significant maternal cardiovascular and respiratory changes after 20 minutes. These included increased respiratory rate, respiratory acidosis, diminished cardiac output, and increased pulmonary artery and capillary wedge pressures.
TABLE 46-3. Physiological Effects of CO2 Insufflation of the Peritoneal Cavity
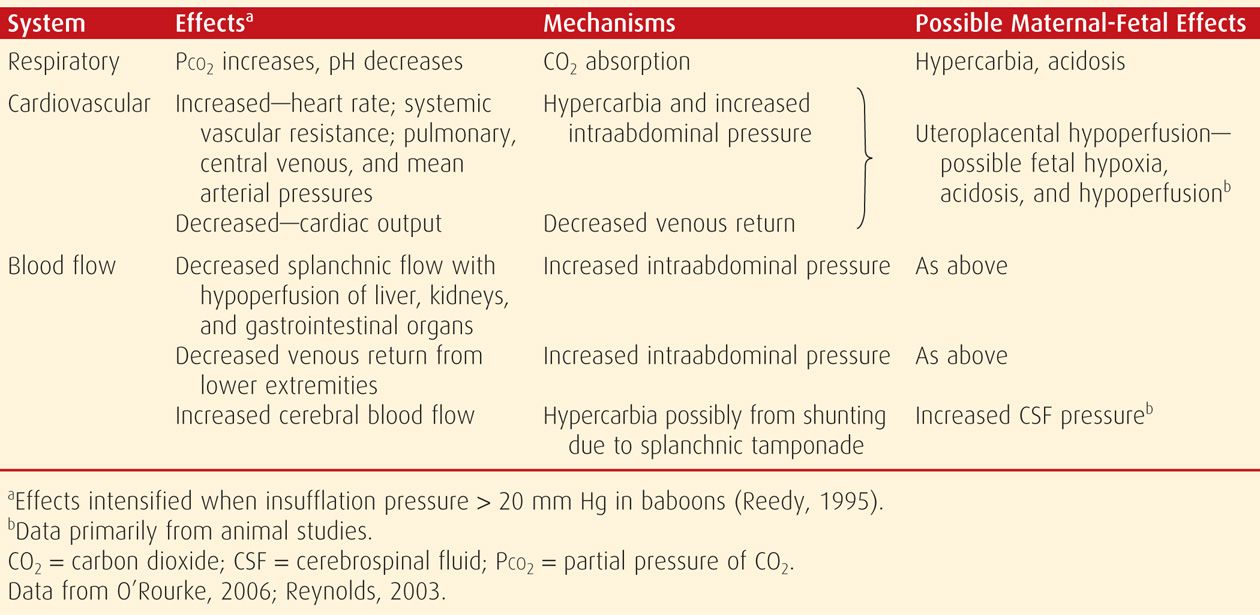
In women, cardiorespiratory changes are generally not severe if insufflation pressures are kept below 20 mm Hg. With noninvasive hemodynamic monitoring in women at midpregnancy, the cardiac index decreased 26 percent by 5 minutes of insufflation and 21 percent by 15 minutes (Steinbrook, 2001). Despite this, mean arterial pressures, systemic vascular resistance, and heart rate did not change significantly.
 Perinatal Outcomes
Perinatal Outcomes
Because precise effects of laparoscopy in the human fetus are unknown, animal studies are informative. In early studies of pregnant ewes, various investigators reported that uteroplacental blood flow decreased when intraperitoneal insufflation pressure exceeded 15 mm Hg (Barnard, 1995; Hunter, 1995). This was the result of decreased perfusion pressure and increased placental vessel resistance (see Table 46-3). The previously cited baboon studies by Reedy and coworkers (1995) produced similar findings. Since then, other studies in sheep have corroborated these observations (O’Rourke, 2006; Reynolds, 2003).
Pregnancy outcomes in women are limited to observations. Reedy and colleagues (1997) used the updated Swedish Birth Registry database to analyze a 20-year period and more than 2 million deliveries. There were 2181 laparoscopic procedures, most of which were performed during the first trimester. Perinatal outcomes for these women were compared with those of all women in the database as well as those undergoing open surgical procedures. These investigators confirmed the earlier findings of an increased risk of low birthweight, preterm delivery, and fetal-growth restriction in pregnancies of women in both operative groups compared with controls. There were no differences, however, when outcomes of women undergoing laparoscopy versus laparotomy were compared. Similar findings were reported from an observational study of 262 women undergoing surgery for an adnexal mass (Koo, 2012).
 Technique
Technique
Preparation for laparoscopy differs little from that used for laparotomy. Bowel cleansing empties the large intestine and may aid visualization. Nasogastric or orogastric decompression reduces the risk of stomach trocar puncture and aspiration. Aortocaval compression is avoided by a left-lateral tilt. Positioning of the lower extremities in boot-type stirrups maintains access to the vagina for fetal sonographic assessment or manual uterine displacement. Vaginally placed instruments that enter the cervix or uterus for uterine manipulation should not be used during pregnancy.
Most reports describe the use of general anesthesia after tracheal intubation with monitoring of end-tidal carbon dioxide—EtCO2 (Hong, 2006; Ribic-Pucelj, 2007). With controlled ventilation, EtCO2 is maintained at 30 to 35 mm Hg.
Beyond the first trimester, technical modifications of standard pelvic laparoscopic entry are required to avoid uterine puncture or laceration. Many recommend open entry techniques to avoid perforations of the uterus, pelvic vessels, and adnexa (Kizer, 2011; Koo, 2012). The abdomen is incised at or above the umbilicus, and the peritoneal cavity entered under direct visualization. At this point, the cannula is then connected to the insufflation system, and a 12-mm Hg pneumoperitoneum is created. The initial insufflation should be conducted slowly to allow for prompt assessment and reversal of any untoward pressure-related effects. Gas leakage around the cannula is managed by tightening the surrounding skin with a towel clamp. Insertion of secondary trocars into the abdomen is most safely performed under direct laparoscopic visual observation through the primary port. Single-port surgery has also been described (Dursun, 2013).
In more advanced pregnancies, direct entry through a left upper quadrant port in the midclavicular line, 2 cm beneath the costal margin, has been described (Donkervoort, 2011; Stepp, 2004). Known as Palmer point, this entry site is used in gynecological laparoscopy because visceroparietal adhesions uncommonly form here (Vilos, 2007).
Gasless Laparoscopy
This is a less commonly used alternative approach that uses a rod with intraabdominal fan-blade-shaped retractors. When opened, these allow the abdominal wall to be lifted upward. It avoids the typical laparoscopic cardiovascular changes because the pneumoperitoneum is created by retraction rather than insufflation (Phupong, 2007).
 Complications
Complications
Risks inherent to any abdominal endoscopy are possibly increased slightly during pregnancy. The obvious unique complication is perforation of the pregnant uterus with either a trocar or Veress needle (Azevedo, 2009; Kizer, 2011). That said, reported complications are infrequent (Fatum, 2001; Joumblat, 2012; Koo, 2012). After a Cochrane database review, it was determined that randomized trials would be necessary to deduce comparative benefits and risks of laparoscopy versus laparotomy during pregnancy (Bunyavejchevin, 2013). Pragmatically, this seems unfeasible, and common sense should dictate the approach used.
IMAGING TECHNIQUES
Imaging modalities that are used as adjuncts for diagnosis and therapy during pregnancy include sonography, radiography, and magnetic resonance (MR) imaging. Of these, radiography is the most problematic. Inevitably, some radiographic procedures are performed before recognition of early pregnancy, usually because of trauma or serious illness. Fortunately, most diagnostic radiographic procedures are associated with minimal fetal risks. As with drugs and medications, however, these procedures may lead to litigation if there is an adverse pregnancy outcome. And x-ray exposure may lead to a needless therapeutic abortion because of patient or physician anxiety.
Beginning 2007, the American College of Radiology (ACR) has addressed the growing concern of radiation dose in all fields of medicine. Some of the goals were to limit exposure through radiation safety practices and promote lifelong accumulated records of exposures in any given patient (Amis, 2007). Task Force recommendations included additional considerations for special radiosensitive populations, such as children and pregnant and potentially pregnant women. The Task Force also suggested that the College should encourage radiologists to record all ionizing radiation times and exposures, compare them with benchmarks, and evaluate outliers as part of ongoing quality assurance programs. At the present time at Parkland Hospital, special recommendations are made for the pregnant woman. Radiation exposure values and duration are recorded in high-exposure areas such as computed tomography (CT) and fluoroscopy. Moreover, quality assurance mechanisms are in place to monitor these parameters.
An excellent review of ionizing radiation exposure during pregnancy was performed following the recent Fukushima nuclear plant disaster in Japan (Groen, 2012). This review reinforced considerations during pregnancy that are discussed subsequently.
 Ionizing Radiation
Ionizing Radiation
The term radiation is poorly understood. Literally, it refers to energy transmission and thus is often applied not only to x-rays, but also to microwaves, ultrasound, diathermy, and radio waves. Of these, x-rays and gamma rays have short wavelengths with very high energy and are ionizing radiation forms. The other four energy forms have rather long wavelengths and low energy (Brent, 1999b, 2009).
The biological effects of x-rays are caused by an electrochemical reaction that can damage tissue. According to Brent (1999a, 2009), x- and gamma-radiation at high doses can create two types of biological effects and reproductive risks in the fetus:
1. Deterministic effects—these may cause congenital malformations, fetal-growth restriction, mental retardation, and abortion. Although controversial, this so-called NOAEL—No Observed Adverse Effect Level—suggests that there is a threshold dose (0.05 gray or 5 rad) below which there is no risk. It also suggests that the threshold for gross fetal malformations is more likely to be 0.2 gray (20 rad).
2. Stochastic effects—these are randomly determined probabilities, which may cause genetic diseases and carcinogenesis. In this case, cancer risk is increased, and hypothetically, at even very low doses.
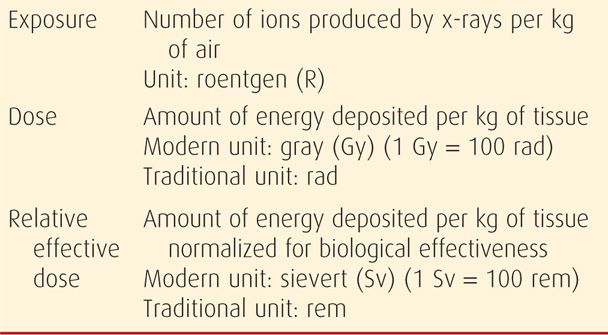
In this sense, ionizing radiation refers to waves or particles—photons—of significant energy that can change the structure of molecules such as those in DNA, or that can create free radicals or ions capable of causing tissue damage (Hall, 1991; National Research Council, 1990). Methods of measuring the effects of x-rays are summarized in Table 46-4. The standard terms used are exposure (in air), dose (to tissue), and relative effective dose (to tissue). In the range of energies for diagnostic x-rays, the dose is now expressed in grays (Gy), and the relative effective dose is now expressed in sieverts (Sv). These can be used interchangeably. For consistency, all doses discussed subsequently are expressed in contemporaneously used units of gray (1 Gy = 100 rad) or sievert (1 Sv = 100 rem). To convert, 1 Sv = 100 rem = 100 rad.
TABLE 46-4. Some Measures of Ionizing Radiation
 X-Ray Dosimetry
X-Ray Dosimetry
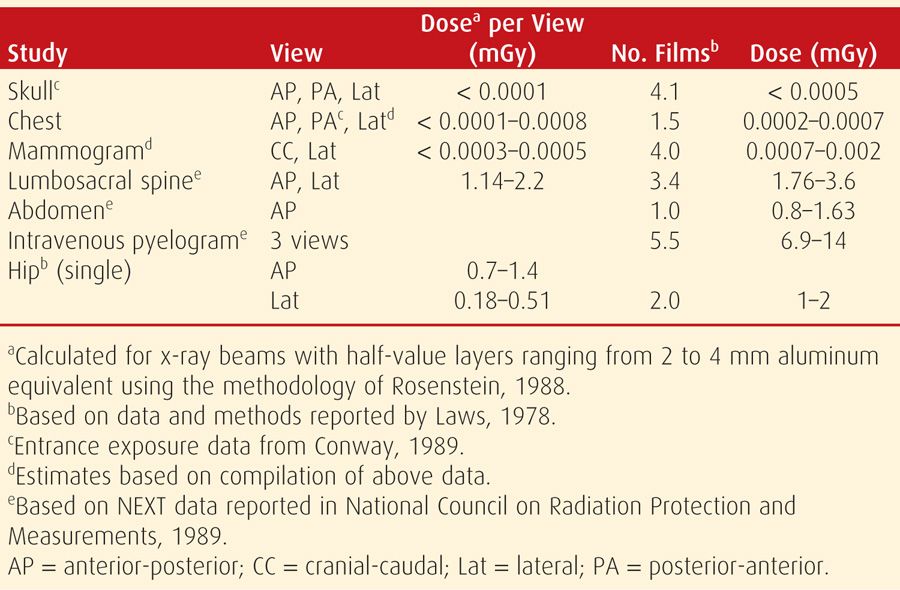
When calculating the ionizing radiation dose, such as that from x-rays, several factors to be considered include: (1) type of study, (2) type and age of equipment, (3) distance of target organ from radiation source, (4) thickness of the body part penetrated, and (5) method or technique used for the study (Wagner, 1997).
Estimates of dose to the uterus and embryo for various frequently used radiographic examinations are summarized in Table 46-5. Studies of maternal body parts farthest from the uterus, such as the head, result in a very small dose of radiation scatter to the embryo or fetus. The size of the woman, radiographic technique, and equipment performance are variable factors. Thus, data in the table serve only as guidelines. When the radiation dose for a specific individual is required, a medical physicist should be consulted. Brent (2009) recommends consulting the Health Physics Society website (www.hps.org) to view some examples of questions and answers posed by patients exposed to radiation.
TABLE 46-5. Dose to the Uterus for Common Radiological Procedures
 Deterministic Effects of Ionizing Radiation
Deterministic Effects of Ionizing Radiation
One potential harmful effect of radiation exposure is deterministic, which may result in abortion, growth restriction, congenital malformations, microcephaly, or mental retardation. These deterministic effects are threshold effects, and the level below which they are induced is the NOAEL (Brent, 2009).
The harmful deterministic effects of ionizing radiation have been extensively studied for cell damage with resultant embryogenesis dysfunction. These have been assessed in animal models, as well as in Japanese atomic bomb survivors and the Oxford Survey of Childhood Cancers (Sorahan, 1995). Additional sources have confirmed previous observations and provided more information (Groen, 2012). One is the 2003 International Commission on Radiological Protection publication, which describes biological fetal effects from prenatal irradiation. Another is the Biological Effects of Ionizing Radiation—BEIR VII Phase 2 report of the National Research Council (2006), which discusses health risks from exposure to low levels of ionizing radiation.
Animal Studies
In the mouse model, the lethality risk is highest during the preimplantation period—up to 10 days postconception. This is likely due to blastomere destruction caused by chromosomal damage (Hall, 1991). The NOAEL for lethality is 0.15 to 0.2 Gy. Genomic instability can be induced in some mouse models at levels of 0.5 Gy (50 rad), which greatly exceeds levels with diagnostic studies (International Commission on Radiological Protection, 2003).
During organogenesis, high-dose radiation—1 gray or 100 rad—is more likely to cause malformations and growth restriction and less likely to have lethal effects in the mouse. Acute low-dose ionizing radiation appears to have no deleterious effects (Howell, 2013). Studies of brain development suggest that there are effects on neuronal development and a window of cortical sensitivity in early and midfetal periods. During this, the threshold ranges from 0.1 to 0.3 Gy or 10 to 30 rad (International Commission on Radiological Protection, 2003).
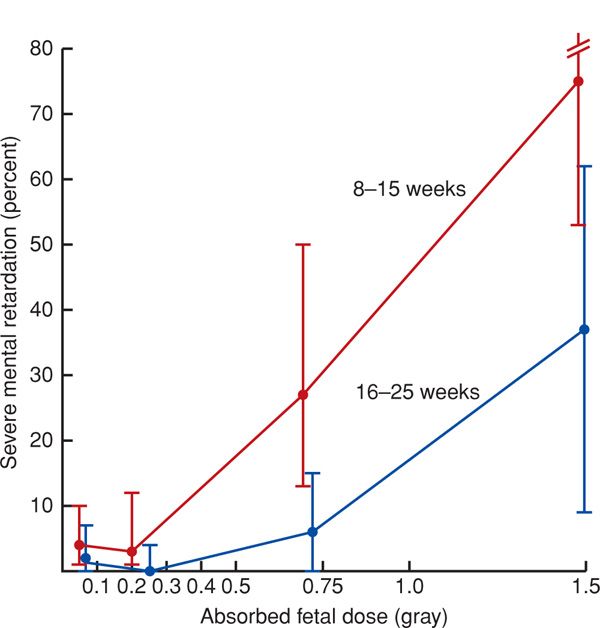
Human Data
Data on adverse human effects of high-dose ionizing radiation have most often been derived from atomic bomb survivors from Hiroshima and Nagasaki (Greskovich, 2000; Otake, 1987). The International Commission on Radiological Protection (2003) confirmed initial studies showing that the increased risk of severe mental retardation was greatest between 8 and 15 weeks (Fig. 46-2). There may be a lower-threshold dose of 0.3 Gy—30 rad—a range similar to the window of cortical sensitivity in the mouse model discussed above. The mean decrease in intelligence quotient (IQ) scores was 25 points per Gy or 100 rad. There appears to be linear dose response, but it is not clear whether there is a threshold dose. Most estimates err on the conservative side by assuming a linear nonthreshold hypothesis. From their review, Strzelczyk and coworkers (2007) conclude that limitations of epidemiological studies at low-level exposures, along with new radiobiological findings, challenge the hypothesis that any amount of radiation causes adverse effects. In one such study describing fetuses exposed to low radiation doses, Choi and colleagues (2012) did not find an increased risk for congenital anomalies.
FIGURE 46-2 Follow-up of subjects from Hiroshima and Nagasaki after the atomic bomb explosion in 1945. Subsequent severe mental retardation caused by exposure to ionizing in utero radiation at two gestational age epochs to 1 Gy, that is, 100 rad. Mean values and 90-percent confidence levels are estimated from dosimetry calculated by two methods—T65DR and D586—used by the Radiation Effects Research Foundation of the Japanese Ministry of Health and National Academy of Sciences of the United States. (Data from Otake, 1987, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree